Medical expert of the article
New publications
Blockade of the left bundle branch of the Hiss bundle
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
What is left bundle branch block? It is an abnormality of electrical activity of the heart detected on ECG, indicating impaired conduction of electrical impulses along the left fibers of the atrial-ventricular (atrioventricular) bundle. [1]
Epidemiology
According to clinical statistics, left atrial-ventricular bundle branch block is detected in nearly 6% of patients aged 70+ on diagnostic ECG, and in the elderly it most often indicates coronary heart disease that develops due to atherosclerosis.
In people under 50 years of age, LVAD is found in approximately 1% of cases, and its etiologic factor is chronic elevation of BP. In the general population, the prevalence of left bundle branch block is estimated at 0.06-0.1%
It is also known that in almost 90% of people the detection of such a disorder of the conduction system of the heart becomes the starting point for the diagnosis of serious cardiovascular diseases. And in almost one third of patients with heart failure ECG shows the presence of blockade of the left bundle branch of Hiss.
Causes of the left bundle branch block
The main causes of left bundle branch blockade (in the medical literature the abbreviation BLNPG is used) are considered to be:
- Heart attack and myocardial infarction;
- Acute left ventricular failure of various etiologies, including systemic arterial hypertension and ischemic heart disease;
- Stenosis of the heart valves;
- Inflammation of the heart muscle - myocarditis;
- Myocardial stiffness associated with myocardial fibrosis, which may be caused by damage to its tissue due to hypoxia, inflammation, or excessive hemodynamic effects of coronary blood flow;
- Dilated cardiomyopathy, in which the heart muscle is stretched and increases in size;
- Hypertrophic cardiomyopathy;
- Calcinosis of the conduction system of the heart.
In particular, left bundle branch block in athletes is due to left ventricular hypertrophy resulting from physical exertion and defined as the sports heart.
And left bundle branch block in pregnancy in most cases is the result of elevated BP or gestation-related type of heart failure - peripartum cardiomyopathy.
Congenital block of the left bundle branch of the Hiss bundle - without or with abnormal heart rhythm - has been reported in congenital heart defects. In addition, experts say idiopathic congenital cardiac electrical conduction disorders are linked to a group of rare genetic conditions defined as ion channelopathies. They are the result of genetic changes affecting ion channels in the walls of heart muscle cells, which provide a chemical (ionic) pathway for cell-to-cell signaling. [2]
Risk factors
Risk factors for Hiss bundle branch blockade include:
- Advanced age;
- Chronic elevation of BP and atherosclerotic cardiosclerosis;
- The presence of cardiac pathologies, including atrial or interventricular septal defects, coronary artery obstruction, and the entire spectrum of metabolic myocardial changes inflammatory, endocrine, and autoimmune origin.
Pathogenesis
Controlling the heartbeat the conduction system of the heart includes a bundle of fibers that conduct electrical impulses from the AV node (atrioventricular node of the interatrial septum) to the muscle cells of the lower chambers of the heart (ventricles) - the bundle of Hiss, as well as its legs and their anterior and posterior branches.
The bundle of Guis (fasciculus atrioventricularis) is a set of specialized Purkinje cells, transitional cardiomyocytes and specialized cardiomyocytes, called pacemaker cells, that create rhythmic impulses.
The legs of this bundle are subendocardial Purkinje muscle fibers originating from the interventricular septum and running along it in the subendothelial layer of the lateral walls of the ventricles to their papillary muscles (m. Papillares). The cells of these fibers are larger than ordinary cardiomyocytes and are connected by desmosomes and connexons (gap junctions), and their function is to distribute electrical impulses evenly for coordinated ventricular contraction. The left pedicle (crus sinistrum) is responsible for transmitting electrical excitation to the left ventricle (ventriculus sinister).
The pathogenesis of complete or partial blockade of conduction of electrical impulses generated by the sinoatrial (sinus) node by the left leg experts explain by violations of the path of their passage, which leads to desynchronization of the contraction of the muscular walls of the ventricles.
The mechanism of such a disturbance may be due to the occurrence of the so-called action potential conduction loop in the Purkinje fiber network due to upward and downward propagation of the impulse along different pathways. Thus, the response of the left ventricle is delayed (with slower depolarization and longer refractory period), and the right ventricle is activated and contracts before the left ventricle during the isoelectric interval.
Symptoms of the left bundle branch block
Quite often BLNPH does not cause any symptoms, is detected on ECG quite accidentally and does not cause special clinical problems.
However, the first signs in the form of dyspnea and fatigue may indicate a decrease in the functional capacity of the left ventricle (the intensity of its systolic contraction) to provide sufficient cardiac output to maintain blood flow to other organs.
The most common clinical symptoms of left pedicle blockade are:
- Pre-syncope and syncopal episodes (fainting) due to lack of blood flow to the brain;
- Cardiac arrhythmias;
- Increased blood pressure;
- Chest pain, often acute.
