Medical expert of the article
New publications
Hemarthrosis of the knee.
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The joint parts of the musculoskeletal system have a well-developed vascular network and are well supplied with blood. Therefore, certain injuries, such as trauma, can cause bleeding and blood can accumulate in the joint cavity. This kind of thing happens when hemarthrosis of the knee joint develops. In principle, hemarthrosis can happen in any of the joint cavities, but in trauma practice it is the knee joint that is most often affected. [1]
Epidemiology
The name hemarthrosis is derived from the combination of the Greek words haima - blood + arthron - joint + õsis. The term is used to describe hemorrhage into the joint cavity. According to statistics, it is the knee joint that suffers in most of these situations, as it has a more complex structure, undergoes heavy loads and is supplied with a branched network of blood vessels.
Among athletes, the frequency of hemarthrosis development is about 90%. According to general statistics, the adult population suffers from pathology in 10% of all diseases of the musculoskeletal system.
The most common causes of this disorder - hemarthrosis - are injuries of any severity (dislocations, contusions, fractures, capsular and ligamentous injuries).
In patients with hemophilia or hemorrhagic syndrome, even mild minor trauma can cause the appearance of hemorrhage.
Traumatic hemarthrosis of the knee joint is more often diagnosed in men aged 20 to 49 years, and in women - from 30 to 59 years. At the same time, the rate is significantly higher in representatives of the male population.
At age 16 years and younger, lateral patellar dislocation was the most frequent structural injury associated with traumatic knee hemarthrosis in both boys (39%) and girls (43%); in this age group, the annual incidence of lateral patellar dislocation was 88 per 100,000 and higher in boys (113 per 100,000) than in girls (62 per 100,000). [2]
Causes of the hemarthrosis of the knee joint.
All joints in the body are well supplied with blood, so when blood vessels and tissues are damaged, bleeding often occurs, causing blood to pool in the joint cavity hemarthrosis.
The most etiologically common factor is trauma or pathological non-traumatic processes, such as tumors, dystrophic and degenerative pathologies, infections, etc.
Specific reasons for the development of hemarthrosis can be identified as:
- Fracture of articular bone surfaces, which leads to blood flowing into the joint from damaged bone vessels, or from damaged tissues (joint capsule, cartilage and ligaments, menisci);
- Isolated soft tissue tear (meniscus, capsule, ligament);
- Surgical intervention for meniscus resection, arthroscopic intervention on the ligamentous apparatus (blood may be released from the operated tissues in the early postoperative period, with its accumulation in the joint cavity);
- Vascular damage provoked by degenerative or tumor process;
- Neoplasms: benign synovial hemangiomas, pigmented villonodular synovitis, or any malignant tumor arising near the joint cavity or metastatic. [3], [4]
Posttraumatic hemarthrosis of the knee joint can develop as a result of almost any trauma. Most often it is a bruise of the knee when falling on it, less often - a direct blow, or sports injuries, which are accompanied by tears of ligaments or menisci, intra-articular fractures.
Some accumulation of blood in the form of hemarthrosis is noted after surgical interventions - in particular, after meniscus resection, cross ligament fusion, osteosynthesis of the femoral condyles or tibia.
Patients with hypovitaminosis, hemophilia and hemorrhagic diathesis may suffer from hemarthrosis even with minimal traumatic stress.
Hemarthrosis of the knee joint after knee arthroplasty is relatively rare. Thromboembolic or infectious complications in the area of surgical intervention are more common. [5]
Risk factors
Knee joints are most often damaged during sports activities: it can be hockey, soccer, basketball, skating, skiing, wrestling. The risk group includes professional athletes who spend a lot of time training and are not always careful.
In winter, injuries due to unfavorable weather conditions and skiing or snowboarding become more frequent. These sports involve an increased load on the knee joints as the person descends the mountain on half-bent legs, which is not a natural position for the musculoskeletal system. In such sports it is important to remember to use special protective equipment and to control the load on the knee joints.
Other risk factors for hemarthrosis include:
- Traffic accidents;
- Hypovitaminosis C;
- Hemophilia;
- Hemorrhagic diathesis;
- Childhood and old age;
- Surgical interventions on the joint area.
Pathogenesis
The knee is one of the largest and most complex joints of the human musculoskeletal system. It provides flexion and extension of the lower limb, as well as its mobility in different directions, supports motor coordination and correct body posture.
