Medical expert of the article
New publications
Calcinosis: what is it, how to treat?
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
What does calcification mean? It is the formation of accumulations of insoluble calcium salts where their presence is not expected either from an anatomical or physiological point of view, that is, outside the bones.
Among all the biogenic macroelements of the human body, the proportion of calcium – in the form of hydroxyapatite crystals in bone tissue – is the most significant, although blood, cell membranes and extracellular fluid also contain calcium.
And if the level of this chemical element is significantly increased, then calcification develops – a disorder of mineral metabolism (code E83 according to ICD-10).
Causes calcinosis
Calcium metabolism is a multi-stage biochemical process, and today the key causes of calcinosis, as one of the types of mineral metabolism disorders, have been identified and systematized. However, given the close relationship between all metabolic processes occurring in the body, in clinical endocrinology it is customary to simultaneously consider the pathogenesis of calcification (or calcification) deposition.
The primary cause of calcareous dystrophy is recognized as the oversaturation of the blood with calcium - hypercalcemia, the etiology of which is associated with increased osteolysis (destruction of bone tissue) and the release of calcium from the bone matrix.
Hypercalcemia, as well as hyperthyroidism or parathyroid gland pathologies, reduce the thyroid gland's production of calcitonin, which regulates calcium levels by inhibiting its excretion from the bones. It is assumed that it is the presence of hidden thyroid problems in postmenopausal women - in combination with a decrease in the level of estrogens that retain calcium in the bones - that causes extraosseous calcium deposits, i.e., calcification in osteoporosis.
There are other pathological conditions that cause calcium salts to concentrate in the wrong places. Thus, in patients with primary hyperparathyroidism, hyperplasia of the parathyroid glands or their hormonally active tumor, the synthesis of parathyroid hormone (parathyroid hormone or PTH) increases, as a result of which the action of calcitonin is suppressed, and the level of calcium in the blood plasma, as well as bone demineralization, increases.
It is necessary to take into account the importance of phosphorus in calcium metabolism, because the violation of the proportions of the content of these macroelements in the body leads to hyperphosphatemia, which increases the formation of "calcium deposits" in the bone, soft tissues, and blood vessels. And oversaturation of the renal parenchyma with calcium salts leads to renal failure and the development of nephrocalcinosis.
The mechanism of increased osteolysis with the release of calcium phosphate and carbonate from bone depots in the presence of cancerous tumors of any localization is explained by the so-called paraneoplastic syndrome: the growth of malignant neoplasms is accompanied by hypercalcemia, since mutated cells are capable of producing a polypeptide similar in action to parathyroid hormone.
It is well known that the pathogenesis of calcium salt formation can be caused by an excess of vitamin D, which in endocrinology is associated with an increase in the synthesis of 1,25-dihydroxy-vitamin D3 - calcitriol, which actively participates in the process of calcium and phosphorus metabolism. Hypervitaminosis of vitamin A, leading to osteoporosis, as well as a deficiency of vitamin K1 from food and endogenous vitamin K2 are involved in the development of calcareous dystrophy.
In the absence of endocrine pathologies, the content of total calcium in the blood plasma does not exceed the physiological norm, and then the causes of calcinosis are different, caused by local factors. These include the deposition of calcium phosphate on the membranes of organelles of damaged, atrophied, ischemic or dead cells, as well as an increase in the pH level of the intercellular space fluid due to the activation of alkaline hydrolytic enzymes.
For example, the process of calcification in the case of vascular atherosclerosis is presented as follows. When cholesterol deposited on the vessel wall is covered with a shell formed from glycoprotein compounds of the endothelium, a cholesterol plaque is formed. And this is classic atherosclerosis. When the tissues of the atheromatous plaque shell begin to be "saturated" with calcium salts and harden, this is already atherocalcinosis.
A shift in the hydrogen index of blood acidity (pH) towards the alkaline side with partial dysfunction of the physicochemical buffer system of the blood (bicarbonate and phosphate), which maintains the acid-base balance, plays a significant role in the etiology of calcium metabolism disorders. One of the reasons for its disorder, leading to alkalosis, is Burnett syndrome, which develops in those who consume a lot of calcium-containing products, taking baking soda or antacids that neutralize gastric acid, which are adsorbed in the gastrointestinal tract, for heartburn or gastritis.
It is believed that any of the above endocrine disorders are aggravated by excessive calcium intake with food. However, as Harvard University researchers claim, there is still no strong evidence that dietary calcium increases the likelihood of tissue calcification, since it does not cause a persistent increase in blood calcium levels.
