Medical expert of the article
New publications
Pneumosclerosis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Pneumosclerosis is a pathology in the lungs, characterized by the replacement of lung tissue with connective tissue.
This occurs as a result of inflammation, as well as dystrophy of lung tissue, due to which elasticity and gas transport are disrupted in the affected areas. The extracellular matrix, growing in the main respiratory organs, deforms the branches of the windpipe, and the lung itself becomes denser and wrinkles. The result is airlessness, the lungs decrease in size.
Causes pneumosclerosis
Often pneumosclerosis is an accompaniment and outcome of lung diseases:
- Infectious in nature, caused by the entry of foreign substances into the lungs, inflammation of the lung tissue caused by a virus that has not resolved, pulmonary tuberculosis, mycoses;
- Chronic bronchitis, inflammation of the tissue surrounding the bronchi, chronic obstructive pulmonary disease;
- Pneumoconicosis, which occurs after prolonged inhalation of dust and gases, is industrial in origin, caused by radiation;
- Fibrosing and alveolitis caused by the action of an allergen;
- Pulmonary form of Beck's disease;
- The presence of extraneous tessarcoidosis in the branches of the pulmonary throat;
- Injuries resulting from wounds, injuries to the thorax and lungs.
- Hereditary lung diseases.
Ineffective and insufficient treatment of acute and chronic processes in the respiratory organs can lead to the development of pneumosclerosis.
Defects in the blood flow of the pulmonary circulation due to narrowing of the left atrioventricular orifice, left ventricular failure, and pulmonary thrombosis may contribute to the development of pneumosclerosis. This pathology may also be a consequence of ionizing radiation after taking pneumotropic drugs, which are toxic. Weakening of the immune system may also contribute to the development of pneumosclerosis.
If the pulmonary inflammatory process is not completely resolved, the restoration of the lung tissue does not occur completely, connective tissue scars begin to grow, the alveolar lumens narrow, which can provoke the development of pneumosclerosis. Very frequent occurrence of pneumosclerosis has been noted in patients who have had staphylococcal pneumonia, which was accompanied by the formation of necrotic areas of lung tissue and the occurrence of an abscess, after healing of which fibrous tissue growth was noted.
In pneumosclerosis that occurs against the background of tuberculosis, connective tissue may form in the lungs, which may lead to the development of peri-cicatricial emphysema.
A complication of chronic inflammation in the bronchi, such as bronchitis and bronchiolitis, is the occurrence of perilobular and peribronchial pneumosclerosis.
Pleurogenic pneumosclerosis can begin after repeated inflammations of the pleura, in which the superficial layers of the lung join the inflammatory process, and its parenchyma is compressed by exudate.
Radiation and Hamman-Rich syndrome often provoke diffuse pulmonary sclerosis and the development of a honeycomb lung. Left ventricular heart failure and mitral valve stenosis can lead to fluid leakage from blood vessels, which can lead to cardiogenic pneumosclerosis.
Sometimes pneumosclerosis is caused by the mechanism of its development. But the general mechanisms of various forms of etiology are those that are the result of pathology in the ventilation of the lung, defects in the bloodstream, as well as lymph in the lung tissue, failure of the pulmonary drainage capacity. Violation of the structure and alveolar destruction can lead to the replacement of lung tissue with connective tissue. Vascular, bronchial and pulmonary pathology often leads to disruption of lymph circulation, as well as blood circulation, so pneumosclerosis can occur.
Other causes of pneumosclerosis:
- Unresolved acute pneumonia, chronic pneumonia, bronchiectasis.
- Chronic bronchitis, which is accompanied by peribronchitis and leads to the development of peribronchial sclerosis.
- Pneumoconiosis of various origins.
- Congestion in the lungs in a number of heart diseases, and especially in mitral valve defects.
- Atelectasis of the lung.
- Long-term and severe exudative pleurisy, which leads to the development of pneumosclerosis due to the involvement of superficial layers of the lungs in the inflammatory process, as well as in connection with atelectasis, which occurs with prolonged compression of the parenchyma by exudate (pleurogenic cirrhosis).
- Traumatic injury to the chest and lung itself.
- Tuberculosis of the lungs and pleura.
- Treatment with certain medications (cordarone, apressin).
- Systemic connective tissue diseases.
