Medical expert of the article
New publications
Complete heart block
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Among all types of dysfunction of the heart's conducting system, which ensures the rhythmicity of the heartbeat and controls coronary blood flow, the most serious is complete heart block - with complete cessation of the passage of electrical impulses between the atria and ventricles. [1]
Epidemiology
The incidence of complete heart block is estimated to be 0.02-0.04% of the general population. Third-degree AV blockade is observed in 0.6% of patients with hypertension, in about 5-10% of patients with inferior wall myocardial infarction and in the same number of people over 70 years of age with a history of cardiac pathologies.
Clinical evidence suggests that idiopathic fibrosis and sclerosis of the conduction system is the cause of nearly half of cases of complete AV blockade.
Third-degree congenital heart block occurs in one child for every 15,000 to 20,000 births.
Causes of the complete heart block
Complete heart block is what cardiologists call atrial-ventricular or third-degree atrioventricular block.
This is complete AV heart block or complete transverse heart block, in which action potentials generated by the sinoatrial (SA) node do not pass through the AV node (atrioventricular or atrial-ventricular) as a result of a defect of the conduction system of the heart anywhere from the AV node to the bundle of Guis, its branches (legs) and Purkinje fibers. [2]
The main causes of heart rhythm and conduction abnormalities, leading to complete heart block, are related to:
- Acute ischemic heart disease;
- Complications of myocardial infarction, affecting the inferior wall of the heart, and postinfarction cardiosclerosis;
- Atherosclerosis of the coronary vessels that supply blood to the structures of the conductive system;
- Cardiomyopathies, including diabetic hypertrophic and idiopathic dilatation;
- Congenital heart disease;
- Idiopathic degeneration (fibrosis and calcification) of the conduction system (most often the proximal leg of the Hiss bundle), which is called senile conduction degeneration or Leva disease;
- Long-term use of antiarrhythmic drugs of all classes and cartiotonic agents of cardiac glycosides group (Digoxin, Celanide, Lanatosite and other foxglove preparations);
- Electrolyte imbalance - violation of the ratio of potassium and magnesium in the presence of hypermagnesemia or hyperkalemia.
In children, high-grade AV block may occur in a completely structurally normal heart or in association with concomitant congenital heart disease. Congenital AV block (with high neonatal mortality) may result from an autoimmune process affecting the developing fetal heart, particularly from exposure to anti-nuclear anti-Ro/SSA autoantibodies, which are associated with many autoimmune diseases.
Risk factors
In addition to cardiac pathologies of a structural nature, coronary atherosclerosis and other cardiovascular diseases, risk factors for complete heart block are:
- Advanced age;
- Arterial hypertension;
- Diabetes;
- Increased vagus nerve tone;
- Endocarditis, Lyme disease and rheumatic fever;
- Cardiac surgery and transdermal coronary interventions;
- Systemic diseases such as lupus erythematosus, sarcoidosis, amyloidosis.
In addition, risk factors can be genetically determined, as in brugada syndrome, resulting from a mutation in the SCN5A gene, which encodes the alpha subunits of the integral membrane protein of cardiac myocytes that forms potential-dependent sodium channels (NaV1.5) in heart muscle. About a quarter of people with this syndrome have a family member with this mutation.
Pathogenesis
Specialists explain the pathogenesis of complete AV heart block by the absence of electrical connection between the atria and ventricles through the atrioventricular (AV) node and their complete dissociation.
To ensure the completion of the contraction cycle in the atria before the onset of contraction in the ventricles, the impulse received from the sinoatrial (SA) node must be delayed in the AV node, but in third-degree blockade, the atrioventricular node cannot conduct signals. And disruption of this pathway leads to impaired activation of atria and ventricles through the Gis-Purkinje system, as a result of which their coordination (synchronization) is lost.
In this case - since the CA node cannot control the heart rate without appropriate conduction through the AV node - the atria and ventricles begin to contract independently of each other. Since the impulses do not travel to the ventricles, their contraction occurs due to a substitute or so-called ectopic slip rhythm, which can be mediated by the AV node, one of the Gis bundles (if a return conduction loop is formed) or by the ventricular cardiomyocytes themselves (and such a rhythm is called idioventricular).
As a consequence, the ventricular contraction rate drops to 40-45 beats per minute, resulting in decreased cardiac output and hemodynamic instability. [3]
Symptoms of the complete heart block
In complete AV blockade, the first signs may be manifested by a feeling of weakness, general fatigue fatigue, dizziness.
In addition, clinical symptoms of complete cardiac conduction blockade may include: dyspnea, sensation of chest pressure or pain (if blockade accompanies acute myocardial infarction), changes in heartbeat (in the form of pauses and fluttering), pre-syncope or sudden loss of consciousness (syncope).