Risk factors
As clinical practice shows, in some cases the calcification process is triggered by various infections – tuberculosis, amebiasis, toxoplasmosis, trichinosis, cysticercosis, meningitis, encephalitis, etc. – and the accompanying inflammatory processes with tissue damage.
The following risk factors for the development of calcification are also identified:
- bone fractures, during the healing of which osteoclasts are activated, utilizing damaged bone tissue with their enzymes;
- deterioration of bone tissue trophism during prolonged bed rest or paralysis (paraplegia), leading to immobility;
- malignant neoplasms;
- chronic granulomatous diseases (sarcoidosis, Crohn's disease);
- autoimmune pathologies of a systemic nature (scleroderma, rheumatoid arthritis, lupus);
- chronic kidney pathologies with a decrease in their filtration capacity (in this case, the metabolism of phosphorus and calcium is disrupted with the development of secondary hyperparathyroidism);
- chronic form of adrenal cortex insufficiency - Addison's disease, leading to hypocorticism and cortisol deficiency, as a result of which the content of Ca cations in the blood increases;
- hypercholesterolemia, elevated LDL levels in the blood, systemic atherosclerosis;
- heart defects, infectious endocarditis, cardiac surgery;
- vascular anomalies, vascular surgery;
- osteoporosis and osteopenia (decreased bone mineral density);
- diabetes mellitus (with high blood glucose levels, the absorption of magnesium, which prevents the deposition of calcifications, is impaired);
- insufficient level of magnesium in the body (without which insoluble calcium salts cannot be transformed into soluble ones);
- malabsorption syndrome (in which the binding of Ca inside cells increases);
- age-related degenerative-dystrophic changes in bone and connective tissues, involutional changes in the walls of blood vessels;
- long-term use of diuretics belonging to the thiazide group (which reduce the excretion of calcium by the kidneys), corticosteroids, heparin, anticonvulsants and laxatives;
- hemodialysis (increases the risk of arterial calcification);
- radiation therapy and chemotherapy for cancer.
A separate item in this list should be noted: calcinosis and heredity, in particular, genetically determined predisposition to deforming osteodystrophy; collagenoses and hereditary chronic granulomatous disease; familial hypocalciuric hypercalcemia (due to mutation of genes encoding calcium-sensitive receptors of cell membranes).
Calcium deposits in the lumbar intervertebral discs, hip, knee and shoulder joints and surrounding soft tissues may be associated with a slowly progressive genetic disease called ochronosis (alkaptonuria).
Symptoms calcinosis
The symptoms of calcinosis are caused not so much by its etiology as by the specific location of the calcifications. At the same time, they rarely manifest themselves or do not manifest themselves at all, since in most cases they accompany other nosological forms.
Initial calcification can only be detected using imaging equipment – either by chance or when a patient with elevated calcium levels in the blood is prescribed an examination.
But the first signs of the formation of subcutaneous calcium granulomas near the joints of the extremities, which are fused with the skin and begin to shine through it as they grow, can be seen without an X-ray. This is scleroderma calcinosis of the skin or dystrophic calcinosis in scleroderma.
Soft tissue calcification
In addition to scleroderma calcinosis of the skin, soft tissue calcinosis can be palpated in posttraumatic ossifying myositis: a dense area can be felt in the muscle, where calcifications are deposited. The main symptoms are intense pain and stiffness of movement, the skin over the lesion turns red, and the subcutaneous tissue swells.
Focal calcinosis of the gluteal muscles (small or medium) - with moderate pain of varying intensity and swelling - can develop after injuries, burns or intramuscular injection of drugs. Severe pain in the buttock area and even limping when walking are caused by calcification foci formed due to arthrosis of the hip joint, sarcoma or progressive congenital Gaucher disease. In case of paralysis of the limbs, dystrophic calcinosis affects the muscles of the lower leg and thigh.
And with toxoplasmosis, ochronosis or malignant tumor of the retina (retinoblastoma) calcification of the oculomotor muscles that hold the eyeball in the orbit occurs. A decrease in their elasticity prevents normal eye movement.
When calcium-phosphorus salts are deposited in the synovial bags of joints and periarticular tissues, metabolic calcification of tendons, ligaments, hyaline and fibrous cartilages is observed. The following may be diagnosed: calcifying tendinitis of the supraspinatus tendon; chondrocalcinosis in the ankle, knee and hip joints; calcification of the quadriceps tendon (in the area of the tibial tubercle or near the kneecap). In all cases, local pain, signs of local inflammation, and limited mobility are observed.
