New publications
Thoracoplasty
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Thoracoplasty is a surgical method for the treatment of pulmonary tuberculosis and post-resection complications; it is also used to correct deformities of the thorax and spine. It consists in complete or partial removal of several ribs. The scope of the operation depends on the patient's diagnosis and the clinical form of the disease.
In pulmonary tuberculosis therapeutic thoracoplasty is an organ-preserving operation in comparison with lung resection. Ventilation and gas exchange abilities of the lungs remain practically preserved, the volume of the hemithorax is reduced, and the reasons preventing natural healing processes - shriveling and cirrhosis of the lung are eliminated. Although many clinics consider thoracoplasty a backup operation, preferring it to lung resection, in others it is used for treatment of tuberculosis quite widely.
Indications for the procedure
Surgical intervention is shown to patients, firstly, for vital indications - when it is necessary to ensure the normal functioning of internal organs, which before the operation were affected or were in unsuitable conditions - were compressed, distorted, damaged, etc.
Secondly, for a purely cosmetic purpose, to bring the patient's body to an aesthetically acceptable appearance.
- Thoracoplasty for pulmonary tuberculosis is indicated in patients diagnosed with fibrotic cavernous tuberculosis, as well as - cavernous and infiltrative, in cases when drug anti-tuberculosis therapy is ineffective and/or there are contraindications to radical interventions - lung resection. [1]
Curative thoracoplasty is indicated in patients with unilateral chronic fibrotic cavernous pulmonary tuberculosis:
- Persons not older than 50 years of age who have had the disease for no more than two years;
- At the stage of stabilization of the inflammatory process with localization of the cavern in the upper lobe of the lung with a diameter of no more than 5 cm with moderate insemination of other lobes.
- Patients with polychemoresistant form of the disease with predominantly unilateral upper lobe localization of caverns with a diameter of 2-4 cm;
- In addition, patients with slowly progressive bilateral tuberculosis with small to medium-sized caverns.
In complex and advanced cases, patients are indicated for complex operations - thoracoplasty with cavernoplasty, cavernotomy or bronchus ligation. Usually indications for combined operations are characterized by the presence of giant caverns, the size of which covers more than one or two segments of the lung.
Corrective intrapleural thoracoplasty is indicated in patients with caseous necrotic lesions in the remaining parts of the lung after resection. The choice of one-stage or delayed surgery is dictated by additional conditions, such as the duration of pneumonectomy surgery, the amount of blood loss in the patient and so on. Currently, preference is given to delayed thoracoplasty, 2-3 weeks after pneumonectomy, because one-stage combined intervention is characterized by high traumatism.
Indication for additional corrective limited thoracoplasty is undifferentiated interval cavity, in cases when it is impossible to decorticate the lung (Delorme operation); in the so-called "stiff lung"; the presence of immunity to mycobacterial therapy; emphysema and pneumosclerosis of the remaining parts of the lung.
Corrective ectrapleural surgery is indicated to prevent the appearance of residual pleural cavity, because the previously operated lung has partially lost the ability to expand, and in the conditions of repeated resection, such overstretching is not only undesirable, but also unlikely.
- Thoracoplasty in pleural empyema (purulent pleurisy), a condition that often develops after a lung resection, is indicated in the form of thoracomyoplasty. Part of the indications for combined interventions arise already in the course of operations due to visual inspection. In patients with limited pleural empyema, less extensive interventions are indicated. [2], [3]
- Therapeutic thoracoplasty for chest deformities, mainly diagnosed with funnel chest, is certainly indicated in cases where the patient has significant disorders of the vital organs of the cardiovascular system and respiratory organs, i.e. For vital indications. The operation is often performed in childhood and adolescence - the greater the violations, the earlier the surgical intervention is indicated. With deformities that do not interfere with the normal function of internal organs, cosmetic thoracoplasty is performed. Especially often complaints about aesthetic imperfections of the anterior or posterior part of the chest are received from female patients, since the appearance of the body is of great importance for this group of patients, which is also a conditional indication for surgery.
- Similarly, if comprehensive conservative treatment is ineffective, thoracoplasty is also performed for scoliosis of the spine. Surgical treatment is prescribed for patients who have completed the formation of the spine (around 13-16 years of age). The purpose of thoracoplasty for scoliosis is to eliminate abnormalities in the functioning of the thoracic organs, as well as for aesthetic reasons. [4]
Preparation
Preoperative patients are examined comprehensively, which implies the appointment of laboratory, as well as instrumental diagnostic studies.
Basically a series of standardized tests:
- Total blood count;
- Urinalysis;
- Blood Biochemistry;
- Coagulogram to determine blood clotting parameters;
- Tests for dangerous infectious diseases - HIV, syphilis, hepatitis.
