Medical expert of the article
New publications
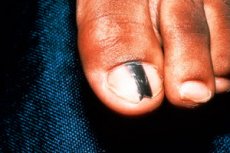
Subnail melanoma: what it looks like, treatment
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Cancer is one of the greatest problems of humanity, which is becoming more and more urgent every year. A tumor can appear anywhere in the human body and, as it develops, spread to large areas by metastasis. Skin cancer (and it also has several types) is one of the most common pathologies in oncological practice. But the primacy in mortality in the first year of the disease is still one of the types of skin cancer - melanoma. True, melanoma is often understood as a tumor of melanocytes on the surface of open areas of the skin, and not everyone suspects that such a neoplasm is possible in the nail area. Dark spots under the nail are often attributed to trauma with hemorrhage (bruise, hematoma), but in fact it may be a malignant formation - subungual melanoma.
Epidemiology
Since cell degeneration occurs when they are damaged, the risk of developing nail melanoma is relatively low. After all, the cells of the nail bed are protected from damage by a dense nail plate. According to statistics, only 0.7-4% of tumor processes on the skin are diagnosed in the nail area.
At the same time, the risk of developing subungual melanoma on the hands or feet is approximately the same, which cannot be said about different fingers of the extremities. The big toe is most susceptible to injury (especially on the feet), so melanoma of this finger is most common. By the way, in 4 out of 10 cases of nail melanoma, patients indicate its injury in the recent past.
Most often, the disease affects adults. After 55-60 years, this indicator is maximum. Subungual melanoma in children is unlikely. Usually, a dark spot in the area of the nail in a child turns out to be a nevus, causing the appearance of a characteristic strip (melanonychia) on its surface.
People with dark skin (African Americans, Indians, Latin Americans, Asians) are most prone to developing subungual melanoma.
In representatives of the dark-skinned race, the disease develops mainly against the background of melanonychia (melanin deposition in the nail plate). Dark-skinned inhabitants of the planet have a tendency to form dark spots on the nail bed and in the nail plate, but often the pathology is not considered as an independent disease, considering it a symptom of other diseases, including subungual melanoma.
 [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
[ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ]
Causes nail melanoma
We have identified several factors that can lead to the degeneration of cells in a certain area of the skin: trauma, UV radiation, pigment nevi, hereditary predisposition. Now we will try to consider the causes of melanoma under the nail in more detail.
Let's start with the fact that when we talk about nevi, we mainly suspect moles or birthmarks. In fact, hemangiomas (a non-malignant vascular tumor that is usually detected immediately after the birth of a child), papillomas (a benign tumor caused by the papillomavirus), and warts (viral neoplasms on the body) also have similar properties. Despite the fact that all such growths are benign, their damage is likely to lead to a change in the properties of the cells and malignancy of the process.
In principle, the cells of any growth on the skin of a finger that has existed for many years without causing much concern to its owner, take the brunt of the impact when injured, and are therefore more damaged than others. At the same time, the risk of developing malignant processes in this case is higher, and it does not matter where this growth formed: on open skin or under the nail plate.
After the age of 40, some people develop separate, shapeless dark spots on their skin that resemble moles. After the age of 50, many people develop such marks, and not just one at a time. This pathology is called seborrheic keratosis ( senile keratosis ), and it is caused by a disruption in the production of keratinocytes in the basal layer of the skin. The neoplasm itself is benign. But over time, it begins to rise higher above the skin and becomes more susceptible to injury. If such a spot appears on the toes, it can be squeezed or rubbed by shoes, suffer from blows, etc., which can lead to cell degeneration. And there are quite a few such cases.
 [ 13 ]
[ 13 ]
Risk factors
Risk factors for the development of subungual melanoma include any previously diagnosed types of skin and connective tissue cancer, as well as a hereditary predisposition to oncological diseases. Even if the cancerous tumor is localized inside the body, it can metastasize to the nail fold, nail base, etc.