 [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
[ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ]
Vascular calcification
Calcium deposits on the walls of blood vessels most often appear in atherosclerosis, involutional fibrosis of the vascular walls, autoimmune and congenital endothelial dysplasia - such as dystrophic calcification.
Narrowing of blood vessels by 15-25% and slowing of blood flow, which can result from calcification of the aortic arch in areas where atherosclerotic plaques form, causes attacks of weakness and headaches; dizziness and fainting; a feeling of discomfort in the mediastinum and paresthesia of the fingers. In addition, diffuse calcification of the aorta with similar symptoms is observed in syphilitic mesaortitis and autoimmune aortoarteritis.
Severe calcification of the thoracic aorta, in addition to the symptoms already mentioned, leads to shortness of breath, arrhythmia and increased blood pressure, pain in the heart area, radiating to the shoulder, neck, shoulder blades and hypochondrium. And calcification of the abdominal aorta makes itself known by a decrease in appetite and overall body weight; aching pain in the abdominal cavity associated with food intake; problems with the intestines; heaviness and pain in the legs.
Arterial calcification, as a rule, accompanies the same atherosclerosis or age-related decrease in the elasticity of vascular walls - fibrosis and calcification, affecting arterial vessels in the areas of their bifurcation. Thus, calcification of the carotid arteries, which supply blood to the brain, is detected in many patients in the area of the carotid sinus, where the common artery divides into external and internal. Narrowing of the lumen of these vessels, as well as the mouth of the subclavian artery - if there is diffuse calcification of the arteries of the neck - manifests itself not only in the form of headache, dizziness, temporary loss of vision, nausea and vomiting, but also neurological symptoms: paresthesia of the extremities, movement and speech disorders. The result may be a stroke, for more details see - Stenosis of the carotid artery.
Constantly cold feet, limping, deterioration of the skin trophism on the toes (with areas of atrophy and ulceration), pain in the legs, and erectile dysfunction in men can manifest themselves as calcification of the iliac arteries (originating at the bifurcation of the abdominal aorta), which leads to stenosis and obliteration.
If calcification of the arteries of the lower extremities develops (in half of the cases, this is atherocalcinosis in the elderly, in the rest - a consequence of diabetes in people aged 35 and older), then its typical localization is the superficial femoral artery or arteries of the lower leg. And among the symptoms, heaviness and pain in the legs, paresthesia and cramps are noted.
Cardiac calcification
When identifying cardiac calcification, cardiologists distinguish between calcification of its membranes, the coronary arteries that supply them with blood, and the valves that regulate blood flow.
Patients with calcifications in the outer lining of the heart (pericardium) or its muscular lining (myocardium) experience all the signs of heart failure: shortness of breath, pressure and burning behind the breastbone, rapid heartbeat and pain in the heart area, swelling of the legs, and sweating at night.
Coronary calcification (calcification of the coronary arteries) has symptoms of angina pectoris, that is, severe shortness of breath and chest pain radiating to the shoulder.
Non-rheumatic lesions of the heart valves with fibrosis, calcification and stenosis include calcification of the aortic valve or calcification of the aortic root in the area of the fibrous ring, which can be defined as degenerative calcification of the aortic valve or degenerative calcified stenosis of its cusps. Whatever its name, it leads to cardiac, coronary or left ventricular failure with corresponding cardiac symptoms.
The degree of calcification, like the degree of stenosis, is determined during CT scanning: grade 1 aortic valve calcification means the presence of one deposit; grade 2 aortic valve calcification is determined if there are several calcifications; in case of diffuse lesions that can affect nearby tissues, grade 3 aortic valve calcification is diagnosed.
Mitral valve calcification or mitral calcification is accompanied by similar symptoms plus hoarseness and coughing fits.
Calcification of the brain
In the form of focal or diffuse deposits, cerebral calcification is detected by MRI in patients with tumors - teratoma, meningioma, craniopharyngioma, intraventricular ependymoma, pineal gland adenoma. Multiple calcifications are formed in gliomas, glioblastomas and giant cell astrocytomas. Among the most common symptoms are severe headaches, visual impairment, paresthesia and paresis of the limbs, tonic-clonic seizures.
Damage to individual structures due to encephalopathies of infectious and parasitic origin (toxoplasmosis, cysticercosis, cryptococcosis, CMV) can cause focal calcifications in the subarachnoid space, in the gray and white matter. They manifest themselves in different ways - in accordance with the loss of functions of neurons in the affected areas.