- Idiopathic fibrosing alveolitis.
- Exposure to ionizing radiation.
- Lung damage from chemical warfare agents.
Pathogenesis
The pathogenesis of pneumosclerosis depends on its etiology. However, in all its etiological forms, the most important pathogenetic mechanisms are disorders of pulmonary ventilation, drainage function of the bronchi, blood and lymph circulation. The proliferation of connective tissue is associated with a violation of the structure and destruction of specialized morphofunctional elements of the lung parenchyma. Disorders of blood and lymph circulation that arise during pathological processes in the bronchopulmonary and vascular systems contribute to the development of pneumosclerosis.
A distinction is made between diffuse and focal (local) pneumosclerosis, the latter being large- and small-focal.
Depending on the severity of the proliferation of connective tissue, fibrosis, sclerosis, and cirrhosis of the lungs are distinguished. In pneumofibrosis, cicatricial changes in the lungs are moderately expressed. In pneumosclerosis, a more severe replacement of the lungs with connective tissue occurs. In cirrhosis, complete replacement of the alveoli, as well as partially the bronchi and vessels with disorganized connective tissue is observed. Pneumosclerosis is a symptom or outcome of a number of diseases.
Symptoms pneumosclerosis
The following symptoms of pneumosclerosis are distinguished:
- Signs of the underlying disease leading to pneumosclerosis (chronic bronchitis, chronic pneumonia, bronchiectasis, etc.).
- Shortness of breath with diffuse pneumosclerosis, initially during physical exertion, then at rest; cough with separation of mucopurulent sputum; pronounced diffuse cyanosis.
- Limited mobility of the pulmonary margin, sometimes shortened percussion sound, weakened vesicular breathing with a harsh shade, scattered dry, sometimes fine-bubble rales during auscultation. As a rule, simultaneously with the clinical picture of pneumosclerosis there are symptoms of chronic bronchitis and pulmonary emphysema. Diffuse forms of pneumosclerosis are accompanied by precapillary hypertension of the pulmonary circulation and the development of symptoms of pulmonary heart disease.
- Clinical symptoms of pulmonary cirrhosis: sharp deformation of the chest, partial atrophy of the pectoral muscles, wrinkling of the intercostal spaces, displacement of the trachea, large vessels and heart towards the affected side, dull sound on percussion, sharp weakening of breathing, dry and wet wheezing on auscultation.
Limited pneumosclerosis most often does not cause the patient any sensations, except for a slight cough with a small amount of discharge in the form of sputum. If you examine the affected side, you can find that the thorax in this place has a kind of depression.
The main symptom of diffuse pneumosclerosis is dyspnea: initially during physical activity, later also at rest. The alveolar tissue is poorly ventilated, therefore the skin of such patients is bluish. The patient's fingers resemble drumsticks (Hippocratic finger symptom), which indicates the growth of respiratory failure.
Diffuse pneumosclerosis occurs with chronic inflammation of the branches of the respiratory throat. The patient complains only of a cough - at first rare, which becomes obsessive, strong with abundant purulent discharge. The course of pneumosclerosis is aggravated by the underlying disease: bronchiectatic disease or chronic pneumonia.
Aching pain in the thoracic region and sudden weight loss are possible; such patients look weakened and get tired quickly.
Clinical manifestations of pulmonary cirrhosis may develop: the thorax is grossly deformed, the intercostal muscles are atrophied, the windpipe, heart, and large vessels are displaced toward the affected side.
With diffuse pneumosclerosis, which developed due to a disruption in blood flow in the small bloodstream, symptoms of pulmonary heart disease may be observed.
How severe the course of the disease will be depends on the size of the affected areas.
The percentage of lung tissue already replaced by Pischinger's space is reflected in the following classification of pneumosclerosis:
- Fibrosis, in which limited affected areas of lung tissue appear as cords, alternating with healthy tissue filled with air;
- Sclerosis or pneumosclerosis itself is characterized by the presence of tissues of a denser consistency, connective tissue replaces pulmonary tissue;
- The most severe degree of pneumosclerosis, in which connective tissue completely replaces the lung tissue, and the pleura, alveoli and vessels are compacted, the mediastinal organs are displaced to the side where the affected area is located, is called cirrhosis. Pneumosclerosis is divided into two types according to the degree of prevalence in the lung: diffuse and limited (local), which is distinguished as small-focal and large-focal.