The rich circulatory system of the knee nourishes the muscles and tissues adjacent to the knee joint and involved in the formation of the joint itself, namely the menisci, cartilage and ligaments. However, it turns out that the presence of a large network of blood vessels becomes a major factor in the formation of hemarthrosis due to peri and intra-articular traumatic injuries.
The basic blood vessels localized in the knee region are located along the posterior surface - under the knee. In this case, both venous and arterial vessels are referred to by anatomists as "hamstring vessels". The artery carries blood from the heart down to the peripheral part of the lower limb, and then the vein carries it back to the heart. In addition to the main vessels, in the knee region there are many branches of smaller caliber, between which there are numerous anastomoses. A powerful blood network provides nutrition to muscle and other tissue structures adjacent to the knee joint. Blood is supplied to the menisci, cartilage, ligamentous apparatus. At the same time, near and intra-articular injuries significantly increase the risk of hemarthrosis. [6]
Symptoms of the hemarthrosis of the knee joint.
Symptomatology with hemarthrosis of the knee joint is different, depending on the degree of pathology.
- Grade 1 is characterized by a small volume of blood accumulated in the joint cavity (no more than 15 ml). The victim indicates the presence of pain in the knee, with a slight increase in axial load. Externally, the knee joint area is unchanged, when probing the presence of fluid is not detected. Directly hemarthrosis is diagnosed in the course of ultrasound examination, after comparing the symptoms with the presence of a history of trauma.
- Grade 2 is characterized by an accumulation of 15 to 100 ml of blood in the cavity. Externally, the knee joint increases in volume. The symptom of "balloting patella" is determined, pressing on the area of the patella leads to its "drowning" among nearby tissues, loose due to fluid accumulation. The patient indicates the presence of shooting pains in the knee, with intensification with load and motor activity. Movement is limited in most cases.
- Grade 3 is characterized by the accumulation of more than 100 ml of blood. The knee area visibly increases in volume, becomes bluish in color due to compression of blood supplying vessels. The patient speaks of severe cramping pain, inability to move. A sharp soreness is noted when loading.
With a small hemorrhage in the form of hemarthrosis, the symptomatology is unexpressed, the signs of pathology are smoothed.
In the case of a meniscus tear or significant soft tissue damage, symptoms such as visual enlargement of the joint are detected externally. The patient notes the appearance of a painful sensation in the articular bag.
The main sign of severe hemarthrosis becomes fluctuation: in the process of pressing on the knee area, a response springiness is noted. Other characteristic symptoms include:
- Shooting intra-articular pain;
- Change in the size and configuration of the knee (roundness, sphericity prevails);
- Inability to fully extend the leg at the knee;
- In case of severe hemorrhage (hemarthrosis) - a feeling of "floating" patella (when squeezing the kneecap it seems to "float" higher, and when tapping the knee there are peculiar shocks).
Local status in hemarthrosis of the knee joint
Hemarthrosis of the right, left knee joint is manifested by the following characteristics:
- The knee is enlarged in volume;
- The contours have been smoothed out;
- There is moderate soreness;
- Pressing the thumbs of two hands on the patella area leads to tingling (balloting of the patella);
- Joint flexion is limited;
- There's a sticky heel symptom.
With hemarthrosis of the 1st degree, a slight swelling, tingling, local temperature increase is noted.
Grade 2 hemarthrosis reveals swelling, pain, and localized fever.
Ligament rupture of the knee joint with hemarthrosis of the 3rd degree is manifested by swelling, severe pain, restriction of movement.
Hemarthrosis of the knee joint in a child
The pathological process accompanied by hemorrhage in the knee joint - hemarthrosis - in childhood can be provoked both by trauma and hemorrhagic hemostasiopathies (hemorrhagic diathesis, hemorrhagic syndrome). Spontaneous joint hemorrhages are noted in children with severe hemophilia. Often the causes are dislocations of the patella, meniscus tears, ligaments, or a fracture received in the process of motor activity or sports activities. More rarely, hemarthrosis is a consequence of vitamin C avitaminosis.
The main symptoms of the pathology of hemarthrosis in childhood are unchanged: there is pain in the knee, swelling, a feeling of swelling and restriction of movement. Only a doctor can establish an accurate diagnosis. Therefore, it is not necessary to delay in time, it is important to go to a trauma center in time and perform radiography.