Often, asymptomatic calcification of the basal nuclei (basal ganglia of the brain), as well as the dentate nucleus of the cerebellum, is observed in old age. And in the hereditary Fahr disease, which can manifest itself in adults of different ages, neurodegenerative changes (cognitive and mental) steadily progress.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
Calcification of bones and joints
Dystrophic calcification of bones accompanies almost all bone neoplasms. For example, with benign osteochondroma, cartilaginous growths form on tubular and flat bones, in which calcium salts settle. Such calcified growths can be painful and limit mobility.
Calcification of the lower extremities - with bone sarcoma affecting the tissues of the tubular bones (hip, fibula or tibia) - pain and deformation increase, leading to impaired motor functions.
Considering the tendency of glycosaminoglycans of connective periarticular tissues and cartilage to attract Ca2+, joint calcification can be considered a comorbid process in the development of joint diseases, especially in their chronic forms, typical for mature and elderly people.
Calcification of the shoulder joint, elbow and wrist, calcification in the hip joint area, calcification of the knee joint with deposition of calcium pyrophosphate crystallohydrates in the synovial membrane or joint capsule, cause inflammation, swelling, severe pain and lead to limited mobility of the limbs.
 [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ]
[ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ]
Calcification of visceral organs and glands
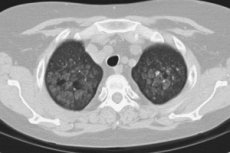
First of all, calcification of the lungs is associated with tuberculosis (in which tuberculous granulomas and areas of adjacent necrotic tissue become calcified). Calcification may affect the lungs and bronchi in patients with chronic pneumoconiosis (silicosis, asbestosis, etc.) or parasitic pneumocystosis (ascariasis, toxoplasmosis, echinococcosis, etc.); in the presence of cysts or as a result of damage after prolonged forced ventilation of the lungs.
Calcifications appear in the lungs of patients with sarcoidosis or metastatic leukemia. Read about pleural calcification in the article – Pleural fibrosis and calcification
 [ 36 ], [ 37 ], [ 38 ], [ 39 ]
[ 36 ], [ 37 ], [ 38 ], [ 39 ]
Renal calcification
Symptoms of renal failure - polyuria, nausea, thirst, cramps, general weakness, back pain - are manifested by nephrocalcinosis or dystrophic calcification of the kidneys, chronic glomerulonephritis (with calcifications in the tissue of the membranes of the nephron tubules and in the epithelium of the glomeruli), kidney tumors (carcinoma, nephroma).
Calcification of the renal pyramids revealed by ultrasound means the formation of calcium salt accumulations in the triangular areas of the renal medulla, i.e. where the filtering and urine-forming nephrons are located. And parietal calcification in the kidneys develops when parenchyma cells atrophy or die – due to pyelonephritis or polycystic disease.
Adrenal calcification
When patients have a history of tuberculosis or cytomegalovirus adrenalitis, a cystic formation in their medulla or Addison's disease (which destroys this substance), an adenoma of the adrenal cortex, pheochromocytoma, carcinoma or neuroblastoma, adrenal calcification is their "fellow traveler".
It has no symptoms of its own, so the main signs of adrenal insufficiency are observed: general weakness, dizziness, increased skin pigmentation, poor appetite and weight loss, problems with bowel function, myalgia, numbness of the skin, increased irritability, etc.
 [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
[ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ]
Calcification of the liver
Whatever the causes of liver calcification, as in the case of other internal organs, the symptoms of calcific dystrophy will be within the framework of the clinical picture of hepatocyte damage. Therefore, there may be digestive disorders (due to decreased bile production), weight loss, pain in the hypochondrium (on the right), and bitter belching.
In most cases, calcification of the spleen is atherocalcinosis of the splenic artery or partial calcification of a hamartoma formed in the organ parenchyma, which does not manifest itself in any way and is discovered by chance.
Gallbladder calcification
According to gastroenterologists, calcification of the gallbladder has two main causes: chronic inflammation (cholecystitis) and oncology (carcinoma). In the case of cholecystitis, often accompanied by cholelithiasis, the degree of calcium dystrophy is so high that the walls of the bladder resemble porcelain in hardness and fragility, and doctors even call such a gallbladder porcelain. In this case, patients complain of abdominal pain (after each meal), nausea and vomiting.
Calcification of the pancreas
Most often, focal calcification of the pancreas develops at the site of damage and death of its acinar cells, which are replaced by fibrous or fatty tissue - in the chronic form of pancreatitis. Then pancreatitis is called calcifying, but symptoms of chronic pancreatitis appear. If there are cysts or pseudocysts in the pancreas, they can also contain calcifications.
