Medical expert of the article
New publications
Instrumental methods of cardiac examination
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Phonocardiography of the heart allows recording heart sounds, tones and murmurs on paper. The results of this study are similar to cardiac auscultation, however, it should be borne in mind that the frequency of sounds recorded on the phonocardiogram and perceived during auscultation do not fully correspond to each other. Some murmurs, for example, high-frequency diastolic murmur at the V point in aortic insufficiency, are better perceived during auscultation. Simultaneous recording of PCG, artery sphygmogram and ECG allows measuring the duration of systole and diastole to assess the contractile function of the myocardium. The duration of the intervals QI tone and II tone - the click of the mitral valve opening allows assessing the severity of mitral stenosis. Recording ECG, PCG and the curve of the pulsation of the jugular vein allows calculating the pressure in the pulmonary artery.
X-ray examination of the heart
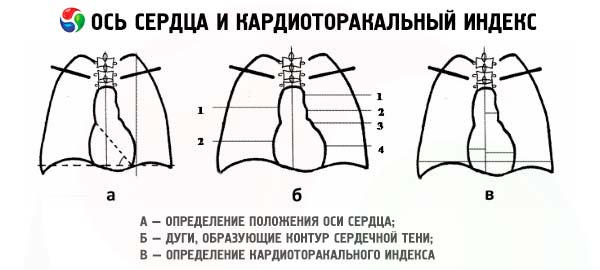
During chest X-ray examination, the shadow of the heart surrounded by the air-filled lungs can be carefully examined. Usually, 3 projections of the heart are used: anterior-posterior or direct, and 2 oblique, when the patient stands to the screen at an angle of 45°, first with the right shoulder forward (I oblique projection), then - the left (II oblique projection). In the direct projection, the shadow of the heart on the right is formed by the aorta, superior vena cava and right atrium. The left contour is formed by the aorta, pulmonary artery and conus of the left atrium and, finally, the left ventricle.
In the first oblique position, the anterior contour is formed by the ascending aorta, the pulmonary cone, and the right and left ventricles. The posterior contour of the heart shadow is formed by the aorta, the left and right atrium. In the second oblique position, the right contour of the shadow is formed by the superior vena cava, the ascending aorta, the right atrium, and the right ventricle, and the posterior contour is formed by the descending aorta, the left atrium, and the left ventricle.
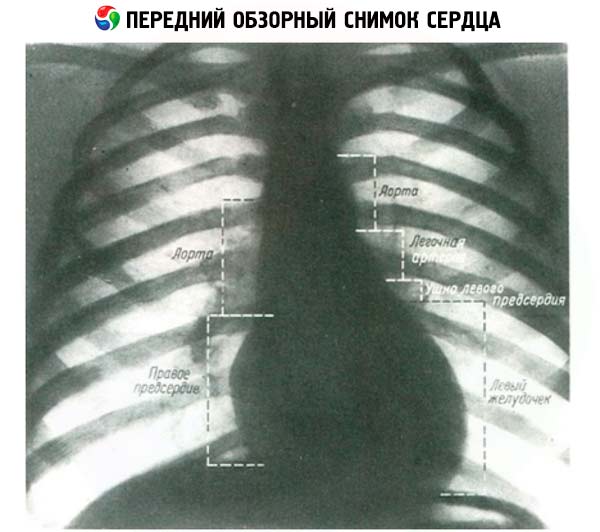
During a routine examination of the heart, the dimensions of the heart chambers are assessed. If the transverse dimension of the heart is more than half the transverse dimension of the chest, this indicates the presence of cardiomegaly. Enlargement of the right atrium causes a shift in the right border of the heart, while enlargement of the left atrium shifts the left contour between the left ventricle and the pulmonary artery. Posterior enlargement of the left atrium is detected when barium passes through the esophagus, which reveals a shift in the posterior contour of the heart. Enlargement of the right ventricle is best seen in the lateral projection by the narrowing of the space between the heart and the sternum. Enlargement of the left ventricle causes a shift in the lower part of the left contour of the heart outward. Enlargement of the pulmonary artery and aorta can also be recognized. However, it is often difficult to determine the enlarged section of the heart, since the heart may rotate around its vertical axis. An X-ray clearly shows the enlargement of the heart chambers, but with thickening of their walls, a change in configuration and displacement of the borders may be absent.