If the child has hemostasis system diseases due to genetic, congenital or acquired damage to platelets, blood vessel walls or the clotting mechanism, then the child should be registered with a specialist. It is important to inform the doctor as soon as possible about the detected pathological symptoms. Treatment for hemarthrosis in this situation is individualized, with constant monitoring of the blood picture.
Complications and consequences
If untreated, the accumulated blood in the cavity undergoes lysis, a process of protein clotting, which leads to the transformation of the blood fluid into elastic clots that separate from the plasma. Calcification of the clots (hardening) may then occur, making it much more difficult to perform movements in the knee joint.
Lysis can cause the development of intra-articular degenerative disorders: pathological changes occur in cartilage, joint capsule, ligaments. As a result, joint structures wear out quickly, motor activity is severely limited, and arthritis and osteoarthritis may develop.
In addition to complications of hemarthrosis on the orthopedic side, aseptic inflammatory reaction in the knee joint often develops. With an open traumatic injury, hematogenous penetration of infection into the joint cavity, ignoring the rules of asepsis and antisepsis during surgical intervention, purulent inflammation can develop. Spilled blood becomes a perfect environment for many pathogenic organisms: treatment in this case is delayed and becomes more complicated.
To avoid complications, it is important to timely consult a doctor - traumatologist, surgeon, orthopedist. Do not try to cure hemarthrosis of the knee joint on your own: the pathology cannot be treated with folk methods, which in most cases can only aggravate the situation.
Diagnostics of the hemarthrosis of the knee joint.
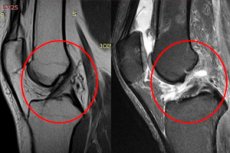
The diagnosis of hemarthrosis of the knee joint is established based on typical clinical symptoms, external manifestations, as well as the results of functional tests (symptom of "balloting patella"). Ultrasound examination is performed to assess the volume of accumulated blood. Patients with fractures, meniscus tears, ligamentous apparatus injuries are shown X-ray of the knee joint, magnetic resonance imaging, computed tomography.
On physical examination, forced position of the lower limb, periosteal edema, hematoma of the surrounding tissues in the knee area may be noticed.
Knee pain may be palpatorily detected. The pain tends to increase during axial load and motor activity.
Laboratory tests of blood and urine demonstrate the absence of pathologic changes. The most commonly prescribed:
- General blood examination. If leukocytosis is noted, it indicates the development of an inflammatory reaction due to the attachment of infection. High COE indicates the presence of pronounced inflammation. A decreased level of hemoglobin and erythrocyte indices against the background of an increase in the level of platelets - a sign of the development of iron deficiency anemia.
- Homeostasis Assessment, coagulogram (to determine blood clotting ability).
Basic instrumental diagnostics is represented by such studies:
- X-ray of the knee joint in two projections (there is no bone pathology, but secondary symptomatology of soft tissue injuries is detected: widening of the joint gap, divergence of the syndesmosis).
- Ultrasound examination (reveals signs of fluid presence, damage to capsule and ligaments, tendon).
- Magnetic resonance imaging (reveals a pattern of damage to the ligament-capsular apparatus and tendons). [7]
Puncture of the knee joint in hemarthrosis carries both diagnostic and therapeutic load: during the procedure, accumulated blood is removed, which is sent for examination. At the same time, drug solutions are injected into the joint cavity, or antiseptic cavity lavage is performed. Puncture allows you to clarify some diagnostic points, eliminate pain syndrome, stop the development of inflammatory reaction. The procedure is carried out in polyclinic conditions with the use of local anesthesia. After completion, the surgeon applies a pressure bandage. After a certain time, the puncture is done again. Treatment can last several weeks, depending on the degree and severity of pathology. [8], [9]
Differential diagnosis
The differential diagnosis is made according to the clinical and radiologic picture:
|
Pathology |
Basis for differentiation |
Diagnosis |
|
Closed knee injury |
Anamnestic information specifying the injury. |
X-ray, MRI shows secondary soft tissue injury. Widened joint gap, visible damage to the capsule and ligaments, tendon. |
|
The acute phase of reactive arthritis |
Complaints of stiffness, stiffness due to severe swelling and fluid accumulation. Active and passive mobility is severely limited. |
X-ray, MRI shows gross degeneration of synovial tissues and cruciate ligaments, cartilage destruction. Osteitis, osteomyelitis may occur. |
|
Acute phase of knee tuberculosis |
Presence of primary tuberculosis focus, positive Mantoux reaction, motor restriction. |
On radiograph, MRI - destructive polymorphic changes of the joint surfaces. |
Who to contact?
