Medical expert of the article
New publications
Anovulatory menstrual cycle in women
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
If there is no ovulatory phase in a woman's menstrual cycle, it is defined as an anovulatory cycle.
In ICD-10, code N97.0 has female infertility associated with anovulation. And this is logical, since the absence of ovulation itself is not considered a disease, but a sign of pathology of the female reproductive system, which occurs in various conditions and diseases.
Epidemiology
According to statistics, 15% of women of reproductive age may have a menstrual cycle without ovulation; 50% of teenage girls have anovulatory cycles in the first two years after the onset of menstruation.
In young women, 75-90% of anovulation cases are the result of polycystic ovary syndrome; more than 13% of cases are due to hyperprolactinemia. Idiopathic chronic anovulation occurs in 7.5% of cases. [ 1 ], [ 2 ], [ 3 ]
Almost 30% of infertility cases are caused by an anovulatory cycle. [ 4 ]
Causes anovulatory cycle
The ovulatory and anovulatory cycles differ fundamentally: the first is a normal menstrual cycle with alternation of all phases (follicular or follicular, ovulatory and luteal); the second is abnormal, without the release of a mature oocyte from the follicle, that is, without ovulation, without the formation and involution of the corpus luteum and the release of luteinizing hormone from the pituitary gland.
It should be borne in mind that an anovulatory cycle can be not only pathological, but also physiological. In particular, it occurs during the first two years after menarche in girls; with a sharp change in the climate zone of residence or severe stress; during lactation after childbirth; after a miscarriage or stopping taking birth control pills, as well as after 45 years - due to fluctuations in hormone levels before the onset of menopause.
The main causes of pathological anovulatory cycle are hormonal disorders, which, in turn, can be caused by:
- polycystic ovary syndrome (PCOS);
- dysfunction of the ovaries in the presence of chronic inflammation - oophoritis;
- hyperanlrogenism;
- excessive production of prolactin by the pituitary gland - hyperprolactinemia;
- hyperestrogenism or, conversely, estrogen deficiency;
- dysfunction of the hypothalamic-pituitary system - gonadotropic insufficiency;
- imbalance of thyroid-stimulating hormones (thyroxine and triiodothyronine) in hyper or hypothyroidism;
- dysfunction of the adrenal cortex (hypocorticism), including its hormonally active tumor - androsteroma.
In addition, an excess of the quantitative norm of follicles - multifollicular ovaries - can also cause an anovulatory cycle, since the multifollicular structure of the ovaries prevents the maturation of follicles and, in addition, often leads to PCOS and the associated hormonal imbalance. [ 5 ]
More details in the publication – Causes, symptoms and diagnosis of anovulation
Depending on the etiology and hormonal state, specialists distinguish normogonadotropic normoestrogenic, hypergonadotropic hypooestrogenic and hypogonadotropic hypooestrogenic types of anovulatory cycle. [ 6 ]
Risk factors
The following factors significantly increase the risk of a cycle without ovulation:
- long-term use of oral contraceptives;
- hereditary or acquired insulin resistance leading to metabolic syndrome – with increased production of adrenocorticotropic hormone (ACTH) by the pituitary gland and hyperandrogenism;
- overweight or underweight;
- the impact of frequent stress on hormonal levels;
- excessive physical activity (menstrual irregularities and amenorrhea are part of the so-called triad of female athletes);
- diseases of the uterus (endometriosis, fibroids, etc.);
- tumors of the ovaries, thyroid and parathyroid glands, pituitary gland or hypothalamus;
- adrenal insufficiency.
Pathogenesis
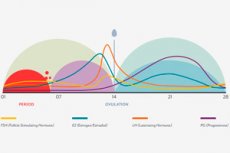
In all of the above-mentioned causes, including polycystic ovary syndrome with damage to their follicular apparatus, the pathogenesis of the absence of ovulation is associated with the fact that hormonal homeostasis is disrupted - the natural balance of sex steroids and gonadotropins: estradiol and estrone, androstenedione and testosterone, luteotropin and follitropin (luteinizing and follicle-stimulating hormones - LH and FSH), progesterone, prolactin, gonadotropin-releasing hormone, which are produced by the ovaries and corpus luteum, adrenal cortex and hypothalamic-pituitary system. [ 7 ], [ 8 ], [ 9 ]
The following publications will help you understand the positive and negative relationships between sex and gonadotropic hormones in more detail:
Symptoms anovulatory cycle
With anovulation, the first signs are menstrual cycle irregularities, when it is shorter than 21 days or longer than 35 days, or the length of the cycles changes from month to month. Although menstruation during an anovulatory cycle (which many gynecologists consider menstrual-like bleeding) may occur, it is less regular and longer. About 20% of women do not have periods, that is, amenorrhea is observed, and in 40% of cases, rare and short menstruations are observed (if the intervals between menstruations increase by more than 35 days, this is defined as oligomenorrhea). [ 10 ]
In addition, the following symptoms are noted:
- in the second phase, the basal temperature during an anovulatory cycle does not increase;
- there may be spotting in the middle of the cycle;
- weight gain and facial hair growth (often associated with PCOS and hypocorticism);
- Heavy bleeding may occur during an anovulatory cycle, which is associated with insufficient levels of FSH and LH and a deficiency of progesterone - hormones that neutralize the effect of estradiol on the uterine mucosa. This type of bleeding is called breakthrough estrogen or metrorrhagia, and can be confused with menstruation.