Thyroid calcification
When the thyroid gland is enlarged (goiter), calcification occurs due to alteration and proliferation of thyrocytes - cells of its tissue. If the goiter type is colloid, then during its growth, due to deterioration of tissue trophism, the cells die, and the areas of necrosis become calcified, often with ossification.
Thyroid calcification in the presence of a cyst in it manifests itself only if its size is significant. And then symptoms of goiter are noted in the form of pain in the neck and headaches; a sensation of a foreign body in the throat, a sore throat and coughing; general weakness and bouts of nausea.
Calcification of lymph nodes
Lymph nodes are scattered throughout the body, and calcification of the lymph nodes can be of various localizations - with lymphadenitis, lymphocytic leukemia, lymphogranulomatosis, tuberculosis of the lymph nodes.
Calcareous dystrophy may affect enlarged or inflamed lymph nodes in people with rheumatoid arthritis, scleroderma, vasculitis, Sharp's syndrome, and other systemic collagenoses (congenital and acquired).
In the lymph nodes located in the chest, calcifications are formed during pulmonary tuberculosis, chronic pneumoconiosis, and sarcoidosis.
 [ 54 ], [ 55 ], [ 56 ], [ 57 ], [ 58 ], [ 59 ]
[ 54 ], [ 55 ], [ 56 ], [ 57 ], [ 58 ], [ 59 ]
Calcinosis in women
According to some data, calcification of the mammary glands is detected during mammography in at least 10% of women of childbearing age with fibrosis of the mammary glands, fibroadenomas and fibrocystic mastopathy, as well as in almost half of those over fifty. More information in the material - Calcifications in the mammary gland.
In a quarter of the women examined, gynecologists detect calcified myomatous nodes - myoma calcification, which produces the same symptoms as a regular myoma: pressure in the pelvic area, frequent urination and constipation, pain in the lower abdomen and lower back, longer and more intense menstruation.
With any ovarian pathology – adnexitis, polycystic and solitary cysts, malignant cilioepithelial cystoma or carcinoma – there may be ovarian calcification, the manifestation of which is limited to the symptoms of adnexitis.
A separate problem is calcinosis during pregnancy. According to clinical studies, to minimize the risk of developing nephropathy of pregnancy, accompanied by increased blood pressure (preeclampsia), the daily dose of calcium supplements from the middle of the second trimester can be 0.3-2 g. However, calcium is necessary not only for this, read - Calcium during pregnancy. And its intake by pregnant women who are not at risk of preeclampsia should not exceed 1.2 g per day (with a dose outside pregnancy - 700-800 mg).
Pregnant women are advised to take calcium so that it is enough to form the baby's skeleton, and so that the mother's body does not suffer. But thanks to a whole complex of hormones, the body of healthy women during pregnancy adapts to provide the fetus with calcium not by releasing it from the bone matrix. Compensatory mechanisms are activated: during gestation, the absorption of this macroelement from food products increases, the reabsorption of Ca in the intestine increases, its excretion through the kidneys and content in the blood decreases, the production of parathyroid hormone and calcitonin hormones, as well as calcitriol, increases.
If additional intake of calcium preparations disrupts the natural regulation of mineral metabolism, then calcinosis during pregnancy is possible, which affects the excretory system, which is working in an enhanced mode, with the development of nephrocalcinosis.
Not only the expectant mother may suffer: with an excess of calcium in the newborn's body, the fontanelle closes too early, and this increases intracranial pressure and interferes with the normal development of the brain. In children of the first year of life, due to the acceleration of ossification (ossification) of porous bone tissue, the process of its replacement with lamellar bone tissue is disrupted, and the child's growth slows down.
One of the complications of pregnancy is considered to be calcification of the placenta, although accumulations of insoluble calcium salts in the tissues of the maternal side of the full-term (mature) placenta are detected in almost half of cases of successful resolved pregnancy, that is, they cannot be considered a pathology. In other cases, calcifications are formed either due to premature maturation of the placenta, or due to endocrine pathology or the presence of risk factors for the development of calcification in the mother.
Calcifications in the immature placenta (before 27-28 weeks of pregnancy) can worsen its blood supply and provoke fetal hypoxia, delayed prenatal development, congenital pathologies and anomalies, and cause premature birth - everything depends on the maturity of the placenta and the level of calcareous dystrophy.
In obstetrics, based on the results of ultrasound examination from the 27th to the 36th week, grade 1 placental calcification is determined (grade 1 placental calcification) – in the form of individual microcalcifications. Grade 2 placental calcification – from the 34th to the 39th week – means the presence of calcifications visualized without additional magnification. And with grade 3 placental calcification (which is determined from the 36th week), numerous foci of calcific dystrophy are detected.