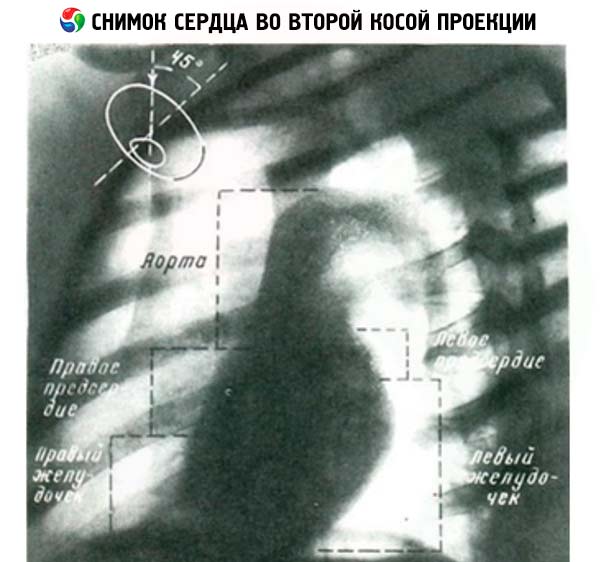
Calcification of cardiac structures may be an important diagnostic feature. Calcified coronary arteries usually indicate severe atherosclerotic lesions. Aortic valve calcification occurs in almost 90% of patients with aortic stenosis. However, in the anteroposterior image, the projection of the aortic valve is superimposed on the spine and the calcified aortic valve may not be visible, so it is better to determine the calcification of the valves in oblique projections. Pericardial calcification may be of important diagnostic value.
The condition of the lungs, especially their vessels, is important in diagnosing heart disease. Pulmonary hypertension may be suspected when the large branches of the pulmonary artery are dilated, while the distal sections of the pulmonary artery may be normal or even reduced in size. In such patients, pulmonary blood flow is usually reduced and the pulmonary veins are usually normal in size or reduced. In contrast, when pulmonary vascular blood flow is increased, for example, in patients with certain congenital heart defects, there is an increase in both the proximal and distal pulmonary arteries and an increase in the pulmonary veins. A particularly pronounced increase in pulmonary blood flow is observed with a shunt (blood discharge) from left to right, for example, with an atrial septal defect from the left atrium to the right.
Pulmonary venous hypertension is detected in mitral stenosis, as well as in any left ventricular heart failure. In this case, the pulmonary veins in the upper parts of the lung are especially dilated. As a result of the pressure in the pulmonary capillaries exceeding the oncotic pressure of the blood in these areas, interstitial edema occurs, which is radiologically manifested by the erasure of the edges of the pulmonary vessels, an increase in the density of the lung tissue surrounding the bronchi. With the increase of pulmonary congestion with the development of alveolar edema, bilateral expansion of the roots of the lungs occurs, which begin to resemble a butterfly in appearance. Unlike the so-called cardiac edema of the lungs, when they are damaged, associated with an increase in the permeability of the pulmonary capillaries, the radiological changes are diffuse and more pronounced.
Echocardiography
Echocardiography is a method of examining the heart based on the use of ultrasound. This method is comparable to X-ray examination in its ability to visualize the structures of the heart, evaluate its morphology, and contractile function. Thanks to the ability to use a computer, record an image not only on paper, but also on videotape, the diagnostic value of echocardiography has increased significantly. The capabilities of this non-invasive method of examination are currently approaching the capabilities of invasive X-ray angiocardiography.
The ultrasound used in echocardiography has a much higher frequency (compared to the frequency accessible to hearing). It reaches 1-10 million oscillations per second, or 1-10 MHz. Ultrasound oscillations have a short wavelength and can be obtained in the form of narrow beams (similar to light beams). When reaching the boundary of media with different resistance, part of the ultrasound is reflected, and the other part continues its path through the medium. In this case, the reflection coefficients at the boundary of different media, for example, "soft tissue - air" or "soft tissue - liquid", will differ. In addition, the degree of reflection depends on the angle of incidence of the beam on the interface surface of the media. Therefore, mastering this method and its rational use require a certain skill and time.