Instrumental diagnostics include electrocardiogram, cardiac ultrasound, radiography and/or chest computed tomography, external respiratory function testing (Spirometry or spirography).
On an individual basis, the question of temporary withdrawal of drugs that affect the clotting process, as well as the expediency of taking / withdrawal of other drugs that the patient takes on a regular basis is decided. Drinking and smoking patients are recommended to give up bad habits one month before the intervention.
In addition, patients with pulmonary tuberculosis are prepared for surgery from one week to several months, depending on the severity of intoxication and respiratory dysfunction. The preparation itself consists of anti-tuberculosis drug therapy, which is selected individually for each patient.
Patients with empyema of the pleura are obligatorily assigned to perform sanation of the pleural cavity to remove purulent secretion through its puncture.
The night immediately before surgery, no food or drinks, including water, are recommended after midnight.
The patient enters the operating room having removed eyeglasses, contact lenses, hearing aids, removable dentures, watches, jewelry and religious paraphernalia, removing false nails or removing nail polish from the nails.
Technique of the thoracoplasty
In thoracic surgery, the patient is usually given endotracheal anesthesia and myorelaxants. A flexible tube for intubation anesthesia is inserted into the patient's trachea under intravenous anesthesia to prevent pain. After intubation, the patient is turned over onto the abdomen with the arm on the side of the operation down, resting it on a screw chair or tied with a kerchief to maximize scapular retraction. A roll of the operating table is raised under the second to fourth ribs to make the upper ribs protrude more prominently.
- In this position, a classic open extrapleural thoracoplasty is performed, i.e., without entering the pleural cavity.
In destructive forms of tuberculosis, therapeutic surgery is performed as follows. Above the upper corner of the scapula, slightly above (not more than 1 cm) begin to cut the skin parallel to the spine downward, indenting 6-7 cm wide from the line of spinous processes of thoracic vertebrae. The incision should wrap around the lower corner of the scapula and end at the posterior axillary line.
The first muscle located under the skin layer is the trapezius muscle. The first centimeters of the trapezius muscle should never be cut, so as not to impair the restoration of the arm's motor function and prevent atrophy of the shoulder girdle muscles. Deeper is the muscle that raises the scapula. A high incision involving this neck muscle can lead to torticollis.
It is allowed to dissect the upper part of the broadest muscle of the back, which is done for a more complete withdrawal of the scapula.
To provide operative access to the upper ribs, the small and large rhomboid muscle of the second layer under the trapezius muscle is dissected, then cross the bundles of the upper dentate muscle.
Rib resection is performed from bottom to top, starting with the fourth to fifth rib.
The location of the cavern is important in determining the extent of the operation. If it is located below the level of the clavicle, in the first intercostal space, the upper six to seven ribs are removed; if in the supraclavicular zone, it is usually sufficient to remove four to five upper ribs. Completely, the first, second, and third ribs are usually removed, along with the cartilaginous sections. Removal of the rib heads (except for the first) and apicolysis (separation of the apex of the lung from the fusion) are also mandatory. Failure to comply with these rules leads to the absence of the desired clinical effect.
The most complex complex operations are performed on patients with giant caverns. There is no consensus on the advisability of such intervention and the decision is made by the operating surgeon in each specific case. Such patients undergo extended thoracoplasty with lung invagination in the area of cavern localization and fixation of the invaginated part with sutures; microdrainage of the cavern and fixation of the lung apex up to the eighth rib (A.M. Kiselev's technique). The lowering of the lung apex allows to achieve the onset of good concentric collapse of the cavern. Extended thoracoplasty in combination with cavernoplasty, cavernotomy and bronchus occlusion proved to be effective and recognized as the most acceptable variant of intervention.
These operations are performed in stages to treat patients with bilateral destructive tuberculosis. The first thoracoplasty in such cases is performed on the side of the most affected lung, and after six months, during which the patient adapts after the first stage of surgery, the intervention is performed on the opposite side.
- Corrective intrapleural thoracoplasty (correction of hemithorax, involving the opening of the pleural cavity) is usually performed as a second stage after the main operation two to three weeks later, although in rare cases it can be performed as a one-stage operation. The reasons for its performance are undifferentiated gap between the lobes of the remaining lung, inability to perform Delorme operation for any reason, emphysema and/or pneumosclerosis, resistance to conservative treatment and other indications.
In such cases, an intrapleural thoracoplasty covering two or three ribs is performed. The main condition for performing the operation is to remove the first rib as completely as possible. Basic principles:
- Decoration is performed from the top rib to the bottom rib;
- The removal of the first rib is done under full visual control;
- Decortication is performed according to the shape and size of the hemithorax;
- The necessary correction is achieved by removing half as many ribs as in extrapleural thoracoplasty, i.e., one rib deconstructed internally corresponds to two ribs externally.
The main stage of surgery - lung resection is performed from the anterolateral access.