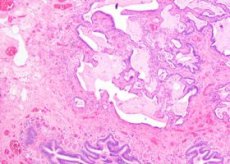
Macroscopically, limited pneumosclerosis has the appearance of denser lung tissue; this part of the lung is distinguished by its sharply reduced size compared to the rest of the healthy areas of the lung. Focal pneumosclerosis has a special form – carnification – postpneumatic sclerosis, characterized by the fact that the pulmonary parenchyma in the inflamed area has the appearance and consistency reminiscent of raw meat. Microscopically, areas of sclerosis and suppuration, fibrinous exudate, fibroatelectasis, etc. can be detected.
Diffuse pneumosclerosis is characterized by spreading to the entire lung or both lungs. The affected organ looks denser, its size is significantly smaller than that of a healthy lung, the structure of the organ differs from healthy tissues.
Limited pneumosclerosis differs from diffuse pneumosclerosis in that the gas exchange function does not suffer significantly, the lung remains elastic. In diffuse pneumosclerosis, the affected lung is rigid, its ventilation is reduced.
Based on the predominant damage to various structures of the lungs, pneumosclerosis can be divided into alveolar, peribronchial, perivascular, interstitial, and perilobular.
According to the causes of occurrence, pneumosclerosis is divided into circulatory, post-necrotic, post-inflammatory and dystrophic.
Where does it hurt?
What's bothering you?
Forms
Pulmonary emphysema and pneumosclerosis
In pulmonary emphysema, there is an increased amount of air in the lung tissue. Pneumosclerosis can be the result of chronic pneumonia, although they are very similar in the clinic. The development of both emphysema and pneumosclerosis is influenced by inflammation of the branches of the windpipe, infection of the bronchial wall, and obstacles to bronchial patency. There is an accumulation of sputum in the small bronchi, ventilation in this area of the lung can provoke the development of both emphysema and pneumosclerosis. Diseases that are accompanied by bronchospasm, for example, bronchial asthma, can accelerate the development of these diseases.
Root pneumosclerosis
Sometimes connective tissue grows in the root areas of the lung. This condition is called root pneumosclerosis. It appears against the background of dystrophic or inflammatory processes, leading to the fact that the affected area loses elasticity, and gas exchange is also disrupted in it.
Local pneumosclerosis
Local or limited pneumosclerosis may not show any clinical signs for a long time, except that harsh breathing and fine-bubble rales are heard during auscultation. It can only be detected radiologically: a section of compacted lung tissue is visible on the image. Local pneumosclerosis practically does not lead to pulmonary insufficiency.
Focal pneumosclerosis
Focal pneumosclerosis can develop due to destruction of the lung parenchyma due to a lung abscess (infectious etiology) or cavities (in tuberculosis). Connective tissue can grow in the place of already healed and still existing foci and cavities.
Apical pneumosclerosis
In apical pneumosclerosis, the lesion is located at the apex of the lung. As a result of inflammatory and destructive processes, the lung tissue at its apex is replaced by connective tissue. At the beginning, the process resembles the phenomena of bronchitis, the consequence of which it most often is, and is determined only radiologically.
 [ 22 ]
[ 22 ]
Age-related pneumosclerosis
Age-related pneumosclerosis is caused by changes that occur due to the aging of the body. Age-related pneumosclerosis develops in old age in the presence of congestive phenomena in pulmonary hypertension, more often in men, especially long-term smokers. If a patient over 80 years of age has pneumosclerosis on an X-ray in the absence of complaints, this is considered normal, since it is a consequence of natural involutional changes in the human body.
Reticular pneumosclerosis
If the volume of connective reticular tissue increases, the lungs lose their clarity and purity, it becomes mesh-like, like a web. Because of this mesh-like quality, the normal pattern is practically invisible, it looks weakened. On a computer tomogram, the compaction of the connective tissue is even more noticeable.
Basal pneumosclerosis
Basal pneumosclerosis is understood as the replacement of connective tissue by pulmonary tissue mainly in its basal sections. Basal pneumosclerosis often indicates previous lower lobe pneumonia. On the X-ray, the clarity of the pulmonary tissues of the basal sections is increased, the pattern is enhanced.