- cervical mucus - cervical mucus during an anovulatory cycle may become thicker and thinner for a few days, indicating increased estrogen levels in anticipation of ovulation, but then it becomes thick again.
If you have an anovulatory cycle and your breasts hurt, this is an indicator of low progesterone levels. About 20% of women with ovulation problems do not experience breast pain (mastodynia).
But the endometrium in a chronic anovulatory cycle, especially in women with PCOS, undergoes hyperplasia, that is, growth and thickening, due to the lack of the inhibitory effect of progesterone on the stimulation of the mucous membrane of the uterine cavity by estrogen.
Complications and consequences
The main consequences and complications of a cycle without an ovulatory phase include:
- infertility, since pregnancy does not occur after an anovulatory cycle (and even when trying to get pregnant with the help of IVF, a donor egg is used);
- early perimenopause and menopause;
- anemia;
- decreased bone density;
- cancerous degeneration of the endometrium.
Diagnostics anovulatory cycle
It seems that in the absence of menstruation or irregularities in their periodicity, the diagnosis of an anovulatory cycle is very simple. But this is far from the case in all cases. [ 11 ]
To diagnose an anovulatory cycle, women undergo blood tests for levels of estrogen, progesterone, luteinizing and follicle-stimulating hormones, prolactin, 17a-hydroxyprogesterone, dihydrotestosterone, ACTH, thyroid hormones, and insulin. [ 12 ]
Instrumental diagnostics are carried out:
When performing a high-resolution transvaginal ultrasound examination, the anovulatory cycle is identified by ultrasound signs based on the absence of visualization of the protrusion into the ovarian cortex of the dominant (preovular) follicle and vascularization of its wall (perifollicular vascular perfusion).
The task that differential diagnostics solves based on the results of hormonal tests is to determine the underlying cause of anovulatory disorders. [13 ]
Who to contact?
Treatment anovulatory cycle
Taking into account the cause of the anovulatory cycle, its treatment is also carried out.
Medications often prescribed to induce ovulation include the estrogen antagonists clomiphene (Clomid, Clostilbegyt) or tamoxifen (Nolvadex), and the aromatase inhibitor letrozole (Femara).
In case of dysfunction of the hypothalamic-pituitary system, it promotes the development of follicles and stimulates ovulation. Follitropin alpha (by injection) – 75-150 IU once a day (during the first seven days of the cycle). This drug is contraindicated in case of ovarian cysts and hypertrophy, tumors of the hypothalamus, pituitary gland, uterus or mammary glands. Its side effects include nausea, vomiting, abdominal and joint pain, ascites and the formation of venous thrombi. [ 14 ]
Also, the injectable drug Puregon (Follitropin beta) can compensate for the FSH deficiency.
Progesterone analogues Dydrogesterone (Duphaston) and Utrozhestan are used in anovulatory cycles with a deficiency of this hormone to stimulate the synthesis of pituitary gonadotropins (LH and FSH) and the luteal phase. The dosage is determined by the doctor, for example, the daily dose of Utrozhestan is 200-400 mg, it is taken for 10 days (from the 17th to the 26th day of the cycle). This drug is contraindicated in deep vein thrombosis, liver failure, breast cancer. And side effects include headache, sleep disturbances, increased body temperature, nocturnal hyperglycemia, breast tenderness, vomiting, intestinal disorders. [ 15 ], [ 16 ], [ 17 ], [ 18 ]
In case of hyperprolactinemia, Bromocriptine (Parlodel) is used to reduce the production of prolactin by the pituitary gland. If the anovulatory cycle is associated with increased production of male hormones by the adrenal glands, corticosteroids are prescribed. [ 19 ]
Herbal treatment or phytotherapy to support ovulation is most often aimed at restoring hormonal balance. For this purpose, on the recommendation of a doctor, the following can be used: the herb and seeds of Tribulus terrestris; the herb and flowers of red clover; the root of wild yam; the root and rhizomes of Cimicifuga (black cohosh); linseed oil and evening primrose seed oil. Of particular note are the seeds, fruits and leaves of a tree-like shrub of the Lamiaceae family – Vitex chasteberry (another name is Chasteberry). Extracts from these parts of Vitex chasteberry increase dopamine activity in the brain, which leads to a decrease in the release of prolactin, as well as a normalization of the balance of progesterone and estrogen and an increase in LH levels.
Also read the article – Treatment of anovulation
Prevention
It is possible to prevent an anovulatory cycle if you have weight problems: if your body mass index increases, you need to lose the extra weight; if you have lost a significant amount of weight, you need to gain the missing kilograms. [ 20 ]
For women's health, it is necessary to maintain a healthy lifestyle and eat rationally. See - Products for restoring hormonal balance
Forecast
Considering that ovulation can be restored with the help of appropriate drugs, [ 21 ] the prognosis for an anovulatory cycle is considered favorable in almost 90% of cases.