In this case, grade 2 placental calcification at 27-36 weeks or the presence of microcalcifications before the 27th week of pregnancy is of particular concern.
 [ 60 ], [ 61 ], [ 62 ], [ 63 ], [ 64 ]
[ 60 ], [ 61 ], [ 62 ], [ 63 ], [ 64 ]
Calcinosis in men
Prostate calcification may occur due to hyperplasia, adenoma or adenocarcinoma of the prostate gland, as well as due to its diffuse changes associated with age-related involution. For more details, see the material - Diffuse changes in the prostate gland.
Calcification of the scrotum - with pain in the groin area - is possible with chronic orchitis, scleroderma, sebaceous gland cysts, after injuries, and also in older men with age-related degeneration of genital tissues.
Focal or diffuse calcification of the testicles is associated with inflammatory processes of an infectious nature, in particular, tuberculosis, epididymitis or rhoepididymitis, the presence of teratoma or oncology and can manifest itself as discomfort in the groin (due to compaction of the testicular structure) and attacks of pain.
 [ 65 ], [ 66 ], [ 67 ], [ 68 ], [ 69 ], [ 70 ]
[ 65 ], [ 66 ], [ 67 ], [ 68 ], [ 69 ], [ 70 ]
Calcinosis in children
Most of the above-mentioned causes and risk factors for dystrophic calcification also cause calcification in children, so specialists pay attention to those diseases that lead to the manifestation of calcification in childhood, sometimes in infants. Such pathologies include:
- Wolman disease - with diffuse calcifications of both adrenal glands in newborns;
- congenital toxoplasmosis - causes focal calcification in the cortex, subcortex or brainstem. Surviving children develop atrophy of the optic nerves, hydrocephalus and a number of endocrinopathies; they lag behind in development - physical, mental and intellectual;
- Conradi-Hünermann syndrome or congenital calcifying chondrodystrophy, in which calcifications form in the area of the articular cartilage of the epiphyses of the tubular bones of the upper and lower extremities;
- congenital idiopathic arterial calcification;
- Albright's syndrome (localization of Ca deposition - subcutaneous soft tissues, mucous membrane of the eyes and cornea, muscle tissue, arterial walls, myocardium, renal parenchyma);
- Darier's pseudoxanthoma elasticum (with the formation of self-resolving nodular or plaque-like calcifications of the skin);
- hereditary oxalosis, causing diffuse renal calcification (calcifications consist of calcium oxalate) with severe renal failure and calcification of the joints. The disease progresses and leads to growth retardation.
Forms
According to the nature of the spread of pathological calcium accumulation in tissues, segmental - focal calcinosis and diffuse or diffuse calcinosis are distinguished. This process can also be intracellular, extracellular and mixed.
And depending on the pathogenetic features, such types of calcinosis are distinguished as metastatic, dystrophic and metabolic (or interstitial), the pathogenesis of which is not fully understood. Therefore, foreign endocrinologists do not consider metabolic calcinosis as a separate type, considering it a synonym for metastatic, and associate it with a violation of the functions of the blood buffer system in combination with an increased level of phosphates in the blood.
Metastatic calcinosis (in the sense of formation of pathological foci of calcium salt deposition) is determined only with increased calcium levels in the blood plasma. In most cases, this is moderate calcinosis affecting tissues with an alkaline reaction of the extracellular fluid and the content of polyanionic components that actively "catch" and firmly "hold" calcium cations. Among such tissues: acidic glycosaminoglycans of elastin, vascular endothelial collagen and skin reticulin; chondroitin sulfates of ligaments, cartilage, periarticular capsules, as well as heparan sulfate proteoglycans of the extracellular matrix of the tissues of the liver, lungs, heart membranes, etc.
Dystrophic calcification is local (focal) in nature and does not depend on hypercalcemia. Calcifications "capture" cells damaged by free radicals and areas of inflamed or atrophied tissue, foci of autolysis or necrosis, granulomas and cystic formations. The following are subject to dystrophic calcification: heart valves and myocardium (in the area of the post-infarction scar or in the presence of myocarditis); lungs and pleura (affected by tuberculosis mycobacteria or other pathogenic microorganisms); vascular walls (especially in the presence of atherosclerotic plaques and thrombi); epithelial lining of the renal tubules; fibrous nodes in the uterus or mammary glands, as well as in various structures of other organs in comorbid diseases.