Moderate pneumosclerosis
Connective tissue at the beginning of the development of pneumosclerosis most often grows moderately. The altered lung tissue characteristic of this form alternates with healthy lung parenchyma. This is often revealed only on an X-ray, since it practically does not disturb the patient's condition.
Postpneumonic pneumosclerosis
Postpneumonic pneumosclerosis - carnification is a focus of inflamed lung tissue, which is a complication of pneumonia. The inflamed area looks like raw meat. On macroscopic examination, this is a section of the lung that looks denser, this part of the lung is reduced in size.
Interstitial pneumosclerosis
Interstitial pneumosclerosis is characterized by the fact that the connective tissue mainly captures the interalveolar septa, tissues around the vessels and bronchi. It is a consequence of past interstitial pneumonia.
Peribronchial pneumosclerosis
Peribronchial pneumosclerosis is characterized by localization around the bronchi. Around the affected bronchi, the lung tissue changes to connective tissue. The cause of its occurrence is most often chronic bronchitis. For a long time, the patient is not bothered by anything except coughing, later - with the release of sputum.
Post-tuberculosis pneumosclerosis
In post-tuberculous pneumosclerosis, connective tissue grows as a result of previous pulmonary tuberculosis. This condition can develop into the so-called "post-tuberculous disease", which is characterized by various nosological forms of non-specific diseases, such as, for example, COPD.
Complications and consequences
In pneumosclerosis, morphological changes in the alveoli, bronchi and blood vessels are observed, due to which pneumosclerosis can be complicated by impaired ventilation of the lungs, reduction of the vascular bed, arterial hypoxemia, chronic respiratory failure, pulmonary heart disease can develop, inflammatory diseases of the lungs, and pulmonary emphysema are added.
Diagnostics pneumosclerosis
The radiographic picture is polymorphic, as it reflects the symptoms of both pneumosclerosis and associated diseases: chronic bronchitis, pulmonary emphysema, bronchiectasis, etc. Characteristic features include increased, looped and deformed pulmonary patterns along the bronchial branches due to compaction of the bronchial walls, infiltration and sclerosis of the peribronchial tissue.
Bronchography: convergence or deviation of the bronchi, narrowing and absence of small bronchi, deformation of the walls.
Spirometry: decrease in VC, FVC, Tiffeneau index.
The localization of the pathological process in pneumosclerosis is directly related to the results of physical examinations. Breathing is weakened over the affected area, dry and moist rales are heard, the percussion sound is dull.
A more reliable diagnosis can be made by X-ray examination of the lungs. X-ray is invaluable in detecting changes in the lungs in asymptomatic pneumosclerosis, how widespread these changes are, their nature, and severity. Bronchography, MRI, and CT of the lungs help to more accurately assess the condition of unhealthy areas of lung tissue.
The manifestations of pneumosclerosis cannot be described accurately by X-ray, since they reflect not only the defeat of pneumosclerosis, but also concomitant diseases, such as pulmonary emphysema, bronchiectasis, chronic bronchitis. The affected lung on the X-ray: is reduced in size, the pulmonary pattern along the branches of the bronchi is enhanced, loopy and meshy due to the deformation of the walls of the bronchi, and also due to the fact that the peribronchial tissue is sclerotic and infiltrated. Often the lungs in the lower sections become similar to a porous sponge - "honeycomb lung".
The bronchogram shows convergence and deviation of the bronchi, they are narrowed and deformed, small bronchi cannot be identified.
During bronchoscopy, bronchiectasis and chronic bronchitis are often determined. By analyzing the cellular composition of bronchial lavage, it is possible to clarify the cause of occurrence and the activity of pathological processes occurring in the bronchi.
 [ 31 ]
[ 31 ]
Fluorography in pneumosclerosis
All patients who visit the clinic for the first time are offered to undergo a fluorographic examination of the chest organs. The annual medical examination, which everyone who has reached the age of 14 is required to undergo, involves mandatory fluorography, which helps to identify many respiratory diseases, including pneumosclerosis in the early stages, the course of which is initially asymptomatic.
The vital capacity of the lungs in pneumosclerosis is reduced, the Tiffno index, which is an indicator of bronchial patency, is also low, which is detected using spirometry and peak flowmetry.
Changes in the blood picture in pneumosclerosis are nonspecific.
What do need to examine?
