Medical expert of the article
New publications
Knee joint
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The knee joint (art. genus) is the largest and most complex in structure. It is formed by the femur, tibia and patella. The articular surfaces of the medial and lateral condyles of the femur articulate with the superior articular surface of the tibia and patella. Inside the joint there are crescent-shaped intra-articular cartilages - the lateral and medial menisci, which increase the congruence of the articulating surfaces and also perform a shock-absorbing role.
The lateral meniscus (meniscus lateralis) is wider than the medial meniscus (meniscus medialis). The lateral edge of the meniscus is fused with the joint capsule. The inner thinned edge of the meniscus is free. The anterior and posterior ends of the meniscus are attached to the intercondylar eminence of the tibia. The anterior ends of the meniscus are connected by the transverse ligament of the knee (lig. transversum genus).
Read also: |
The joint capsule of the knee joint is thin. On the femur it is attached approximately 1 cm from the edges of the articular surfaces, on the tibia and patella - along the edges of the articular surfaces. The synovial membrane forms several folds containing fatty tissue. The largest paired pterygoid folds (plicae alares) are located on the sides of the patella. From the patella to the anterior intercondylar field, an unpaired infrapatellar synovial fold (plica synovialis infrapatellaris) runs vertically downwards.

Ligaments of the knee joint
The knee joint is strengthened by ligaments. The fibular collateral ligament (lig. collaterale fibulare) is extracapsular, runs from the lateral epicondyle of the femur to the lateral surface of the head of the fibula. The tibial collateral ligament (lig. collaterale tibiale), fused with the capsule, begins on the medial epicondyle of the femur and is attached to the upper part of the medial edge of the tibia. On the posterior surface of the joint is the oblique popliteal ligament (lig. popliteum obliquum), which is the terminal bundle of the tendon of the semimembranosus muscle. This ligament is woven into the posterior wall of the joint capsule and is also attached to the posterior surface of the medial condyle of the tibia.