- Patients diagnosed with chronic purulent pleurisy (empyema) with extensive connective tissue overgrowths can undergo thoracoplasty according to Sheda, developed by him at the end of the XIX century. The operation is traumatic. Therefore, it is performed rarely and when it is impossible to resort to more gentle methods.
The operation starts with an incision at the level of the fourth rib. All ribs up to the second are resected, they are crossed at the cartilage and posterior corner. The empyema cavity is opened in the area of the fistula, making an incision along the gap between the ribs. With the help of an electric suction from the cavity remove purulent contents, tissue decay products, fibrin clots and granulation tissue. From bottom to top, the wall pleura is dissected along with pleural adhesions, periosteum and intercostal muscles. Blood vessels between the ribs are clamped, a ligature is applied to them, the outer wall of the empyema cavity is sutured and removed completely in stages. The cavity itself is treated with antiseptic. The musculoskeletal flap is returned to its place, sutured, two drains are inserted and pressed with a bandage.
Staircase thoracoplasty is considered to be a gentler technique and more common. This is a technique of intrapleural surgery, in which the integrity of the extramural pleura is preserved, because with complete or partial removal of the ribs, the intercostal muscles, previously dissected, are moved to the surface of the remaining lung. Visually, the intercostal muscles resemble the steps of a ladder, whence the name of the operation. Otherwise, this intervention is called Linberg thoracoplasty after the name of the author of the technique.
- In repeated lung resections, extrapleural corrective thoracoplasty is also used as a prophylactic operation to prevent the formation of a residual pleural cavity. The intervention is performed from the posterolateral access. If it is necessary to significantly reduce the volume of the thoracic cavity, the goal of the operation is achieved not so much by the number of ribs removed, but by the length of the removed paravertebral segments. It is important that the volume and shape of the cavity can be modeled "in situ" when performing corrective thoracoplasty.
Since we are talking about the correction of complications, according to modern concepts, delayed intervention is preferable, because in this case the surgical load on the patient's body is not so great. In two to three weeks the inflammatory tuberculosis process does not reactivate significantly, and also such a short rehabilitation period does not lead to an increase in the volume of the second intervention. In the short time that has passed after lung resection, the residual cavity (even if it has formed) will not increase and will be eliminated in the same way as in a one-stage operation, exactly along the same number of ribs, within the boundaries of which it was formed and radiologically determined.
- Thoracoplasties to correct congenital deformities of the thoracic cavity are performed in the vast majority of cases in childhood and adolescence. These are "clean" operations (there is no bacterial insemination), concerning, as a rule, resection of part of the ribs. And although in each specific case a different volume of intervention, the use of different surgical techniques and methods, methods of fixation of the achieved corrections are assumed, the main modern trends are reduced to the increasing use of minimally invasive operations.
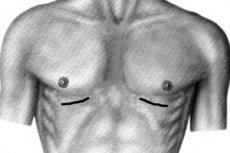
Such an internationally recognized method is the Nass thoracoplasty, a minimally invasive intervention performed through two small incisions in the wall of the sternum on the left and right, under the control of a thoracoscope, an endoscopic instrument that allows the surgeon to observe the actions in the operating field.
Through a skin incision, an intraducer with a braid fixed to it is inserted into the subcutaneous space. It is inserted under the muscles inside the sternum and then behind the sternum in front of the pericardium towards the opposite percutaneous incision. The introduction of the introducer is performed under the control of the thoracoscope. On the other side, the instrument is withdrawn, and a plate made of titanium or inert steel alloy is inserted (usually on the right side) along the formed "trunk". Once it is in place, it is rotated to the desired position. The plate is fixed in thoracoplasty according to Nass with the help of special stabilizers. It is possible to stabilize its position by suturing it to the remaining ribs and intercostal muscles or with the help of Park's fixators, spokes, bone autografts or homografts.
The quality of plate stabilization and the absence of internal bleeding is monitored by repeated thoracoscopy. Only then are sutures placed and the operation is considered complete. The whole process takes approximately 60-70 minutes.
Thoracoplasty, even in the most uncomplicated case, is a very traumatic intervention, so the patient during the entire operation is given a blood transfusion to replenish blood loss. This rule is common to all types of thoracoplasty.
Contraindications to the procedure
Inoperable patients are people with severe mental disorders, i.e. Unable to understand and accept the rules of behavior before, during and after the operation, as well as those suffering from chronic renal, hepatic, cardiac, multi-organ failure that cannot be compensated, i.e. People who simply will not tolerate surgical intervention.
The other contraindications are relative. These are acute diseases and exacerbations of chronic diseases, in women - menstruation period. Surgery is performed after recovery or during remission.