When we talked about dark-skinned people, we noted that their predisposition to subungual melanoma is associated with more frequent cases of melanichia. The incidence of this disease in the Caucasian race is less than 1%. But this does not exclude the occurrence of subungual melanoma in people with light skin. Regardless of the localization of the lesion, people with light skin (usually they have light or red hair and blue eyes), the presence of a large number of moles, and freckles on the face are more susceptible to melanoma.
It is clear that the risk of malignant cell degeneration is higher in people who like to sunbathe, especially during hours of increased solar activity, sunbathe in solariums, and work outdoors. As for solar radiation, skin burns received in early childhood often become an oncological problem in adults, sometimes several decades later.
Fingers are the parts of the limbs that are injured very often. But if even in everyday life finger and nail injuries are not a rare occurrence, then what can we say about production conditions, where the bulk of the work is done with hands, or sports with a high risk of toe injuries (for example, football) and the development of melanoma of the big toe, because it is this finger that suffers most often and more than others.
It is clear that without provoking factors no growth on the fingers or under the nail plate will turn into a malignant tumor. But how can we avoid these provoking factors if our living conditions, nutrition, work already pose a risk of injury, poisoning of the body with carcinogenic substances, irradiation with solar UV light. It turns out that the risk of developing subungual melanoma is quite high for each of us living in modern conditions, working in production and having forgotten the taste of natural products. Residents of the village are the winners in this.
Pathogenesis
Melanoma is usually understood as a tumor that develops from human pigment cells (melanocytes). For this reason, in most cases it is easy to diagnose, because the tumor has a darker shade compared to the rest of the skin. However, a fifth of melanomas can be considered atypical cancer (non-pigmented melanoma), because the tumor does not have its characteristic dark shade due to a small number of melanocytes or their absence.
Most often, melanoma affects exposed skin areas. It can be found much less often on mucous membranes, the retina, under the nails. And this is understandable, because any cancer does not arise out of nowhere. And the main provoking factor causing cell degeneration is their trauma, and exposed skin is most susceptible to it.
A cell injury does not necessarily mean a blow. It could just as easily be a "burn" from exposure to sunlight or chemicals.
Any factor causing cell damage can lead to necrotic changes in it with subsequent proliferation and recovery processes. But everything would be fine if it were not for the influence of carcinogenic factors, which are increasing every year. Thus, studies conducted in 1979-2004 showed that over 15 years the number of proven carcinogenic factors increased more than 4 times, and factors with probable carcinogenicity - more than 10 times. It is easy to guess that in the following 13 years these figures increased even more, as did the percentage of skin cancer cases.
There is no need to think that carcinogens are something abstract. They surround us everywhere. But the most dangerous are those that enter the body with food (and the number of products containing carcinogens is constantly growing as industry develops), during cigarette smoking or inhalation of harmful substances while performing work activities in chemical, metallurgical, woodworking and some other industries.
They are considered the most dangerous because their impact on the body is daily and very strong. Someone has to work in hazardous enterprises, the choice of products free of carcinogens is limited, and people try to drown out various experiences by smoking, including those related to work and nutrition. Alcohol, infections, unfavorable environmental conditions, and medications have long since faded into the background, although their influence should not be excluded.
What happens under the influence of carcinogens? Cell damage can occur with changes in DNA, as a result of which the protein structure and functions of cells are disrupted, they degenerate and can become malignant. Carcinogens can delay the process of cell proliferation, i.e. cells continue to divide even when there is no longer a need for this. The proliferation process gets out of control of our body, the tumor continues to grow and spread throughout the body.
At the same time, cancer cells are incredibly tenacious. Not only do they multiply uncontrollably, compressing organs and tissues, disrupting their functioning, but they also begin to secrete toxic substances that have a detrimental effect on healthy cells, including immune system cells, poisoning the body and depleting its strength. By metastasizing, they spread throughout the body and create new tumor foci, putting vital organs out of action.
As for ultraviolet radiation, which is why prolonged sun exposure, tanning in solariums, etc. are considered dangerous, it can also alter cell differentiation under the influence of free radicals.
There is no need to think that cell trauma must necessarily cause cancer. It causes the onset of the proliferative process. But it is precisely at the moment of division that cells are considered especially sensitive to negative effects. The more carcinogens enter the body, the greater the risk of disruption of cell differentiation, changes in their DNA, excessive reproduction beyond the body's control.
