Basal cell carcinoma (basal cell carcinoma)
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Basal cell carcinoma (synonym: basal cell carcinoma, basal cell epithelioma, ulcus rodens, epithelioma basocellulare) is a common skin tumor with pronounced destructive growth, a tendency to recurrence, as a rule, does not metastasize, and therefore in the domestic literature is more accepted the term "basalioma".
Causes of the basal cell carcinoma
The question of histogenesis is not resolved; most researchers adhere to a dysontogenetic theory of origin, according to which basal cell carcinoma develops from iPS cells. They can differentiate in different directions. In the development of cancer, importance is attached to genetic factors, immune disorders, adverse external influences (intensive insolation, contact with carcinogenic substances). It can develop on clinically unchanged skin, as well as on the background of various skin pathologies (senile keratosis, radiodermatitis, lupus erythematosus, nevi, psoriasis, etc.).
Basalioma is a slowly growing and rarely metastatic basal cell carcinoma that occurs in the epidermis or hair follicles whose cells are similar to the basal cells of the epidermis. It is considered not as a cancer or a benign neoplasm, but as a special kind of tumor with local destructive growth. Sometimes, under the influence of strong carcinogens, primarily X-rays, basalioma enters the basal cell carcinoma. The question of histogenesis is not yet resolved. Some believe that basal cell carcinomas develop from the primary epithelial bud, others from all epithelial structures of the skin, including embryonic buds and malformations.
Risk factors
The provoking factors are insolation, UV, X-rays, burns, arsenic intake. Therefore, basalioma is often found in persons with type I and II of skin and albinos, who are long exposed to intense insolation. It has been established that excessive insolation in childhood can in many years lead to the development of a tumor.
Pathogenesis
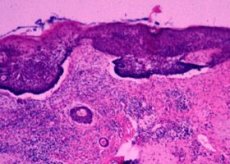
The epidermis is slightly atrophic, sometimes ulcerated, there is a proliferation of tumor basophilic cells, similar to the cells of the basal layer. Anaplasia is less pronounced, there is little mitosis. Basalioma rarely metastasizes, since tumor cells trapped in the bloodstream are not capable of proliferation due to the lack of a growth factor produced by the stromal tumor.
 [18], [19], [20], [21], [22], [23],
[18], [19], [20], [21], [22], [23],
Pathomorphology of basal cell carcinoma
Histologically, basal cell carcinoma is divided into undifferentiated and differentiated. The undifferentiated group includes solid, pigmented, morphe-like and superficial basal cell carcinomas, differentiated - keratotic (with piloid differentiation), cystic and adenoid (with glandular differentiation) and with fatty differentiation.
In the WHO international classification (1996), the following morphological variants of basal cell carcinoma are distinguished: superficial multicentric, codular (solid, adenocystosis), infiltrating, non-sclerotic, sclerosing (desmoplastic, morpho-like), fibro-epithelial; with appendage differentiation - follicular, eccrine, metatypical (basosquamous), keratotic. However, the morphological boundary of all varieties is fuzzy. Thus, in an immature tumor there may be adenoid structures and, on the contrary, with its organoid structure, foci of immature cells are often found. Also, there is no complete correspondence between the clinical and histological pictures. Usually there is a correspondence only in such forms as superficial, fibroepithelial, scleroderma-like and pigment.
For all types of basaliomas, the main histological criterion is the presence of typical complexes of epithelial cells with dark-colored oval nuclei in the central part and located palisade-like along the periphery of the complexes. In appearance, these cells resemble basal epithelial cells, but differ from the latter by the absence of intercellular bridges. Their nuclei are usually monomorphic and not subject to anaplasia. The connective tissue stroma proliferates along with the cellular component of the tumor, located in the form of bundles among the cellular strands, dividing them into lobules. The stroma is rich in glycosaminoglycans, staining metachromatically toluidine blue. It contains many tissue basophils. Retraction gaps often appear between the parenchyma and stroma, which many authors regard as an artifact of fixation, although the probability of exposure to excessive secretion of hyaluronidase is not denied.
Solid basal cell carcinoma among the undifferentiated forms is most common. Histologically, it consists of various shapes and sizes of cords and cells of compactly located basaloid cells with fuzzy boundaries, resembling syncytium. Similar complexes of basal epithelial cells are peripherally surrounded by elongated elements forming a characteristic palisade. Cells in the center of the complexes may undergo dystrophic changes with the formation of cystic cavities. Thus, along with solid structures, cystic structures can exist, forming a solid cystic variant. Sometimes destructive masses in the form of cellular debris are encrusted with calcium salts.
Pigmented basal cell carcinoma is histologically characterized by diffuse pigmentation and due to the presence of melanin in its cells. In the stroma of the tumor there is a large number of melanophages with a high content of melanin granules.
An increased amount of pigment is usually detected in the cystic variant, less often with a solid and superficial multicentric. Basaliomas with pronounced pigmentation contain a lot of melanin in the epithelial cells above the tumor, in its entire thickness down to the stratum corneum.