For example, the dystrophic type includes calcinosis in scleroderma, an autoimmune disease of connective tissue with increased collagen synthesis and pathological changes in the skin, subcutaneous tissue and thickening of the capillary walls.
Complications and consequences
Any disturbance of mineral metabolism can have serious consequences and complications that negatively affect the condition and functioning of individual systems and organs. What is the danger of calcification?
Vascular calcification or atherocalcinosis disrupts the circulatory system and leads to persistent ischemia, and when calcium deposits are localized on the walls of leg vessels, tissue ischemia develops into their necrosis. Complications of calcific dystrophy of the walls of the thoracic aorta (and aortic valve) can include not only chronic heart failure, but also infarction. An abdominal aortic aneurysm with its rupture and fatal outcome can be a consequence of calcification of the walls and persistent stenosis of this vessel.
Calcifications disrupt the functions of the mitral valve due to its prolapse, which is complicated by blood stagnation in the pulmonary circulation, the development of cardiac asthma and heart failure.
If soft tissue calcification foci are localized near bones, they can fuse with the bone, which leads to limb deformation. When calcification affects the joints, the reduced ability to move can force a person to use a wheelchair.
 [ 80 ], [ 81 ], [ 82 ], [ 83 ], [ 84 ], [ 85 ], [ 86 ], [ 87 ]
[ 80 ], [ 81 ], [ 82 ], [ 83 ], [ 84 ], [ 85 ], [ 86 ], [ 87 ]
Diagnostics calcinosis
Calcite deposits in the tissues of internal organs, in the structures of the brain, on the walls of blood vessels, in joints, in lymph nodes and glands can only be detected by visualization methods, i.e. instrumental diagnostics come first: X-ray and scintigraphy; ultrasound examination, computed tomography and magnetic resonance imaging of the corresponding organs; electroencephalography, electro and echocardiography; osteoscintigraphy and osteodensitometry of bones; angiography, duplex angioscanning and ultrasound Dopplerography of vessels; endoscopic examination of cavity organs, etc.
Diagnosis of calcification involves laboratory tests:
- general blood test;
- analysis of the level of total and ionized calcium in the blood;
- blood tests for magnesium and phosphorus, cholesterol and sugar, urea and bilirubin; residual and C-reactive protein, alkaline phosphase, creatinine, amylase, aminotransferases;
- blood tests for levels of calcitonin, calcitriol, parathyroid hormone, and cortisol;
- urine test for calcium, phosphorus and oxalates.
Differential diagnosis
The list of diseases that should be excluded when detecting calcification is so extensive that its differential diagnosis is often carried out with the involvement of doctors of various specialties and the appointment of additional examination.
Treatment calcinosis
Regarding the methods currently used to treat calcinosis, it should be noted that the therapy of metabolic disorders takes into account their etiology and is aimed at the underlying disease, such as a malignant tumor, renal failure or hypercholesterolemia.
In particular, in case of atherosclerosis – to reduce LDL in the blood – statins are prescribed: Lovastatin (Mevacor), Simvastatin (Simgal), Rosuvastatin (Rozart, Rosucard, Tevastor), etc.
To reduce calcium reabsorption by the kidneys, it is forcibly removed from the body by shock courses of loop diuretics, most often Furosemide (other trade names are Furozan, Lasix, Uritol) - in tablets or parenterally; the doctor determines the dosage individually, taking into account the state of the cardiovascular system (since the drug also removes sodium, potassium and magnesium). In this case, the amount of liquid consumed should be increased to at least two liters per day.
Intestinal calcium binding is inhibited by glucocorticosteroids: intravenous injections of Methylprednisolone are prescribed (125 mg once a day for 10 days); intramuscular administration of Kenalog (Triamcinolone) - one injection daily (40-80 mg), the course of treatment is 14 days. Hypercalcemia associated with oncology responds especially well to steroid treatment.
The level of calcium in the blood is also reduced by drugs from the calcimimetics group: Cinacalcet (Mimpara, Sensipar) and Etelcalcetide (Pasarbiv), as well as biophosphonates – Pamidronate (Pamidria, Pamiredin, Pamired) and sodium ibandronate (Boniva).
There are drugs for cleaning vessels from calcification: EDTA sodium (sodium ethylenediaminetetraacetate, disodium endrat, Trilon B) and sodium thiosulfate (sodium hyposulfite). EDTA sodium is administered at 200-400 mg (intravenously by drip) once a day for three to five days. Sodium thiosulfate in the form of a solution is taken orally (2-3 g) once a day. Side effects include nausea, vomiting, diarrhea, muscle spasms.