Treatment of the hemarthrosis of the knee joint.
Features of treatment for hemarthrosis of the knee joint depend on the degree of the pathological process and the root cause of this violation.
Grade 1 does not require specific therapy and there is no need for instrumental removal of the accumulated blood. The accumulation resolves over several days. Therapeutic measures can be directed only to the elimination and correction of the cause of pathology.
2 and 3 degrees of hemarthrosis require joint puncture - removal of blood from the cavity by means of a puncture (needle). After puncture, the doctor applies an aseptic pressure dressing, and the knee itself is fixed with an orthopedic orthosis or plaster bandage. Cold is applied to the damaged area, and after a few days the knee is examined again and, if necessary, the puncture is repeated.
Additional therapeutic manipulations are prescribed depending on the pathological process that provoked hemarthrosis.
Analgesics are used to relieve pain, but their use must be approved by the attending physician. Any medication containing acetylsalicylic acid is contraindicated because of the risk of worsening bleeding due to altered platelet function.
Strongly potent analgesics (particularly narcotic analgesics) are used only in cases of severe pain and difficult tolerance. Oral hormonal agents are prescribed to inhibit the inflammatory process associated with hemorrhage (the most common drug is prednisolone, which is used at 1-2 mg/kg of weight for 3-4 days).
Nonsteroidal anti-inflammatory drugs are not particularly effective in terms of eliminating the acute inflammatory process in hemarthrosis. Their negative property is the inhibition of platelet function and an increased likelihood of increased bleeding. Nevertheless, their judicious use helps to soothe arthritic pain.
In complex situations, surgical intervention is necessary. [10]
Immobilization in hemarthrosis of the knee joint
Deep, long or short plaster casts are used for knee injuries and hemarthrosis. The short version is more often used, which is suitable for meniscus injuries and partial injuries of the cruciate and collateral ligaments. The cast is applied from the upper third of the thigh to the lower third of the tibia - that is, to the lower edges of the ankle. The application begins with the formation of a posterior plaster cast. After the soft tissue edema subsides, the bandage is converted into a circular plaster cast.
The appropriateness of the use of a bandage is often disputed. For example, some trauma surgeons avoid using a short plaster cast because it is not able to ensure complete immobility of the knee joint, and the ankle area often develops congestion and superficial skin injuries.
A long plaster cast is applied covering the entire injured leg, excluding the pelvic girdle.
Immobilization is performed for 10 days to 10 weeks, depending on the indication.
Surgical treatment
One of the most common and modern surgical methods for diagnosing and treating injuries and diseases of the knee joint is arthroscopy. It is a minimally invasive operation performed through a few skin punctures: the patient can walk the next day.
The surgery is relevant in case of meniscus tears and other meniscus injuries, torn knee joint ligaments, inflammation of the synovial membrane, cartilage pathologies. Often arthroscopy is also used to clarify some diagnostic points - in case of blurred symptoms or ineffectiveness of conservative treatment.
Arthroscopy is performed using a special device called an arthroscope. It is a hollow tube with a diameter of 4 mm: its end segment has special optics and illumination. The device is connected to a video camera, which allows you to display the picture on a monitor screen.
A small incision of about 6 mm is made to insert the arthroscope into the joint. Additional incisions (1, rarely 2) may be necessary to insert surgical instruments.
In most cases of arthroscopy, spinal anesthesia is used. The operation itself lasts about half an hour, sometimes longer (for example, if meniscus stitching is required). Often the patient is allowed to lean on the leg as early as 12 hours after the intervention. Sometimes an orthosis may be required. In general, the load is increased gradually over a month. The rehabilitation scheme is determined individually.
Treatment timeframe
In most patients with traumatic knee hemarthrosis, joint function is restored within 3-4 weeks with adequate therapy. In this case, a small hemarthrosis may not require prolonged immobilization: the use of elastic bandages, splints or supportive dressings is recommended. Application of cold (ice) is also indicated.
Prolonged rest, compliance with bed rest is a necessary condition for the elimination of acute signs of the disorder. But the rest period should not be prolonged for a long time, as the risk of formation of motor limitations and muscle atrophy increases. To prevent this, recovery procedures for the knee should be started as soon as possible: at the first stage, it is preferable to practice isometric exercises. After the elimination of acute symptoms, it is allowed to begin exercises with a gradual increase in motor amplitude. The timing of the start of a particular rehabilitation phase is agreed with the attending physician.