What tests are needed?
Who to contact?
Treatment pneumosclerosis
The main thing in the treatment of pneumosclerosis is the fight against infection in the respiratory organs, improving respiratory function and pulmonary circulation, and strengthening the patient’s immunity.
Patients with pneumosclerosis are treated by a general practitioner or pulmonologist.
Regime and diet
If a patient with pneumosclerosis has a high temperature, he is prescribed bed rest, when the condition improves a little - semi-bed rest, and then - general. The air temperature in the room should be 18-20 °C, ventilation is mandatory. It is recommended to spend more time in the fresh air.
The diet for pneumosclerosis should be aimed at increasing the immunobiological and oxidative processes in the patient's body, accelerating reparation in the lungs, reducing protein loss with sputum, inflammatory exudation, improving hematopoiesis and the functioning of the cardiovascular system. Taking into account the patient's condition, the doctor prescribes diet 11 or 15 tables, the menu of which should include dishes with a normal content of proteins, carbohydrates and fats, but at the same time, increase the amount of products containing calcium, vitamins A, group B, ascorbic acid, potassium salts, folic acid and copper. You need to eat often, in small portions (up to five times). It is recommended to limit the amount of table salt - no more than four to six grams per day, since sodium tends to retain fluid in the body.
Drug treatment of pneumosclerosis
There is no specific treatment for pneumosclerosis. You need to treat the disease that caused the pneumosclerosis.
In case of pneumosclerosis, long-term administration of small doses of glucocorticoids is recommended - up to six to twelve months: twenty to thirty mg per day is prescribed in the acute period, then maintenance therapy, the daily dose of which is five to ten mg, the dose is gradually reduced.
Antibacterial and anti-inflammatory therapy is indicated for bronchiectasis, frequent pneumonia, bronchitis. With pneumosclerosis, about 23 types of different microorganisms can be present in the respiratory tract, it is recommended to use antibiotics and chemotherapeutic drugs of various spectrums of action, combine these drugs, periodically replace them with others. The most common among other antimicrobial drugs in modern medicine for the treatment of pneumosclerosis and other serious pathologies of the respiratory tract are macrolides, the first among which is azithromycin, it should be taken on the first day at 0.5 g, 2-5 days - 0.25 g one hour before or two hours after meals. Cephalosporins of the II-III generation are also popular in the treatment of this disease. For oral administration, among the second generation, cefaclor 750 mg in three doses, cefuroxime axetil 125-500 mg twice a day are recommended; among the third generation cephalosporins, cefixime 400 mg once a day or 200 mg twice a day, cefpodoxime proxetil 400 mg 2 times a day, ceftibuten 200-400 mg per day give a good effect.
A proven antimicrobial drug is metronidazole 0.5 - 1 intravenously by drip for 30-40 minutes every eight hours.
Broad-spectrum antibiotics such as tetracycline, olethetrin and chloramphenicol, 2.0-1.0 g per day in four doses, have not lost their relevance.
For antimicrobial and anti-inflammatory purposes, sulfonamide drugs are prescribed: sulfapyridazine 2.0 mg on the first day, then 1.0 mg for 7-10 days.
Expectorants and thinning agents: bromhexine 0.016 g three to four times a day, ambroxol one tablet (30 mg) three times a day, acetylcysteine - 200 milligrams three times a day, carbocysteine 2 capsules three times a day (1 capsule - 0.375 g carbocysteine)
Bronchospasmolytic agents are used as inhalations (isadrine, euphyllin, atropine sulfate)
If there is circulatory failure, cardiac glycosides are used: strophanthin 0.05% solution - 0.5-1.0 ml per 10-20 ml of 5%-40% glucose or 0.9% sodium chloride, corglycon - 0.5-1.0 ml of 0.6% solution in 5-40% glucose or 0.9% saline.
Vitamin therapy: tocopherol acetate 100-200 mg once or twice a day, ritinol 700-900 mcg per day, ascorbic acid 250 mg once or twice a day, B vitamins (B1 -1.2-2.1 mg per day, B6 - 100-200 mg per day, B12 - 100-200 mg per day)
Physiotherapy for pneumosclerosis
The main goal of physiotherapeutic procedures for pneumosclerosis is to regress and stabilize the process in the active phase, and to achieve relief of the syndrome in the inactive phase.