To generate and record ultrasonic vibrations, a sensor containing a piezoelectric crystal with electrodes attached to its edges is used. The sensor is applied to the chest surface in the area of the heart projection, and a narrow ultrasound beam is directed at the structures being studied. Ultrasonic waves are reflected from the surfaces of structural formations that differ in density and return to the sensor, where they are recorded. There are several echocardiography modes. One-dimensional M-echocardiography produces an image of the heart structures with a sweep of their movement over time. In the M-mode, the resulting image of the heart allows one to measure the thickness of the walls and the size of the heart chambers during systole and diastole.
Two-dimensional echocardiography allows obtaining a two-dimensional image of the heart in real time. In this case, sensors are used that allow obtaining a two-dimensional image. Since this study is conducted in real time, the most complete method of recording its results is video recording. Using different points at which the study is performed and changing the direction of the beam, it is possible to obtain a fairly detailed image of the heart structures. The following sensor positions are used: apical, suprasternal, subcostal. The apical approach allows obtaining a section of all 4 chambers of the heart and the aorta. In general, the apical section is in many ways similar to an angiographic image in the anterior oblique projection.
Doppler echocardiography allows one to evaluate blood flow and the turbulence that occurs with it. The Doppler effect is that the frequency of the ultrasound signal when reflected from a moving object changes proportionally to the speed of the object being located. When an object (for example, blood) moves toward the sensor generating ultrasound pulses, the frequency of the reflected signal increases, and when reflected from a moving object, the frequency decreases. There are two types of Doppler studies: continuous and pulsed Doppler cardiography. This method can be used to measure the speed of blood flow in a specific area located at a depth of interest to the researcher, for example, the speed of blood flow in the supravalvular or subvalvular space, which changes with various defects. Thus, recording blood flow at certain points and in a certain phase of the cardiac cycle allows one to fairly accurately evaluate the degree of valve insufficiency or stenosis of the orifice. In addition, this method also allows one to calculate cardiac output. Currently, Doppler systems have appeared that allow recording Doppler echocardiograms in real time and color image synchronously with a two-dimensional echocardiogram. In this case, the direction and speed of the flow are depicted in different colors, which facilitates the perception and interpretation of diagnostic data. Unfortunately, not all patients can be successfully examined using echocardiography, for example, due to severe pulmonary emphysema, obesity. In this regard, a modification of echocardiography has been developed, in which registration is performed using a sensor inserted into the esophagus.
Echocardiography allows, first of all, to evaluate the sizes of the heart chambers and hemodynamics. With the help of M-echocardiography, it is possible to measure the sizes of the left ventricle during diastole and ristol, the thickness of its posterior wall and interventricular septum. The obtained sizes can be converted into volume units (cm 2 ). The left ventricular ejection fraction is also calculated, which normally exceeds 50% of the end-diastolic volume of the left ventricle. Doppler echocardiography allows to evaluate the pressure gradient through the narrowed opening. Echocardiography is successfully used to diagnose mitral stenosis, and a two-dimensional image allows to determine the size of the mitral opening quite accurately. In this case, concomitant pulmonary hypertension and the severity of the right ventricular lesion, its hypertrophy are also assessed. Doppler echocardiography is the method of choice for assessing regurgitation through the valve openings. Echocardiograms are especially valuable in recognizing the cause of mitral regurgitation, in particular in diagnosing mitral valve prolapse. In this case, the posterior displacement of the mitral valve leaflet may be visible during systole. This method also allows one to assess the cause of the narrowing that occurs on the path of blood ejection from the left ventricle into the aorta (valvular, supravalvular and subvalvular stenosis, including obstructive cardiomyopathy). The method allows one to diagnose hypertrophic cardiomyopathy with a high degree of accuracy with various locations, both asymmetric and symmetric. Echocardiography is the method of choice in diagnosing pericardial effusion. A layer of pericardial fluid may be visible behind the left ventricle and in front of the right ventricle. With a large effusion, compression of the right half of the heart is visible. It is also possible to detect a thickened pericardium and pericardial constriction. However, some structures around the heart, such as epicardial fat, may be difficult to distinguish from the thickened pericardium. In this case, methods such as computed tomography (X-ray and nuclear magnetic resonance) provide a more adequate image. Echocardiography allows one to see papillomatous growths on the valves in infective endocarditis, especially when the vegetation (due to endocarditis) is more than 2 mm in diameter. Echocardiography allows one to diagnose atrial myxoma and intracardiac thrombi, which are well detected in all examination modes.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ]
Radionuclide examination of the heart
The study is based on the introduction of albumin or erythrocytes with a radioactive label into a vein. Radionuclide studies allow for the evaluation of the contractile function of the heart, perfusion and ischemia of the myocardium, as well as the detection of areas of necrosis in it. Equipment for radionuclide studies includes a gamma camera in combination with a computer.