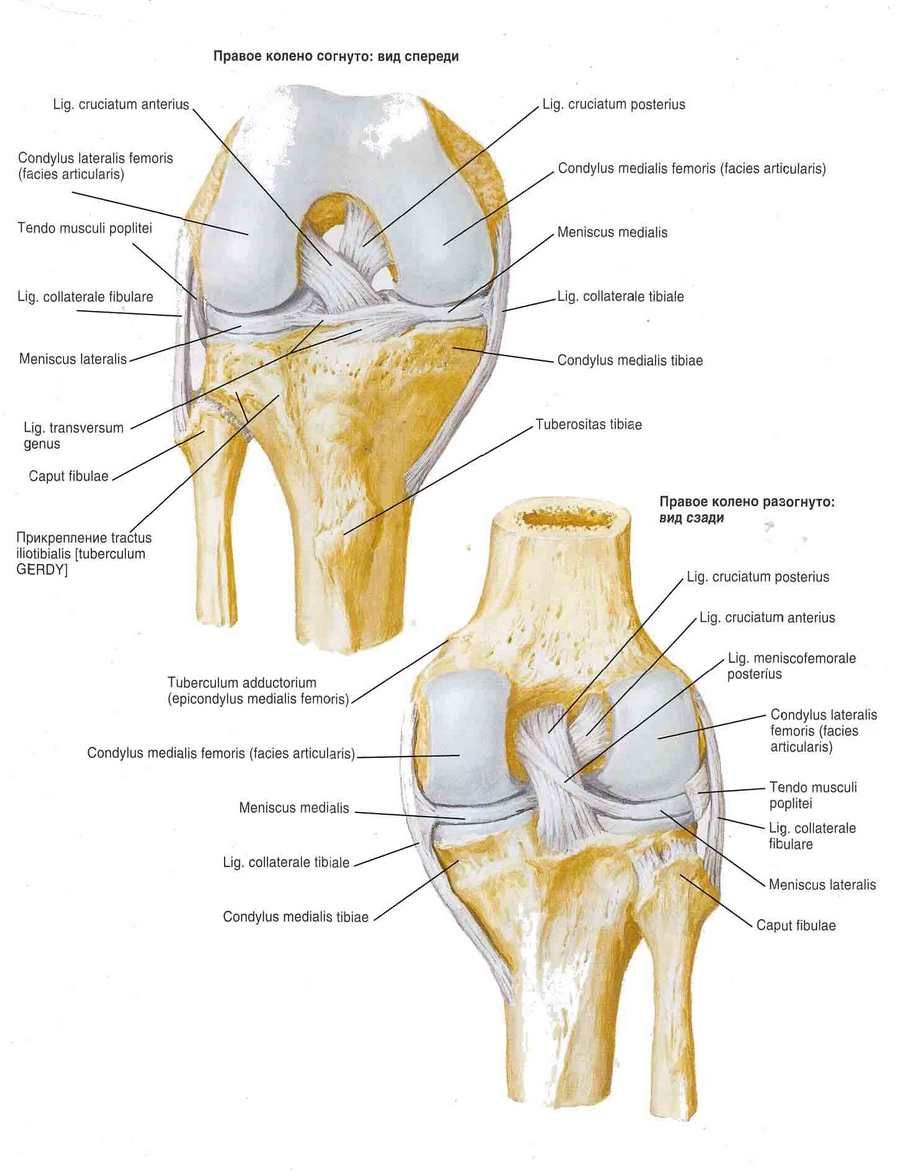
The arcuate popliteal ligament (lig. popliteum arcuatum) originates on the posterior surface of the head of the fibula, curves medially and attaches to the posterior surface of the tibia. In front, the joint capsule is reinforced by the tendon of the quadriceps femoris, which is called the patellar ligament (lig. patellae). The internal and external bundles of the quadriceps femoris tendon, running from the patella to the medial and lateral epicondyles of the femur and to the condyles of the tibia, are called the medial and lateral supporting ligaments of the patella (retinaculum patellae mediate et laterale).
The knee joint cavity contains cruciate ligaments covered with a synovial membrane. The anterior cruciate ligament (lig. cruciatum anterius) begins on the medial surface of the lateral femoral condyle and attaches to the anterior intercondylar field of the tibia. The posterior cruciate ligament (lig. cruciatum posterius) is stretched between the lateral surface of the medial femoral condyle and the posterior intercondylar field of the tibia.
Synovial membrane of the knee joint
The knee joint has several synovial sacs. Their number and size vary individually. The synovial sacs are located mainly between the tendons and under them near the point of attachment of the tendons to the bones. The suprapatellar bursa (bursa suprapatellaris) is located between the tendon of the quadriceps femoris and the femur. The deep infrapatellar bursa (bursa infrapatellaris profunda) is located between the patellar ligament and the tibia. The subtendinous bursa of the sartorius muscle (bursa subtendmea m. sartorii) is located near the point of attachment of its tendon to the tibia. The subcutaneous prepatellar bursa (bursa subcutanea prepatellaris) is located in the layer of tissue in front of the patella. The popliteal fossa (recessus subpopliteus) is located behind the knee joint, under the tendon of the popliteal muscle.