According to the degree of violation of cardiac electrical conduction, its dynamics and localization, such types of BLNPH are distinguished as:
- Partial or incomplete blockade of the left bundle branch (its main trunk, without branches);
- Complete blockade of the left bundle branch of the Hiss bundle or double bundle blockade - cessation of impulse conduction along the main stem and its branches;
- Transient or transient left bundle branch blockade;
- Intermittent - intermittent blockade of the left leg of the bundle of Hiss, in which impulses are not conducted simultaneously with the right leg of the bundle, which is manifested by irregular heartbeat. In such cases, patients may experience chest pain on exertion and at rest;
- Blockade of the anterior branch of the left bundle branch of the Hiss bundle - with impulse transmission through its posterior branch and the right bundle branch;
- Blockade of the posterior branch of the left bundle branch.
If conduction is blocked through one of these branches, the blockade is called fascial blockade.
Blockade of the right and left legs of the bundle of Hiss leads not to a complete "shutdown" of the cardiac conduction system, but to a change in the sequence and timing of ventricular depolarization, which continues to be controlled by the sinus node, and electrical impulses can pass through alternative pathways. Such blockade may be manifested by cardiac arrhythmias (ventricular and supraventricular tachycardia), dyspnea and decreased HR (bradycardia).
Also read - heart rhythm and conduction disorder: symptoms and diagnosis
Complications and consequences
Is left bundle branch block dangerous? It leads to disruption of heart rhythm, and if the patient has heart failure with a significant reduction in left ventricular ejection fraction, the efficiency of the heart is significantly reduced, which can accelerate the progression of the disease and exacerbate its symptoms. It also increases the risk of fatal heart attack in such patients.
A serious consequence of BLNPH is left ventricular failure with adrenal adrenal release of adrenaline (and increased HR and BP), pulmonary edema, and the development of pulmonary hypertension.
It should be kept in mind that any disruption of the function of the bundle of Hiss can lead to Grade I heart block (with atrioventricular conduction delays), atrioventricular block and Grade III heart block - with complete dissociation of electrical conduction between the atria and ventricles.
Diagnostics of the left bundle branch block
Left bundle branch blockade of the left bundle branch of the Hiss often indicates the presence of some form of underlying heart disease, so a heart study is necessary to detect it.
The blockage itself is usually diagnosed using electrocardiography (ECG) and two-dimensional Echocardiography - echocardiography (which evaluates the performance of the left ventricle by determining its ejection fraction).
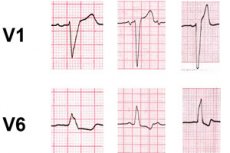
Left bundle branch blockade on ECG is confirmed by a leftward deviation of the electrical axis of the heart (EOS), and its incomplete blockade is characterized by a sharp deviation of the EOS to the left or right. The electrocardiogram also shows wider QRS segments (ventricular complex) exceeding the norm and their downward deviation in lead V, with dominant S teeth; wide monophasic R teeth are recorded in lateral leads, and Q teeth are absent. The normal direction of ventricular depolarization changes (causing sequential depolarization instead of simultaneous depolarization), which is expressed on ECG by reverse directionality (discordance) of ST segment and T plaque.
Also read: analyzing and deciphering an ECG
Patients undergo blood tests: general clinical, electrolytes, AST, ALT, LDH and cardiac troponins.
Instrumental diagnostics are performed, for more information see. - instrumental methods of cardiac examination
Differential diagnosis
Of course, differential diagnosis is also necessary, including blood electrolyte imbalance, right bundle branch block, AV block, left ventricular aneurysm, left ventricular hypokinesia, sinus node weakness syndrome, Leva-Lenegre disease, Wolff-Parkinson-White syndrome, Adams-Stokes-Morganier syndrome, and others.
Treatment of the left bundle branch block
BLNPH can be a sign of underlying heart disease, which is treated by a cardiologist.
Depending on the etiology and the symptoms present, medications are prescribed:
- Hypotensive - pills for high blood pressure
- Antiarrhythmic drugs
- Drugs to prevent and correct heart failure
In case of complete left bundle branch block with severe heart failure, cardiac resynchronization therapy with pacemaker surgery may be considered.
Read also - hiss bundle branch blockade: causes, symptoms, diagnosis, treatment
Prevention
It is not possible to prevent the appearance of this electrocardiographic sign of a violation of the conductive system of the heart, and doctors recommend all known measures for the prevention of cardiovascular diseases.
Forecast
If a middle-aged person after a thorough cardiologic examination does not show any signs of heart pathology, the prognosis is quite good. In these cases, left bundle branch blockade of the Hiss is considered a benign incidental finding on ECG, and the army, that is, compulsory military service is not canceled. Although in BLNPH with pre-syncope in the USA and the UK it is forbidden to work as airplane pilots.