Radionuclide ventriculography is performed with intravenous injection of technetium-99 labeled red blood cells. This produces an image of the cavity of the heart chambers and large vessels (to a certain extent similar to the data of cardiac catheterization with X-ray angiocardiography). The resulting radionuclide angiocardiograms allow one to evaluate the regional and general function of the left ventricle myocardium in patients with ischemic heart disease, evaluate ejection fractions, determine the function of the left ventricle in patients with heart defects, which is important for prognosis, and examine the condition of both ventricles, which is important in patients with congenital heart defects, cardiomyopathies, and arterial hypertension. The method also allows one to diagnose the presence of an intracardiac shunt.
Perfusion scintigraphy with radioactive thallium-201 allows assessing the state of coronary circulation. Thallium has a fairly long half-life and is an expensive element. Thallium injected into a vein is delivered to the myocardial cells with the coronary blood flow and penetrates the membrane of cardiac myocytes in the perfused part of the heart, accumulating in them. This can be recorded on a scintigram. In this case, a poorly perfused area accumulates thallium worse, and a non-perfused area of the myocardium appears as a "cold" spot on the scintigram. Such scintigraphy can also be performed after physical exertion. In this case, the isotope is administered intravenously during the period of maximum exertion, when the patient develops an attack of angina pectoris or changes in the ECG indicate ischemia. In this case, ischemic areas are detected due to their worse perfusion and lower accumulation of thallium in cardiac myocytes. Areas where thallium does not accumulate correspond to zones of cicatricial changes or fresh myocardial infarction. Thallium load scintigraphy has a sensitivity of approximately 80% and a specificity of 90% for detecting myocardial ischemia. It is important for assessing the prognosis in patients with coronary heart disease. Thallium scintigraphy is performed in different projections. In this case, left ventricular myocardial scintigrams are obtained, which are divided into fields. The degree of ischemia is assessed by the number of changed fields. Unlike X-ray coronary angiography, which demonstrates morphological changes in the arteries, thallium scintigraphy allows one to assess the physiological significance of stenotic changes. Therefore, scintigraphy is sometimes performed after coronary angioplasty to assess the function of the bypass.
Scintigraphy after the introduction of technetium-99 pyrophosphate is performed to identify the area of necrosis in patients with acute myocardial infarction. The results of this study are assessed qualitatively by comparison with the degree of absorption of pyrophosphate by bone structures that actively accumulate it. This method is important for the diagnosis of myocardial infarction in the case of an atypical clinical course and difficulties in electrocardiographic diagnosis due to impaired intraventricular conduction. After 12-14 days from the onset of infarction, signs of pyrophosphate accumulation in the myocardium are not recorded.
MR tomography of the heart
Nuclear magnetic resonance examination of the heart is based on the fact that the nuclei of some atoms, when in a strong magnetic field, themselves begin to emit electromagnetic waves that can be recorded. Using the radiation of various elements, as well as computer analysis of the resulting oscillations, it is possible to visualize well various structures located in soft tissues, including the heart. With this method, it is possible to clearly determine the structures of the heart at various horizontal levels, i.e. to obtain tomograms, and to clarify morphological features, including the size of the chambers, the thickness of the heart walls, etc. Using the nuclei of various elements, it is possible to detect foci of necrosis in the myocardium. By studying the radiation spectrum of elements such as phosphorus-31, carbon-13, hydrogen-1, it is possible to assess the state of phosphates rich in energy and study intracellular metabolism. Nuclear magnetic resonance in various modifications is increasingly used to obtain visible images of the heart and other organs, as well as to study metabolism. Although this method remains quite expensive, there is no doubt that it has great potential for use both in scientific research and in practical medicine.