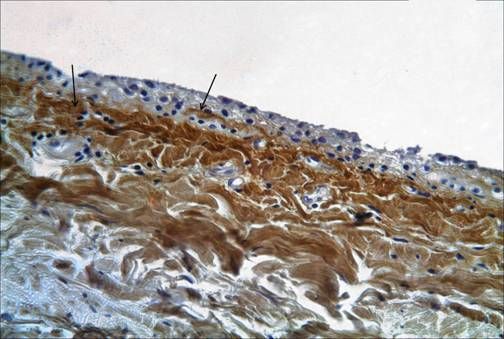
The synovial membrane lines the non-cartilaginous surface of the joint and differs from the mesothelial lining of other body cavities. It is not a true epithelial tissue. According to histological features, three types of synovial tissue are distinguished: the synovial lining of the alveolar surfaces, fibrous surfaces and adipose. The synovial membrane covering the cruciate ligaments is quite well innervated and abundantly supplied with blood. In addition, the knee joint has macroscopic synovial structures that have a certain significance - these are folds or plicae. The following most significant folds are distinguished: suprapatellar, infrapatellar, medialpatellar and lateral. The suprapatellar plica is the most common (in 90% of cases). The synovial folds themselves have little surgical significance, but under various pathological conditions they can increase in size, thicken, losing elasticity, which in turn leads to limited movement in the joint, especially flexion. Sometimes, intra-articular bodies are hidden in the thickness of the synovial folds.
The infrapatellar plica (lg. mucosum) is an embryonic septum between the medial and lateral parts of the joint. When it is hypertrophied, visualization of the various parts of the joint during arthroscopy is extremely difficult. The most frequently treated plica is the medial plica, which begins on the medial side of the joint, runs laterally, and enters the medial part of the synovial capsule, covering the infrapatellar fat pad. Its frequency of presence in the joint ranges from 18 to 55%.
Meniscus of the knee joint
The meniscus of the knee joint is located in the joint cavity and serves to support and protect the cartilage. In addition to shock-absorbing functions, the meniscus maintains the mutual conformity of the shapes of the articulating articular surfaces of the bones, and also reduces friction in the joints. Most knee injuries occur in the meniscus of the joint. With such injuries, mobility is limited, pain occurs, and in severe cases, the cartilage is damaged and arthrosis develops. Meniscus damage can be combined with ligament rupture, bone injuries, which requires immediate medical attention.

Depending on which meniscus is damaged, external or internal, the following types of injuries are distinguished:
- Meniscus detachment from the capsule
- Meniscus tear (most often seen in the internal meniscus, can be longitudinal or transverse)
- Meniscus compression (usually occurs in the lateral meniscus)
A meniscus tear can be caused by a knee injury, an awkward, sharp movement, for example, during a jump. Most often, such injuries occur among athletes. The prognosis for the outcome of the disease depends on the severity of the injury, its location, and the condition of the tissues. In chronic pathologies of the knee joint, the meniscus tissues can degenerate into fibrous growths, can become thinner and delaminate. The cartilaginous tissue loses its functions, which leads to the development of arthrosis of the knee joint.
When the meniscus is damaged, the following symptoms may appear: difficulty moving, especially when going up or down stairs, fluid accumulation in the joint, muscle tissue atrophy, a clicking sound in the knee, local increase in temperature in the affected area, pain when bending and straightening the knee, swelling.
Depending on how severe the disease is, treatment is prescribed, which can be either conservative or surgical. Conservative treatment includes the use of physiotherapy methods, the patient is advised to rest, ice can be applied to the affected area and elastic bandages can be applied. In case of large ruptures or separation of part of the meniscus from the capsule, as well as in case of ligament damage, treatment can be performed surgically using arthroscopy methods. The period of complete restoration of the joint's motor ability can vary from several weeks to two to three months.
The shape of the articular surfaces makes this joint condylar. It undergoes flexion and extension around the frontal axis (with a total volume of 150°). When the shin is flexed (due to the relaxation of the collateral ligaments), it can rotate relative to the vertical axis. The total volume of rotation reaches 15°, passive rotation - up to 35°. The cruciate ligaments inhibit pronation, and they relax during supination. Supination is inhibited mainly by the tension of the collateral ligaments. Flexion is limited by the tension of the cruciate ligaments and the tendon of the quadriceps femoris.
Active and passive stabilizers of the knee joint
The mechanisms of knee joint stabilization in various positions of the thigh, shin, in statics and dynamics, in normal and pathological conditions have been the focus of researchers for many years, but far from everything is clear in this problem at the present time.