Superficial basal cell carcinoma is often multiple. Histologically it consists of small, multiple solid complexes associated with the epidermis, as if "suspended" to it, occupies only the upper part of the dermis to the reticular layer. Lymphohistiocytic infiltrates are often found in the stroma. The multiplicity of foci indicates a multicentric genesis of this tumor. Superficial basalioma often recurs after treatment along the periphery of the scar.
Scleroderma-like basal cell carcinoma, or “morphea” type, is distinguished by the abundant development of connective tissue by a scleroderm-like species, in which narrow strands of basal epithelial cells, as it were, are embedded in the dermis, up to the subcutaneous tissue. Polysad structures can be seen only in large strands and cells. Reactive infiltration around tumor complexes located among massive connective tissue stroma is, as a rule, scanty and more pronounced in the zone of active growth in the periphery. Further progression of destructive changes leads to the formation of small (crybroso form) and larger cystic cavities. Sometimes destructive masses in the form of cellular debris are encrusted with calcium salts.
Basal cell carcinoma with glandular differentiation, or adenoid type, is characterized by the presence, in addition to solid areas, of narrow epithelial cords, consisting of several, and sometimes 1-2 rows of cells, forming tubular or alveolar structures. Peripheral epithelial cells of the latter have a cubic form, with the result that the poly-caddis character is absent or less distinct. The inner cells are larger, sometimes with a pronounced cuticle, the cavity of the tubes or alveolar structures are filled with epithelial mucin. A reaction with a carcinoembryonic antigen gives positive extracellular mucin staining on the surface of cells lining the duct-like structures.
Basal cell carcinoma with cyloid differentiation is characterized by the presence of keratinization foci in the complexes of the basal epithelial cells surrounded by cells similar to prickly. Hornification in these cases occurs bypassing the keratohyaline stage, which resembles the keratogenous isthmus zone of normal hair follicles and may have trichoid differentiation. Sometimes there are immature under the follicles with the initial signs of the formation of hair rods. In some embodiments, structures resembling embryonic hair buds are formed, as well as epithelial cells containing glycogen corresponding to the cells of the outer layer of the hair follicle. Sometimes it can be difficult to differentiate with follicular basaloid hamartoma.
Basal cell carcinoma with sebaceous differentiation is rare, characterized by the appearance of foci or individual cells typical of the sebaceous glands among the basal epithelial cells. Some of them are large, cricoid-ringed, with bright cytoplasm and eccentrically located nuclei. When coloring Sudan III they reveal fat. Lipocytes are much less differentiated than in normal sebaceous gland, transitional forms are observed between them and the surrounding basal epithelial cells. This suggests that this type of cancer is histogenetically associated with the sebaceous glands.
The fibroepithelial type (synonym: Pincus fibroepithelioma), a rare type of basal cell carcinoma that occurs most often in the lumbosacral region, can be combined with seborrheic keratosis and superficial basal cell carcinoma. Clinically, it may look like fibropapilloma. Cases of multiple lesions are described.
Histologically, in the dermis, they reveal narrow and long strands of basal epithelial cells, extending from the epidermis, surrounded by a hyperplastic, often edematous mucoid-modified stroma with a large number of fibroblasts. The stroma is rich in capillaries and tissue basophils. Epithelial cords anastomose among themselves, consist of small dark cells with a small amount of cytoplasm and rounded or oval, intensely stained nuclei. Sometimes small cysts filled with homogeneous eosinophilic contents or horn masses are found in such cords.
Neobasocellular syndrome (syn. Gordin-Golts syndrome) is a polyorganotropic, autosomal dominant syndrome related to phacomatosis. It is based on a complex of hyper or neoplastic changes on the basis of violations of embryonic development. A cardinal symptom is the emergence in the early period of life of multiple basaliomas, accompanied by odontotenny cysts of the jaws and anomaly of the ribs. Mot be a cataract and changes in the central nervous system. It is also characterized by frequent changes of the palms and soles in the form of "depressions", in which basaloid structures are also found histologically. After an early nevoid-basalioma phase in a few years, usually in puberty, ulcerative and locally-disrupting forms appear in these areas as an indicator of the onset of the oncological phase.
The histological changes in this syndrome are virtually indistinguishable from the varieties of basaliomas listed above. In the area of the palmar and plantar “depressions” there are defects of the stratum corneum with thinning of its other layers and the appearance of additional epithelial processes from small typical basaloid cells. Large basal cell carcinoma in these places rarely develop. Individual basal cell foci of a linear nature include all variants of organoid basaliomas.
 [24], [25], [26], [27], [28], [29], [30], [31], [32]
[24], [25], [26], [27], [28], [29], [30], [31], [32]
Histogenesis basal cell carcinoma
Basalioma can develop both from epithelial cells and from the epithelium of the pilosebateum complex. On serial sections M. Hundeiker and N. Berger (1968) showed that in 90% of cases the tumor develops from the epidermis. A histochemical study of various types of cancer shows that glycogen, glycosaminoglycans in the stroma of the tumor are found in most cells, especially in adamantinoid and cylindromatous pictures. Glycoproteins are constantly detected in the basement membranes.