There is a certain percentage of people with a hereditary predisposition to cancer. In them, changes in the DNA of cells are genetically determined. And yet, without exposure to provoking factors, the risk of developing melanoma remains low.
Most skin melanomas, including subungual melanoma, are associated with pigmented nevi, which are also not dangerous until they are exposed to damaging factors: trauma and UV radiation. Melanocytes are particularly sensitive cells, so their damage causes not only active proliferation, but also fairly frequent malignancy (degeneration of cells).
Symptoms nail melanoma
Subungual melanoma is a disease that is similar in its symptoms to some other diseases: nail fungus, hematoma after injury, subungual nevus, melanonychia, wart under the nail, paronychia or panaritium (inflammation or formation of pus in the area of the nail fold and the base of the nail). This is what makes the diagnosis of the pathology difficult.
And yet, what should alert a person? What signs may indicate that the appearance of a dark spot and inflammation in the nail area are not simple consequences of an injury, but the beginning of a malignant process? Let's consider the symptoms characteristic of the onset of the disease:
- The first sign of a possible pathology is a change in the color of the nail and tissues under it or around the nail plate. This does not necessarily have to be the entire nail, most often the discoloration is observed on some part of the nail, for example, at its base. In this case, the tissues can be colored burgundy, deep red, brown, purple-black and even blue.
It is clear that darkening of tissues in the nail area is possible due to severe trauma with hemorrhages (bruise). But usually the symptoms of trauma disappear within 10-12 days. If this does not happen, it is worth consulting a doctor and diagnosing the site of injury.
Naturally, if the dark spot was not formed due to injury, it is imperative to examine it.
- If we are talking about a non-pigmented melanoma, then darkening of tissues may not be observed. And there are no painful sensations in the early stages of the disease. For this reason, the non-pigmented form of the disease is usually diagnosed late, when its treatment is already very difficult and rarely brings good results.
But both pigmented and non-pigmented melanoma gradually grows and a longitudinal stripe appears on the nail plate above it. Most often, such a stripe, which has a darker color compared to other tissues, is located strictly in the middle of the nail, but it happens that it is shifted to the right or left from the center of the nail plate. An identical situation is observed with melanonychia.
Over time, the stripe becomes darker and expands. This is different from the stripe on the nail plate caused by hemorrhage due to microtrauma or taking certain medications, which does not change in size over time and shifts as the nail grows. In the dark-skinned race, the appearance of a dark stripe is a certain feature and does not always indicate melanoma.
The melanoma stripe expands until it covers the entire surface of the nail. Sometimes the process spreads to the lateral nail folds, which also change the skin color to a darker color.
- At first, the tumor is not palpable and can only be suspected by a change in the color of the nail tissue, but as it grows, it thickens and begins to press on the nail plate, causing its destruction. The nail exfoliates, becomes brittle, and cracks appear on it. The adhesion to the nail bed decreases. All these signs are very reminiscent of nail fungus.
As the disease progresses, ichor and pus begin to ooze from under the nail bed. The tissues around the nail become inflamed, and abscesses form between the nail plate and the lateral nail folds. From the outside, this looks like a normal inflammation of the periungual fold (paronychia). If suppuration appears in this area, one may suspect panaritium. But in fact, everything can be much more dangerous, because the appearance of pus from under the nail and in the area of adjacent tissues is one of the symptoms of subungual melanoma.
Then, ulcers form at the site of the abscesses, which gradually become larger in size. Attempts to treat the disease with anti-inflammatory and antibacterial ointments do not give results, because we are not talking about an infectious process. Ulcers can fester or ooze, they are quite painful, but do not heal, no matter what measures are taken.
If at first melanoma resembles a small tubercle, then over time it changes its shape to a mushroom-shaped one with a fleshy "cap" and a thinner stalk. This is a characteristic sign of melanoma, although again its similarity to papilloma is visible.