For ease of consideration, these mechanisms are divided into passive and active. The former include the congruence of the articular surfaces and cartilaginous structures, as well as the capsular-ligamentous apparatus of the knee joint, which passively counteracts the displacement of the tibia. The latter include the periarticular muscles, which actively counteract this. In reality, they work simultaneously, mutually complementing and/or replacing each other. In case of injuries to the capsular-ligamentous structures, both mechanisms are disrupted to one degree or another, permanently or temporarily, as a result of which the function of the joint suffers - its instability is noted.
Stabilization of the knee joint is one of those problems whose solution is possible only with the use of data obtained in various fields of knowledge (morphology, physiology and biomechanics).
In order to determine which links in the pathogenesis of this process can be affected, restoring the impaired function, it is necessary to consider the mechanisms of knee joint stabilization. In addition, it is important to answer the question of which path to take. Should we rely on restoration or compensation of the function? In which cases should we choose conservative and in which surgical treatment tactics, and what is the role of functional therapy in these cases?
The solution to these fundamental issues is possible only with a careful examination of the features of the biomechanics of the knee joint.
Movements in the knee joint
Around the frontal axis up to 135° (flexion) and up to 3° (extension). Rotation of the lower leg around the longitudinal axis - up to 10°.
Flex the lower leg: biceps femoris, semimembranosus, semitendinosus, popliteus and gastrocnemius muscles.
The following muscles rotate the lower leg inward (with the knee bent): the semimembranosus and semitendinosus muscles, the sartorius muscle and the gastrocnemius muscle (medial head).
Rotation of the lower leg outward: gastrocnemius muscle, biceps femoris (lateral head).
Main diseases of the knee joint
 [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ]
[ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ]
Deforming arthrosis of the knee joint
This is a chronic disease in which degenerative processes occur in bone and cartilage tissues, leading to joint deformation. The main signs of deforming arthrosis: pain increases during movement, intensifies in damp and cold weather, and usually subsides at rest. The older a person gets, the higher the likelihood of developing the disease. This is explained by the fact that cartilage tissue inside the joints wears out over time and is increasingly difficult to restore after injuries and physical exertion. Hereditary factors also play an important role in the development of the disease.
Deforming arthrosis of the knee joint is accompanied by a crunch when moving, which passes over time, since the surface of the bones is smoothed out during friction. An inflammatory process develops in the knee joint, cysts appear in the bone tissue, it is difficult for the patient to move, he begins to limp when walking. The course of the disease is aggravated by physical overload, prolonged loads on the legs, for example, in people whose professional activities involve prolonged standing - sellers, teachers, athletes, etc.
Joint deformation usually begins to develop at the second stage of the disease. At the third stage, the joints are expanded and deformed to such an extent that the joint becomes completely immobile.
 [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 17 ], [ 18 ], [ 19 ], [ 20 ]
Arthritis of the knee joint
Knee arthritis is divided into osteoarthritis, rheumatoid arthritis and post-traumatic arthritis. The most common form of knee arthritis is osteoarthritis. This disease progresses gradually, depleting the articular cartilage. Osteoarthritis usually affects elderly and middle-aged people. Osteoarthritis, or gonarthritis, of the knee joint affects the periarticular muscles, including the synovial membrane, ligaments as a result of the inflammatory process in the soft tissues.
 [ 21 ], [ 22 ], [ 23 ], [ 24 ]
[ 21 ], [ 22 ], [ 23 ], [ 24 ]
Rheumatoid arthritis of the knee joint
It can occur in both acute and chronic forms. In the acute stage of the disease, fluid accumulates in the knee joint cavity. The patient feels pain, redness and swelling in the knee joint. The joint's motor activity is reduced, the patient tries to keep the leg in a semi-bent position. If pus has formed in the joint, the disease occurs with a high temperature and chills. The swelling of the joint is very pronounced. As a rule, this form of the disease affects two knee joints.