Today, treatment of calcinosis with magnesium is an obligatory component of complex therapy of this pathology. Preparations containing Mg – Magnesium hydroxide, Magnesium lactate, Magnesium citrate (Magnesol), Magnikum, Magne B6 (Magvit B6), etc. – reduce the activity of parathyroid hormone and block the deposition of insoluble calcium salts.
It is also recommended to take vitamins B6, E, K1, PP (nicotinic acid).
Physiotherapy treatment
The objective of physiotherapeutic procedures prescribed in cases of calcification of bones, joints and muscles is to improve blood circulation and tissue trophism, as well as relieve pain. For this purpose, electrophoresis with drugs; UHF, microwave and magnetic therapy; applications of ozokerite, paraffin, sulphide mud; balneotherapy (treatment with baths), etc. are carried out.
Folk remedies
No recipe offered by folk remedies will help with calcifications in the lungs, basal ganglia of the brain, kidneys or pancreas.
Almost all folk remedies, including herbal treatment, are used for one purpose - to reduce cholesterol levels so that it does not settle on the walls of blood vessels and lead to atherosclerosis. Read the article - Treatment of high cholesterol, there is a section dedicated to folk remedies. Let's add to the remedies listed there a decoction or water infusion of golden mustache and powder from dried dandelion roots.
By the way, garlic is also used for calcification "from cholesterol". In addition to the well-known alcohol tincture of garlic, the dose of which is increased by one drop at each dose, a mixture of grated garlic with nut oil (1:3) and lemon juice is made. This remedy also reduces the level of glucose in the blood in diabetes and promotes the resorption of blood clots, which can also calcify.
They say that brown seaweed (laminaria) helps with calcinosis – thanks to its high magnesium content (170 mg per 100 g). However, it also contains a lot of calcium: 200 mg per 100 g. And on the pharmacy packaging of dry kelp it is indicated that it can be used for constipation.
 [ 94 ], [ 95 ], [ 96 ], [ 97 ], [ 98 ], [ 99 ] , [ 100 ], [ 101 ]
[ 94 ], [ 95 ], [ 96 ], [ 97 ], [ 98 ], [ 99 ] , [ 100 ], [ 101 ]
Surgical treatment
Large calcifications in the knee, shoulder or elbow joint can be removed surgically. Surgical treatment is performed for vascular calcification: stents are installed, the vessel lumen is bougienaged or expanded using balloon angioplasty. A prosthesis is installed instead of a valve or articular cartilage hardened by calcium.
Soft tissue calcifications are removed endoscopically, but sometimes partial or complete resection of the organ (ovary, prostate, gallbladder) is not excluded – in case of complete loss of its functions or the threat of irreversible consequences.
Nutrition for calcinosis
A special diet for calcification, including a diet for calcification of the vessels, aorta or gallbladder, has not been developed.
Therefore, you just need to know what foods you should not eat if you have aortic calcification.
Among the recommendations for excluding or limiting certain foods to the maximum extent, two points are noted - the presence of calcium and vitamin D:
Foods high in calcium: milk and all dairy products (primarily cheese and feta cheese), beans and soybeans, sesame, almonds, hazelnuts, sunflower seeds, cabbage, lettuce, carrots, radishes, celery, green onions, basil, pumpkin, melon, green olives, cherries, raspberries, dried apricots, raisins, figs, dates.
Due to the high content of vitamin D, you should exclude egg yolk, beef and cod liver, fatty sea fish from your diet. It is better to eat non-yeast bread.
But foods rich in magnesium should be present in the menu, and these are porcini mushrooms (dried), walnuts, pistachios, peanuts, pumpkin seeds, wheat bran.
Add to this vitamin K-containing grapes, avocados and kiwis, as well as all the usual grains, which contain phytin (which inhibits the absorption of calcium).
Prevention
Prevention of metabolic disorders, as usual, does not have clearly formulated and scientifically substantiated recommendations. But proper nutrition for calcinosis, despite the leveling of its role by some specialists, is so far the only specific factor.
 [ 102 ], [ 103 ], [ 104 ], [ 105 ], [ 106 ], [ 107 ], [ 108 ]
[ 102 ], [ 103 ], [ 104 ], [ 105 ], [ 106 ], [ 107 ], [ 108 ]
Forecast
In most cases, the prognosis for calcinosis is not very encouraging: few people succeed in curing it, that is, establishing the correct calcium metabolism in the body, in the presence of underlying diseases.
And calcification of the aortic valve and heart, coronary calcification have an unfavorable prognosis and can lead to sudden death.