It is important to understand that the malignant process has the ability to spread not only over the surface of the skin, but also inside the tissues. If at the first stage the pain when pressing on the nail is practically not felt, then with the spread of the tumor process to other areas and deep into the bone, pressure on the finger will be accompanied by severe pain. When pus appears under the nail, the pain can be of a constant pulsating nature.
It is clear that inflammation with the formation of pus and dystrophic processes in the nail disrupt the nutrition of the nail plate, as a result of which it separates from the nail bed, on which the malignant process is actively progressing. But now it is no longer hidden from view, and there is no doubt about its nature. However, treatment at this stage of the disease no longer has such encouraging results.
Stages
Symptoms of melanoma may vary slightly depending on the type of pathology and its stage. There is no strict classification by type regarding nail melanoma, but there are:
- melanoma, which develops in the matrix (base) area of the nail, then darkening of the nail in the lunula area is immediately observed,
- melanoma that begins under the nail plate (in this case, the dark spot can appear anywhere on the nail and, as the nail grows, stretch into a colored strip),
- melanoma of the skin near the nail plate (the spot appears on the periphery of the nail, but gradually spreads further).
It is important to understand that all these signs apply to pigmented melanoma. In the non-pigmented form, external manifestations are not observed until the appearance of brittle nails, pus and ulcers. Also, over time, you can feel a lump under the nail.
As for the progression of the disease, the initial stage of subungual melanoma is more reminiscent of a subungual hematoma with the appearance of a dark spot on the nail, which gradually lengthens and grows along with the nail. Other signs are usually not observed.
In the second stage of the disease, the nail is destroyed and purulent inflammation appears. By the end of the second stage, multiple ulcers are observed under the nail plate and next to it, from which ichor oozes. Then the nail peels off.
It is known about the third and fourth stages of subungual melanoma that during this period the process of metastasis occurs. At first, inflammation of regional lymph nodes and their compaction due to the proliferation of malignant cells and individual foci of the tumor process in nearby tissues are observed, subsequently distant metastases appear, affecting the internal organs of a person.
Depending on the route by which malignant cells spread: with the lymph flow or through the blood (lymphogenous and hematogenous route of metastasis), the disease will progress slowly (in the first case) or aggressively, affecting large areas of the body in a short time (when spreading with the blood flow through the blood vessels).
Complications and consequences
A cancerous tumor is a terrible new growth, regardless of where it is found. After all, cancer cells not only multiply excessively, forming seals that compress nearby organs and disrupt their functionality. They also poison the body and destroy healthy cells. Due to their fault, various failures occur in the body, and when it comes to vital organs, the patient dies.
Usually, a fatal outcome is associated with a large tumor size or metastases to the heart, kidneys, lungs. While the tumor is small and has not metastasized, it can be safely removed, but again, everything depends on the prevalence of the process. Sometimes surgeons limit themselves to removing only the nail or distal phalanx of the finger, in other cases, the entire finger has to be removed. If the metastasis process has not been started, one can hope for a favorable outcome of treatment, otherwise malignant foci may subsequently appear in different parts of the body.
If malignant cells spread through the blood, the disease develops very quickly, and by the time it is diagnosed, it may have progressed to the third or fourth stage. At first, a person suspects a nail injury with the formation of a hematoma, then begins to treat the destruction of the nail and abscesses, considering them to be the work of fungi and bacteria, and when the treatment does not give results, he comes to the doctor, who diagnoses an advanced stage of the disease, although perhaps only a couple of months have passed since the first symptoms appeared.
Things are not the best with non-pigmented subungual melanoma. At first, it does not manifest itself in any way, then a light wart appears, lifting the nail. Over time, the wart acquires a specific mushroom-shaped form, and it would be time to think about what it could be. But until it hurts, few people begin to worry about its appearance. When pain appears, it turns out that the process has gone deep inside and affects the bones.
 [ 25 ]
[ 25 ]
Diagnostics nail melanoma
If you carefully study the symptoms of subungual melanoma, you will notice that there are virtually no specific symptoms by which the disease can be diagnosed with great accuracy. The neoplasm at different stages of development will resemble the clinical picture of many other diseases, which significantly complicates the diagnosis. And often it simply delays the moment of contacting a doctor and becomes the reason for delayed treatment without any guarantees.