Post-traumatic arthritis of the knee joint
It occurs when the knee joint is injured and can develop over the years, gradually destroying the articular cartilage, causing pain and limiting the function of the joint.
Knee joint pain
Pain in the knee joint is accompanied by the following symptoms:
- Increases when walking up stairs
- Limits the motor activity of the joint, intensifies when trying to bend or straighten the leg
- Accompanied by a crunching sound when moving and the appearance of swelling
- The articular surfaces are deformed
- The thigh muscles atrophy
- An uneven, waddling gait appears
Pain in the knee joint often also occurs with coxarthrosis or osteoarthritis of the hip joint.
How is the knee joint examined?
Examine the patient lying on his back with his legs extended. Is there swelling in the knee joint area? (Causes: thickening of the bone, accumulation of fluid in the joint cavity, thickening of the synovium of the knee joint; in the latter case, "friction" is felt upon palpation.) Note whether there is atrophy of the quadriceps muscles. The presence of fluid in the knee joint cavity can be confirmed by the following technique: place the palm of one hand on the patella, or rather, on the area located just above it, and the thumb and index finger of the other hand below the patella. By changing the degree of pressure on the patella, the examiner causes movement of fluid in the knee joint cavity, which is felt with the fingers. If there is 30-40 ml of fluid in the joint cavity, then the phenomenon of patellar balloting can be caused, in which case its jolts against the surrounding bones are felt ("patella tapping"). These "tapping" sounds may be absent if the effusion is very small in amount or if it is "tense" but its volume exceeds 120 ml.
The degree of flexion and extension in the knee joints varies among individuals. Flexion is considered quite sufficient if a person can touch the buttock with his heel. Compare the extension of the knee joints on the diseased and healthy limbs. The condition of the medial and lateral ligaments is examined with the knee joint almost completely extended. With one hand, the examiner lifts the patient's leg, lying on the couch, by the ankle, and with the other hand slightly fixes the knee. The ligaments of the knee joint are strained at the moment of abduction - in this case, they try to abduct by grasping the ankle of the leg being examined with one hand, and with the other hand, located under the knee joint, push the knee joint in the medial direction (this is a test for the medial ligaments). Reverse manipulation with adduction in the knee joint is a test for the lateral ligaments. If these ligaments are torn, the knee joint will “open” more widely when examining the corresponding ligaments (be sure to compare the knee joints on both limbs).
The cruciate ligaments are examined by fixing the knee joint at an angle of 90°. The foot of the leg being examined is on the couch, and the examiner sits on it in order to immobilize the tibia. Grasp the knee from behind with your fingers so that the thumbs lie on the condyles of the femur. With the quadriceps muscle of the thigh relaxed, the anteroposterior transition of the tibia on the femur is assessed (normally it is approximately 0.5 cm), the anterior cruciate ligament limits the forward sliding of the femur, and the posterior one - backward. Excessive sliding in one of the directions (be sure to compare with the knee of the other leg) may indicate damage to the corresponding ligament.
The McMurray rotation test is designed to detect pedunculated (i.e., with preservation of the pedicle) meniscus tears. The knee joint is flexed, the tibia is rotated laterally, and then the knee joint is extended while continuing to rotate the tibia. The maneuver is repeated several times at different degrees of flexion in the knee joint, and then again with rotation of the tibia onto the femur. The purpose of this manipulation is to press the free end of the pedunculated meniscus inside the joint. When the knee is straightened, the pressed free end of the meniscus is released, and this is accompanied by a sensation of a peculiar click (sometimes audible), and the patient notes pain. This maneuver does not, however, reveal "bucket handle" tears. Remember: when moving a normal knee joint, clicking of the patella is usually audible.
Arthroscopy of the knee joint
Knee arthroscopy has made it possible to examine the internal structures of the knee joint, which makes it possible to establish an accurate diagnosis and diseases that cause knee pain without opening the joint. With this method, it has become possible to perform a number of surgical interventions in a closed joint, which undoubtedly shortens the recovery period for people who have undergone arthroscopic surgery.