Recovery and rehabilitation
After removal of the bandage or plaster cast, rehabilitation treatment is mandatory. Patients are shown a course of physiotherapy: shock-wave therapy is considered particularly useful - a modern method based on the impact of shock (acoustic) oscillations. Facing the tissues, there is a release of wave energy, thanks to which the necessary biological effect: pain is reduced, inflammation is reduced, restores mobility of the knee joint, accelerates regenerative reactions, improves microcirculation. Every second patient notes improvement after the first treatment session. Contraindications to shockwave therapy are considered:
- Tumors in the area of the procedure;
- Vascular thrombosis, regardless of its localization;
- Acute infections;
- Diseases accompanied by disorders of blood coagulation;
- During pregnancy;
- Arrhythmias;
- Dermatologic pathologies in the area of the procedure.
Additionally prescribe a course of therapeutic exercise - to restore an adequate degree of mobility in the bursa of the joint.
The duration of the rehabilitation period is individual and depends on the degree of hemorrhage, its causes, as well as on the timeliness of seeking medical help.
Prevention
Active sports, injuries and other stresses adversely affect the condition of all joints, and knees in particular. To prevent traumatic injuries with further development of hemarthrosis, it is important to adhere to simple rules, which represent the prevention of such problems.
Of course, in most cases, injuries happen suddenly, and no one is immune to them. However, an important rule for athletes is that you should always consult a sports doctor, who will identify "weaknesses" in various muscle groups, assess the general condition of the body and advise you on how to prevent possible problems.
What can be done to mitigate the likely risks?
- You should not start a workout without first warming up and muscle warming up.
- If you feel very tired, it is important to take a break or end your workout, as strained muscles and joints are more susceptible to all kinds of injuries.
- Intensive sports activities require a sufficient intake of nutrients and vitamins into the body. Therefore, the diet should be as complete and balanced as possible, and if necessary, additional vitamin and mineral preparations should be taken.
- And during sports, and in any other situations, you should wear the most comfortable shoes, matched to the size and type of activity, made of quality materials.
If an injury does occur, you should immediately visit a specialist. It is not worth delaying the visit, as the disorder can complicate, and a minor hemarthrosis of the knee joint will develop into a more serious problem.
Forecast
If there is excessive intra-articular accumulation of blood, the risk of circulatory disturbances increases. This can cause the formation of painful dystrophic disorders, as in the case of true degenerative arthrosis. The risks of developing such a complication increase if hemarthrosis of the knee joint occurs repeatedly. Therefore, it is worth being attentive to your health and prevent the reappearance of the pathology of hemarthrosis.
In addition, due to intra-articular accumulation of blood, there is a natural decay of hemoglobin and plasma elements: they settle on the capsule and hyaline cartilage, which adversely affects the structure of the knee joint, worsens elasticity.
If untreated, the tissues accumulate hemosiderin, a pigmented substance formed during the breakdown of blood cells. This leads to focal destruction with gradual cartilage damage. At the same time, destructive arthrosis develops: the patient loses the ability to move the knee, there is stiffness and constant pain syndrome. Hemarthrosis may further transform into coxarthrosis.
The prognosis also worsens if synovitis develops - an inflammatory reaction affecting the synovial membrane. If the problem is not treated in time, purulent arthritis develops, requiring intensive antibiotic therapy.
In most cases, provided that medical attention is sought in a timely manner, the prognosis can be considered favorable. Full recovery is noted over several weeks or months.
Army
There is no single answer to the question of whether patients with hemarthrosis of the knee can perform military service. Deferment or exemption from military service is possible:
- For severe knee dysfunction;
- In persistent contracture with severe motor restriction;
- When the limb axis is severely deformed;
- In the presence of an artificial knee joint;
- In patellar instability with frequent dislocations, instability of the knee joint of the second or third degree.
The presence of pathology that prevents the passage of military service must be confirmed by frequent visits to the doctor and episodes of inpatient treatment, certified by radiographs (ultrasound, MRI).
After successful surgical intervention, there should be a report of a deferral with further possible exemption from formation, physical training.
The exact possibilities of service, eligibility for conscription is determined by a specialist of the medical and military expertise after careful study of the medical history and general state of health of the conscript. Hemarthrosis of the knee joint itself does not have a certain category of eligibility: the question is decided individually.