Based on the appearance of pigmented melanoma, the doctor can only suspect oncology. To confirm the diagnosis, it will be necessary to prescribe a clinical blood test and a blood test for tumor markers. But again, a positive result only indicates the presence of a malignant process in the body and does not provide information about its localization. Perhaps the patient has an ordinary hematoma on the nail, which will be removed by mistake, but this will not save him from a tumor in another place, which no one even suspected.
It is possible to confirm that a dark spot on the nail is melanoma using instrumental diagnostics. Dermatoscopy, of course, comes to the forefront, i.e. examination of the spot under the nail using a special device - a dermatoscope. This modified microscope allows you to see through even the horny layer of the nail plate to detect malignant cells underneath or exclude a cancer diagnosis.
Digital dermatoscopy allows you to obtain an enlarged image of damaged tissue on a computer monitor and take a high-quality photo for further study and consultation.
It is clear that at an early stage, when there are still few malignant cells, dermatoscopy may not detect them, especially if the examination is carried out by a doctor with insufficient experience. The only way to 100% confirm or refute the diagnosis of subungual melanoma is a biopsy, during which a tissue sample is taken from under the nail to a depth of up to 3 mm.
To obtain an informative sample in the area of the dark spot at the base of the nail, you need to make a puncture or remove the nail plate. But it is best to remove not only the nail, but the suspicious neoplasm with adjacent areas of healthy skin. The fact is that a biopsy, i.e. a violation of tumor tissue, can provoke even greater proliferation of cells and tumor growth, which, in addition, can metastasize in a short time. In order not to risk, the biopsy should be taken from a removed area of the nail, which includes the nail plate, muscle tissue under it, subcutaneous fat, and sometimes the entire distal phalanx of the finger, if the process has spread widely.
There is no need to worry about the removed nail and the wound in the nail bed. The wound will heal, and perhaps a new nail will even grow soon. But it is better to remove the hematoma than to ignore the cancerous tumor or disturb it and cause metastasis. At an early stage of the disease, the probability of complete recovery is quite high.
If the biopsy confirms the diagnosis, it is important to understand at what stage the disease was detected and whether the tumor has metastasized. To detect metastases, instrumental diagnostic methods are used again: ultrasound examination, radiography, computed tomography and magnetic resonance imaging. If an increase in regional lymph nodes is observed, a puncture biopsy is mandatory to determine whether the change in the size of the lymphatic vessels is associated with the proliferation of malignant cells inside them.
Differential diagnosis
A high-quality differential diagnosis of dark spots on the nail often allows avoiding unnecessary tissue removal. Subungual melanoma can be confused with melanonychia, subungual hematoma, fungal infection, panaritium, purulent granuloma due to the similarity of external signs and the nature of the lesion. A subungual wart may raise suspicion of a non-pigmented melanoma, and a subungual hematoma - of a pigmented one.
In order to differentiate diseases and exclude incorrect diagnosis, it is very important to study the behavior of the spot or tubercle in the nail area from the patient's words. With melanoma, they will definitely increase in size. Pay attention to the nature of the pain. The appearance of a dark spot that is not associated with trauma and does not cause pain when pressed most likely indicates its malignant nature.
Who to contact?
Treatment nail melanoma
As we have already said, cancer cells have a high survivability, so chemotherapy or radiation without tumor removal can hardly guarantee complete destruction of malignant particles. In addition, in order to accurately diagnose cancer based on biopsy results, it is still more appropriate and safer to first remove the neoplasm. So it turns out that surgical removal of subungual melanoma is the main method of its treatment.
If the tumor is relatively small and has not gone deep inside, the phalanx is sanitized by removing the nail plate and soft tissues underneath it to the depth of tumor penetration, plus some healthy tissue is captured. If the process has spread to the periungual ridges, even part of the finger bundle is removed, but the phalanx is preserved.
In case of deep tumor penetration and metastasis into bone tissue, sanitation as a method of surgical treatment no longer makes sense and it is necessary to resort to amputation of the distal phalanx (less often the finger). In this way, it is possible to prevent the spread of cancer cells by hematogenous route.