Electron microscopy revealed that most cells of tumor complexes contain a standard set of organelles: small mitochondria with a dark matrix and free polyribosomes. At the points of contact, the intercellular bridges are absent, but finger-like outgrowths and a small number of Desmosome-like contacts are found. In places of keratinization, there are layers of cells with intact intercellular bridges and a large number of tonofilaments in the cytoplasm. Occasionally, areas of cells containing cellular membrane complexes are found, which can be interpreted as a manifestation of glandular differentiation. The presence of melanosomes in some cells indicates pigment differentiation. In the basal epithelial cells, organelles characteristic of mature epithelial cells are absent, indicating their immaturity.
Currently, it is believed that this tumor develops from pluripotent germinative epithelial cells under the influence of various external stimuli. Histologically and histochemically, the association of basal cell carcinoma with the anagen stage of hair growth has been proved, and the similarity with the proliferating embryonic hair buds is emphasized. R. Hohlunar (1975) and M. Kumakiri (1978) believe that this tumor develops in the germinal layer of the ectoderm, where immature basal epithelial cells are formed with potency for differentiation.
Symptoms of the basal cell carcinoma
The basalioma of the skin has the appearance of a solitary formation, a hemispherical shape, often rounded, slightly elevated above the skin, pink or grayish-red with a pearly shade, but may not differ from normal skin. The surface of the tumor is smooth, in the center there is usually a slight depression, covered with a thin, loosely adjacent blood-scale crust, which, when removed, usually shows erosion. The edge of the ulcerated element is valiformly thickened, consists of small nodules of whitish color, usually referred to as "pearls" and having diagnostic value. In this state, the tumor may exist for years, slowly increasing.
Bazalioma can be multiple. Primary-plural form, according to K.V. Daniel Beck and A.A. Kolobyakova (1979), is found in 10% of cases, the number of tumor foci can reach several dozen or more, which may be a manifestation of neobasocellular syndrome Gorlin-Goltz.
All the symptoms of skin basal cell carcinoma, including Gorlin-Holtz syndrome, allow us to distinguish the following forms: knotty-ulcerative (ulcus rodens), superficial, scleroderm-like (morpheus), pigment and fibroepithelial. With multiple lesions, these clinical types can be observed in various combinations.
Forms
The surface appearance begins with the appearance of a limited peeling pink stain. Then the spot becomes clear contours, oval, round or irregular shape. Along the edge of the focus, dense, small, glittering nodules appear, which merge together and form a roller-like edge elevated above the skin. The center of the hearth slightly sinks. The color of the hearth becomes dark pink, brown. Lesions may be solitary or multiple. Among the superficial forms, there is a self-piercing or pedzhoidnoy basalioma with a zone of atrophy (or scarring) in the center and a chain of small, dense, opalescent, tumor-like elements along the periphery. Lesions reach a significant amount. Usually has multiple character and persistent flow. Growth is very slow. Clinically, it may resemble Bowen's disease.
In the case of the pigment, the color of the lesion has a bluish, violet or dark brown color. This type is very similar to melanoma, especially nodular, but has a denser consistency. Dermatoscopic examination can provide substantial assistance in such cases.
Tumor appearance is characterized by the appearance of a nodule, which gradually increases in size, reaching 1.5-3 cm or more in diameter, acquires a rounded appearance, a stagnant pink color. The surface of the tumor is smooth with severe telangiectasia, sometimes covered with grayish scales. Sometimes its central part ulcerates and becomes covered with dense crusts. Rarely, the tumor protrudes above the skin level and has a leg (fibroepithelial type). Depending on the size, there are small and large-silken forms.
Ulcerative form occurs as a primary variant or as a result of ulceration of the superficial or tumor forms of the neoplasm. A characteristic feature of the ulcerative form is a funnel-shaped ulceration, which has a massive infiltrate (tumor infiltration) with indistinct borders bound to the underlying tissues. The size of the infiltrate is much larger than the ulcer itself (ulcus rodens). There is a tendency to deep ulceration and destruction of the underlying tissues. Sometimes the ulcerative form is accompanied by papillomatous, warty growths.
The scleroderma-like, or scar-atrophic, type is a small, well-defined lesion with a seal at the base, almost not elevating above the skin, of a yellowish-whitish color. Atrophic changes, dyschromia can be detected in the center. Periodically, around the periphery of an element, foci of erosion of various sizes may occur, covered with an easily detachable crust, which is very important for cytological diagnosis.
Pincus's fibroepithelial tumor is classified as basalioma, although its course is more favorable. Clinically, it manifests itself as a skin-colored nodule or plaque, with a densely elastic consistency, and is practically not subject to erosion.
What do need to examine?
How to examine?
Who to contact?
Treatment of the basal cell carcinoma
Treatment of basal cell carcinoma is the surgical removal of a tumor within healthy skin. In practice, cryodestruction is often used. Radiation therapy is used in cases where the operation leads to a cosmetic defect.
Externally used prospidinovuyu, Kolkhaminovuyu ointment.
More information of the treatment