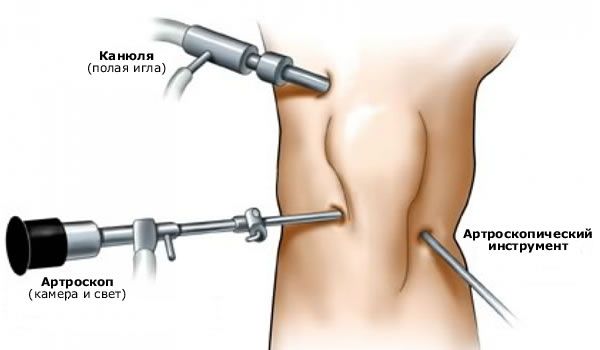
Arthroscopy of the knee joint is a universal examination method, the results of which are always compared with data from other studies.
In our opinion, arthroscopy is most valuable in various intra-articular pathologies: damage to the meniscus, articular cartilage, pathological condition of synovial folds, etc.
Arthroscopy becomes especially relevant in acute trauma, when there is extremely distorted symptomatology and the impossibility of conducting objective testing due to pain syndrome.
From our point of view, arthroscopic diagnostics is the most valuable method of examination for acute rupture of the ligamentous elements of the knee joint.
The earliest detection of cruciate ligament ruptures (in the first two weeks) makes it possible to perform surgical suturing of the ligament elements. In this case, one can hope for a good treatment result. However, if more than three weeks have passed since the injury, suturing the cruciate ligaments is inappropriate, since shortening of the collagen fibers occurs and irreversible avascular changes occur.
During diagnostic arthroscopy performed in the days following the injury, it is necessary to thoroughly wash the joint from blood, which subsequently prevents the progression of gonarthrosis. In addition, this ensures better verification of concomitant intra-articular pathology.
Previously, we attached great importance to partial ruptures of the cruciate ligaments, especially the ACL. We developed various diagnostic criteria for identifying this pathology, including arthroscopic signs of partial ruptures. However, later, taking into account the possibilities of compensation of the process, we came to the conclusion that in case of damage to the cruciate ligaments (especially in case of partial rupture), it is inappropriate to rely only on arthroscopy data, since damage to one or another anatomical substrate is not equivalent to instability of the knee joint.
That is why we currently perform diagnostic arthroscopy immediately before surgical stabilization of the knee joint. Its task is to identify combined intra-articular pathology, followed by surgical correction.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
MRI of the knee joint
MRI of the knee joint allows examining both bones and soft tissues, as well as objectively assessing all processes occurring in the joint and adjacent tissues. This allows identifying various pathologies at the earliest stages, for example, with a torn meniscus or injured ligaments. The MRI method is harmless, has few contraindications (contraindications include pregnancy, excess body weight, the presence of a pacemaker in the body). Magnetic resonance imaging is of great importance in preoperative examination of joints, as well as during the rehabilitation period. MRI of the knee joint is recommended for a torn meniscus, damaged ligaments, various injuries, infectious pathologies, tumors, swelling and pain in the joints and periarticular tissues.
The ACL normally appears as a dark band of low signal intensity on MRI of the knee. From the femoral insertion at the posteromedial aspect of the lateral condyle of the femur, the ACL extends anteriorly downward and medially. The tibial insertion is located anterolaterally on the tubercles of the intercondylar eminence.
The ACL is well visualized on sagittal sections with extension and external rotation of the tibia by 15-20°. External rotation reduces artifacts and straightens the ACL in the sagittal plane.
The ACL is brighter than the PCL, which is important because it can lead to a misdiagnosis of an ACL tear.