Although in complete AV dissociation the atrial rhythm is greater than the ventricular rhythm and there is supraventricular tachycardia, physical examination usually reveals bradycardia. And at HR <40 beats per minute, patients may show signs characteristic of decompensated heart failure, respiratory failure and systemic hypoperfusion: sweating, decreased skin temperature, rapid shallow breathing, peripheral edema, mental changes (up to delirium).
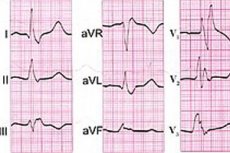
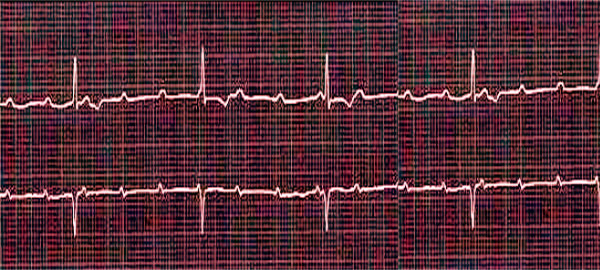
Complete heart block may differ in localization, and specialists distinguish proximal and distal types of block. In the proximal type, a substitutive slipping rhythm is set by the AV node, and the ventricular complex (QRS) on the electrocardiogram is not dilated, and the ventricles contract at a rate of about 50 times per minute.
Distal type of blockade is defined when the source of ectopic slipping rhythm becomes the bundle of Hiss (atrioventricular bundle of myocardial conducting cells in the muscle of the interventricular septum) with legs. In this case, the rate of ventricular contractions within one minute falls to 3O, and the QRS complex on the ECG is dilated.
In third-degree AV block, there is complete right bundle branch blockade - right bundle branch blockade, and complete left bundle branch blockade - left bundle branch blockade.
Conditions in which both the right bundle branch and the left anterior or left posterior bundle are blocked are called bifascicular blockades. And when the right branch of the Gis bundle, the left anterior bundle and the left posterior bundle are blocked, the blockade is called trifascicular (three-beam). And this is complete Gis bundle blockade or complete trifascicular transverse blockade of the distal type. [4]
Complications and consequences
What is the danger of complete heart block? It is dangerous in itself because it can cause sudden full cardiac arrest - asystole. [5]
Also at risk are complications of complete AV heart block, including:
- Deterioration of blood supply to all systems and organs, including cerebral ischemia with morgagni-Adams-Stokes syndrome;
- Development of dilated cardiopathy;
- Ventricular fibrillation;
- Ventricular tachycardia;
- Worsening of heart failure and exacerbation of angina pectoris;
- Cardiovascular collapse.
- Arrhythmic cardiogenic shock.
Diagnostics of the complete heart block
The initial diagnosis of complete heart block is often made by an emergency physician or emergency room physician.
Only instrumental diagnostics can confirm or refute the initial diagnosis: ECG (electrocardiography) in 12 leads or Holter monitoring.
After stabilization of the condition, chest X-ray and ultrasound, as well as blood tests (general and biochemical, for the level of electrolytes, C-reactive protein and creatine kinase, myoglobin and troponins) make it possible to find out the root cause of this condition and identify associated diseases.
Read more in the publication - heart Research
And differential diagnosis is necessary to distinguish between other types of cardiac conduction disorders and pathologies with similar symptomatology.
Who to contact?
Treatment of the complete heart block
Patients with third-degree AV blockade require urgent hospitalization. According to the treatment protocol, intravenous Atropine is used as first-line therapy (in the presence of a narrow QRS complex, i.e., nodal slip rhythm). Beta-adrenomimetics (Adrenaline, Dopamine, Orciprenaline sulfate, Isoproterenol, Isoprenaline hydrochloride) are also used, which, having a positive chronotropic effect, can increase HR.
In emergency situations - in acute hemodynamic instability of patients - temporary percutaneous cardiac pacing should be performed, and if ineffective, a transvenous pacemaker may be required.
Temporary percutaneous or transvenous pacing is required if heart rate slowing (or asystole) caused by AV blockade requires correction and permanent pacing is not immediately indicated or is unavailable.
Permanent electrocardiostimulation, i.e. pacemaker surgery, is the therapy of choice for patients with symptomatic complete AV blockade accompanied by bradycardia.
Prevention
The possibility of preventing the development of complete heart block can be realized by treating the diseases that cause it.
Forecast
Cardiologists relate the prognosis of complete heart block to the underlying diseases that caused the severity of rhythm and conduction disturbances and the severity of its clinical manifestations in patients.
By restoring coronary perfusion in acute myocardial infarction, complete transverse heart block may be reversible, but the risk of sudden cardiac death remains high.
Literature used
- "Heart Block: Causes, Symptoms and Treatment" - Charles M. McFadden (2018).
- "Complete Heart Block: Management and Case Reports" - Isabella Y. Kong, Jason P. Davis (2020).
- "Heart Block: A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References" - Icon Health Publications (2004).
- "Complete Heart Block and Congenital Heart Disease" - Eli Gang, Kadambari Vijay (2019).