General contraindications to therapeutic thoracoplasty as a stand-alone intervention for pulmonary tuberculosis:
- Polycavernous lung lesions;
- Localization of caverns in the lower lobe;
- Stenosis of large bronchi, bronchiectatic disease, bronchial tuberculosis ²²-²²² degree, widespread purulent endobronchitis;
- Rigid (thick-walled) caverns of any size;
- Multi-organ failure;
- The presence of giant caverns (more than 6 cm);
- Caverns localized in the mediastinal area;
- Disseminated bilateral tuberculosis process;
- Tendency to lobular or central spread of giant caverns with cirrhotic deformation of the sections of the remaining lung parenchyma after resection;
- Recurrent pulmonary bleeding from a cavernous deformed but not collapsed early after surgery.
The treating physician should be alerted to allergies, poor blood clotting, sleep apnea and the use of a breathing apparatus in this regard.
Consequences after the procedure
Accidental injuries to internal organs may occur during thoracoplasty, causing undesirable consequences after the procedure. The most typical intraoperative complications are:
- Traumatic pneumothorax and hemothorax;
- Spinal nerve damage;
- Vagus nerve trauma;
- Damage to the stellate node;
- Bleeding followed by muscle hematomas;
- Incidental cavernous dissection in patients with pulmonary tuberculosis.
Therefore, in order to exclude the above accidents, chest radiography is performed immediately after surgery and both pleural cavities are punctured if necessary.
Complications after the procedure can occur even if the surgery is perfectly performed. All patients suffer from severe pain syndrome after the anesthesia has passed.
Apart from this, the most typical consequences of surgery concerning the wound are bleeding and suppuration.
Regarding the general condition, typical complications may include:
- Pneumonias, both specific and nonspecific;
- Accumulation of sputum in the respiratory tract and, as a consequence, aspiration pneumonia;
- Pulmonary atelectasis;
- Respiratory dysfunction and, as a consequence, the development of dyspnea, hypoxia, changes in acid-base state and blood gas composition;
- Hypovolemia;
- Cardiovascular failure;
- Adverse reactions from the peripheral nervous system - neuritis of the median, radial and ulnar nerves;
- Brachial plexitis;
- Hypodynamia;
- Shoulder drooping on the operated side of the body;
- Impaired motor function of the hand.
After intrapleural thoracoplasty in a patient with pulmonary pathology, the lung may not fuse with the sternal wall. In this case, paradoxical breathing may occur due to the formation of a flotating chest wall.
Care after the procedure
Postoperative management of patients involves a set of preventive measures to prevent the development of complications. Care of patients in pulmonary surgery and those operated on for the elimination of defects of the thorax and spine has both common principles and some differences.
First of all, the common is effective anesthesia. Immediately after surgery, the patient is given epidural anesthesia, its duration can be from three days to a week. Narcotic anesthetics are used for up to 72 hours after thoracoplasty, non-narcotic anesthetics for about a week.
Wound care is carried out. The first two days in the lower corner of the surgical wound (in the open method) is a drain for the outflow of blood from small muscle vessels. The patient is regularly dressed. The last stitches are removed after 8-10 days.
In the postoperative period constantly measure blood pressure, pulse rate, ECG. Constant monitoring of pulmonary ventilation, acid-base and blood gas composition. If necessary, oxygen therapy, cardiotonic therapy, restoration of rheological properties of blood.
Almost immediately after surgery, patients perform breathing exercises, they are prescribed therapeutic exercise. In 10-12 days after the intervention, the patient should begin to raise and lower the arm on the operated side. With a certain persistence of the patient, it is possible to fully restore the function of movement and avoid curvature of the body.
Children and adolescents who have undergone thoracoplasty to correct thoracic or spinal curvatures are placed in bed immediately after surgery on a board in a horizontal position on their backs. In thoracoplasty with thoracic fixation, patients can begin to sit up in bed and walk as early as the second or third day after surgery. If the operation was not accompanied by additional fixation, the rest period is lengthened to three to four weeks, after which the patient begins to sit up in bed.
The absence of sputum retention and free breathing is of great importance for patients operated on for lung pathologies, so the rational position of the body is considered to be semi-sitting, which is provided with the help of special supports. Anesthesia is of great importance not only to improve the general condition of the patient, but also for expectoration of sputum. Patients are afraid to expectorate because of pain, and under anesthesia expectoration is easy and painless. In addition, they are prescribed expectorants and recommended to give twice or thrice a day a glass of warm milk, as well as drink plenty of fluids.
In the early postoperative period, a pressure dressing is applied to the chest in order to avoid paradoxical movements of the deconstructed part of the thorax. It is left until the ossification of the periosteum of the removed ribs.
Patients who have undergone curative thoracoplasty for pulmonary tuberculosis require rather long conservative postoperative treatment. They are treated with intensive polychemotherapy, which makes it possible to achieve effective cure, i.e. Disappearance of the cavern and cessation of bacterial excretion, a year or two after the operation.