If enlarged lymph nodes are detected after a biopsy and confirmation of the presence of cancer cells in them, lymphadenectomy is prescribed, i.e. excision of the lymph node affected by cancer. All this is done in order to block the lymphatic pathway of cancer spread.
Other methods of treating nail melanoma are prescribed only after the tumor has been removed. This includes chemotherapy (drug treatment with potent agents), radiation therapy, which is a dosed irradiation of a certain area of the body in the finger area (if the tumor has metastasized, other areas of the body are also irradiated), taking immunomodulatory vaccines and serums containing antibodies. Immunotherapy is effective for melanoma.
As for chemotherapy, treatment can be carried out with two types of drugs - cytostatics and cytotoxic drugs. The former inhibit cell proliferation and lead to their disintegration (death) due to the inability to divide, the latter lead to intoxication of cancer cells, as a result of which they die.
After removal of a tumor without metastases, local treatment with chemotherapy drugs can be performed (application of ointments, washing the wound with solutions, administration of drugs directly into the tissues of the affected finger). If the metastases have not spread beyond the finger, regional chemotherapy is performed, i.e. drugs are administered directly into the diseased organ. If metastases spread beyond the finger and spread to internal organs, systemic chemotherapy is required (drugs are administered intravenously or orally).
Usually, even such complex and difficult to bear treatment gives good results only in the early stages of the disease. Then it only slightly prolongs the life of patients and requires additional administration of painkillers, since the spread of the malignant process inside is always accompanied by severe pain.
Prevention
Oncologists believe that it is necessary to pay close attention to any changes in the nail after an injury. Such changes should be considered malignant until proven otherwise. This may seem strange to some, but such an attitude to the problem is justified. It is better to be on the safe side than to die because of an untreated bruise that at some point transformed into a cancerous tumor.
It would be better, of course, to avoid limb injuries and limit contact with sunlight, using protective equipment and observing a certain amount of caution. But this is far from always possible. For example, not everyone would give up a sports career just because a finger injury under certain conditions can lead to the formation of subungual melanoma. It is not always possible to avoid domestic injuries or nail damage at work, because other people can cause accidents, no matter how a person protects himself.
Forecast
When talking about cancer treatment, we rarely talk about long-term prognosis, because it is not always possible to completely get rid of cancer cells, and the disease greatly exhausts the body and makes it more susceptible to other diseases, such as infectious diseases, which there is no strength left to fight. Not only the disease weakens the body, but also the chemotherapy or radiation therapy. Sometimes the tumor forms again, but in a different place.
Usually, when making any predictions, they talk about a five-year survival threshold. It is believed that if the patient has not died during this time, i.e. the disease has not returned, there is a chance for a full recovery.
So, at the initial stage of subungual melanoma, the five-year survival rate is 75-88%, which is considered a high figure. The prognosis for the second stage is much worse - about 60-70%. At the third stage, when metastases spread only to the lymph nodes, we can only talk about 40%, and even then there is a high risk of relapse 5 years after surgery with a sluggish course of the process. With damage to internal organs (stage 4), up to 85% of patients die within five years, and only a few cross this threshold.
It turns out that the sooner the patient seeks help, the greater the chances of a full recovery with adequate therapy. This means that you need to pay attention to any changes in the color or shape of the nail, the appearance of new nevi and seals on the fingers, the formation of longitudinal lines on the nail and their behavior. If there is a change in the color of the subungual nevus, an expansion of the strip on the nail and thickening of the nail plate, you must consult a doctor.
The only thing we can do is to carefully monitor our health, be as careful and cautious as possible, regularly examine our bodies for any strange growths, bumps, pigment spots, pay attention to changes in the color and shape of moles, the appearance of dark spots, ulcers, cracks, changes in the shape and thickness of the nail. Only in this case is there a great chance to avoid such a deadly disease as subungual melanoma. Do not think that if the pathology is rare, it will not affect us. Such an attitude to the problem is fraught with great disappointments.