If there is no suspicion of pulmonary insufficiency, iontophoresis with novocaine, calcium chloride, and ultrasound with novocaine are recommended.
In the compensated stage, it is useful to use diathermy and inductometry in the chest area. If the patient has difficulty separating sputum, electrophoresis with iodine according to the Vermel method is indicated. In case of poor nutrition - general ultraviolet irradiation. Irradiation of the chest with a Sollux lamp daily or every other day is also used, but it is less effective.
Oxygen therapy
A good effect in pneumosclerosis is obtained from oxygen therapy or treatment with oxygen, which is supplied to the lungs in the same volume as it is contained in the atmosphere. This procedure saturates the lungs with oxygen, which improves cellular metabolism.
Surgical treatment of pneumosclerosis
Surgical treatment of pneumosclerosis is performed only in local forms in case of suppuration of the lung parenchyma, destructive changes in the lung tissue, cirrhosis and fibrosis of the lung. This type of treatment involves removing the damaged area of the lung tissue; in rare cases, a decision is made to remove the entire lung.
Physiotherapy
Physiotherapy exercises for pneumosclerosis are used to improve the functions of external respiration, to harden and strengthen the body. In compensated pneumosclerosis, special breathing exercises are used. These exercises should be simple, they must be performed easily, without straining, without slowing down the breath, the tempo should be average or even slow, rhythmically, the load should be gradually increased. It is advisable to perform sports dosed exercises in the fresh air. In case of severe emphysema, as well as cardiopulmonary insufficiency, gymnastics is done in a sitting, lying or standing position, it should last fifteen to twenty minutes. In case of a serious condition of the patient, a temperature exceeding 37.5 ° C, repeated hemoptysis, physiotherapy exercises are contraindicated.
Treatment of pneumosclerosis with folk methods
Traditional medicine suggests treating pneumosclerosis with the following recipes:
- Pour one tablespoon of one of the herbs into a thermos: creeping thyme, blue eucalyptus or oats. Pour in half a liter of boiling water and leave to infuse overnight. In the morning, strain the infusion. Take in small portions throughout the day while hot.
- In the evening, soak thoroughly washed dried fruits in water. In the morning, eat them on an empty stomach. This should be done daily. This recipe has a laxative and diuretic effect, thereby helping to relieve congestion in the lungs.
- Mix two glasses of young red wine + two tablespoons of honey + two crushed leaves of perennial aloe together. First, you need to cut the leaves, rinse under running water, put them in the refrigerator on the bottom shelf for a week. After that, chop them, mix with honey, add wine and mix thoroughly. Infuse for fourteen days in the refrigerator. Take one tablespoon daily up to four times.
Treatment of pneumosclerosis at home
If the patient is treating pneumosclerosis at home, then the main condition for successful treatment here will probably be strict adherence to medical recommendations, as well as monitoring of his condition by a doctor in an outpatient setting. The local therapist or pulmonologist has the right to make corrections in treatment, based on the patient's condition. When treating at home, it is necessary to ensure the exclusion of the factor that provoked or may aggravate the course of pneumosclerosis. Therapeutic measures should be aimed at preventing the spread of infection, as well as the inflammatory process in the lung parenchyma.
Prevention
To prevent pneumosclerosis, it is recommended to be attentive to the condition of the respiratory organs. Treat colds, bronchitis, acute respiratory viral infections and other respiratory pathologies in time.
It is also necessary to strengthen the immune system, take special means to strengthen it - immunomodulators, and harden the body.
Pneumosclerosis is a serious disease characterized by a long course and severe complications. But almost any disease can be cured with timely treatment. Take care of your health, do not endure the disease "on your feet", contact specialists!
Forecast
With timely detection, treatment, compliance with all recommendations, and a healthy lifestyle, the patient can feel normal and lead an active life.
The prognosis for pneumosclerosis is associated with the progression of lung damage and how quickly respiratory and cardiac failure develops.
A poor prognosis for pneumosclerosis may occur with the development of “honeycomb lung” and the addition of a secondary infection.
If a "honeycomb lung" has formed, respiratory failure may be more severe, the pressure in the pulmonary artery increases and pulmonary heart disease may develop. If a secondary infection, tuberculosis, mycosis joins in, a fatal outcome is possible.