The macroscopic anatomy of the cruciate ligaments is also different: if the PCL is represented by parallel fibers, then the ACL is twisted. The data indicating a rupture of the ACL are the following: lack of visualization of the ACL, lack of continuity of the ligament fibers, or abnormal orientation of the remaining fibers.
A complete rupture of the ACL is diagnosed more based on indirect data: anterior translation of the tibia, excessive posterior tilt of the PCL, wavy contour of the ACL with a partial or complete rupture.
Diagnosis of PCL ruptures is much easier. When the leg is extended, the PCL has a slight posterior tilt in the sagittal plane.
Often, a fibrous band can be seen near the PCL, connecting the posterior horn of the lateral meniscus with the femoral condyle. This is the meniscofemoral ligament (Wrisberg or Humphrey).
Complete ruptures of the PCL are well defined by MRI of the knee joint, either by separation from the bone attachment, or by a defect in the middle of the substance. In the case of a partial rupture of the PCL, an increase in the intensity of its signal and focal thickening are noted.
In case of damage to the BCS, a low-signal intensity of the pole located close to the femur or tibia is determined.
The thickness of the MCL increases with hemorrhage and edema. Usually, MCL ruptures are limited to the deep location of the ligament, focal meniscocapsular divisions with synovial fluid are visualized, peripheral in relation to the meniscus and limited to a thin strip passing deep to the ligament.
A similar picture is presented by damage to the MCL, with the only difference being that the popliteal tendon and structural elements of the arcuat complex are often involved in the process.
X-ray of the knee joint
On X-rays of the knee joint, the articular surfaces of the bones that form it are clearly visible. The patella is superimposed on the distal epiphysis of the femur, the X-ray joint space is wide, curved in its middle part.
X-ray examination is the most accessible when examining patients with knee ligament damage. X-ray data subsequently influence the treatment plan. Of course, they correlate with the results of the clinical examination.
Radiography is performed in two standard projections. In addition, functional radiographs are taken. When evaluating the images, the position of the patella, the tibiofemoral angle, and the thickness of the articular cartilage are taken into account. The relationships and shape of the bones are assessed: the convexity of the lateral tibial plateau, the concavity of the medial, the dorsal position of the fibula in relation to the tibia.

For a correct assessment of the relationship of the tibia to the patella, lateral radiographs should be taken at 45° flexion. For an objective assessment of the rotation of the tibia, the lateral and medial condyles of the tibia should be superimposed. Usually, the medial femoral condyle is projected more distally than the lateral one. The height of the patella is also assessed.
If necessary, to determine the axis of the limb, additional radiographs are taken on long cassettes in a standing position in a direct projection, since with gonarthrosis there may be significant deviations from the norm.
To obtain additional information about the condition of the patellofemoral joint, axial images of the patella are taken, which allows for an analysis of the condition of the articular cartilage on its lateral and medial facets.
To determine the degree of displacement of the tibia relative to the femur in the anteroposterior and medial-lateral directions, we previously performed functional radiographs with a load; now this information is provided by ultrasound.
It is extremely important to pay attention to soft tissue calcification, bone fragment ruptures, and ossification of the femoral attachment of the BCL. T. Fairbank (1948) described a number of radiographic symptoms observed late after meniscus removal: formation of ridges and osteophytes along the edge of the tibia, flattening of the femoral condyles, narrowing of the joint space, which progress over time.
We have noted a number of radiographic signs characteristic of chronic anterior instability of the knee joint: a decrease in the intercondylar fossa, a narrowing of the joint space, the presence of peripheral osteophytes on the tibia, the upper and lower poles of the patella, a deepening of the anterior meniscal groove on the lateral condyle of the femur, hypertrophy and sharpening of the tubercle of the intercondylar eminence.
When determining the severity of deforming arthrosis, one is guided by the radiological signs described by N.S. Kosinskaya (1961). There is a direct correlation between the severity of gonarthrosis and the degree of knee instability, as well as the timing of seeking medical care, the number of previously performed surgical interventions in those whose knee joint was injured.

