Medical expert of the article
New publications
Melanoma
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Melanoma is a malignant neoplasm of the skin that develops from melanocytes - cells migrating in the early embryonic period from the neuroectoderm to the skin, eyes, respiratory tract and intestines.
Melanocytes can form distinctive "nests" from cells with different degrees of differentiation. Externally, the accumulations of melanocytes are manifested by nevi (birthmarks). Melanoma was first described in 1806 by Rene Laennec.
Epidemiology
The incidence in all age groups is currently about 14 cases per 100,000 population per year. At the same time, according to estimates of the National Cancer Institute, for the white population of the United States the probability of developing the disease is 1: 100. In blacks, this tumor is extremely rare, so its risk in this category is not defined.
Melanoma is extremely rare in children: its frequency is about 1% of the cases of this tumor in all age groups. The frequency of its development increases with age. Nevertheless, in children there are two peaks of incidence of this tumor: 5-7 and 11-15 years.
Causes of the melanoma
In the development of melanoma, there are two main predisposing factors - trauma and insolation. Both these types of actions provoke malignant degeneration of skin elements. This dictates the need for a planned removal of nevi from the areas where they are most traumatized by clothing and shoes, and also requires the refusal of excessive enthusiasm for sunbathing and sunbeds.
Other predisposing factors of malignant growth of the skin are belonging to the white race (the lighter the skin, the higher the risk), the presence of cases of this tumor in the family history, the presence of a large number of nevi on the skin, and for adults up to the age of 45 years. In comparison with constant insolation, shorter, but intense doses of insolation are more melano-dangerous.
As a preventive measure, it is most effective to reduce the residence time under the influence of direct sunlight and wearing headgear and clothing that closes the skin as much as possible, are less effective - sunscreen creams.
Symptoms of the melanoma
In 70% of cases melanoma develops from nevi, in 30% - on "clean" areas of the skin. The localization of the tumor can be any part of the body. Most often (50% of cases) it occurs on the skin of the extremities, somewhat less often (35%) - in the trunk region and least often (25%) on the head and neck.
How does melanoma look like?
- Surface spreading - develops from an already existing nevus, for several years has a slow growth rate. This is the most common form of malignant neoplasm.
- Nodal is a knot of loose consistency on the skin. It is often ulcerated, has fast growth rates. It is in 2nd place in frequency after surface spreading.
- Malignant lentigo (melancholic freckle Hutchinson) - similar to the surface spreading, is typical for the elderly. Usually localized on the face.
- Peripheral lentigo - affects the palms, soles of the feet, can be localized on the nail bed. The most characteristic for people who do not belong to the white race. The prognosis is usually unfavorable, since the tumor can remain undiagnosed before reaching a significant size.
There are three early and four late signs of melanoma.
Early signs:
- high growth rates;
- growth of one of the skin areas with its deformation:
- ulceration and spontaneous hemorrhage.
Late symptoms:
- the appearance of satellites (intradermal tumor screenings) around the primary tumor:
- increased regional lymph nodes (with metastases);
- tumor intoxication;
- visualization with the help of instrumental methods of distant metastases.
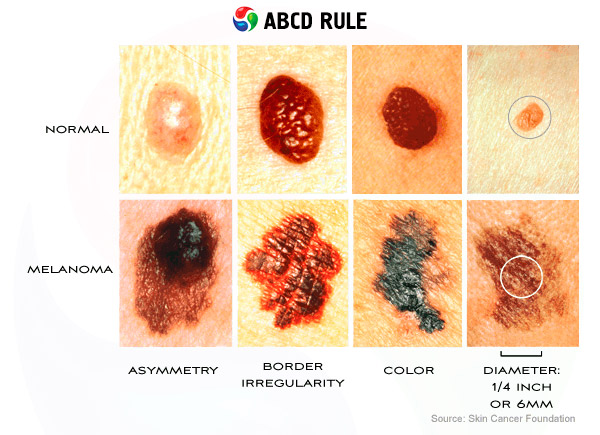
In English-speaking countries, the acronym ABCD is used to memorize signs of tumors:
- A (Assymetry) - asymmetry of the shape and distribution of the pigment. The letter "A" also means that the Appearance of the tumor must be evaluated.
- In (Borders) - the edges of the cancer often have an irregular star shape and bleed (Bleed).
- With (Change) - with any change in characteristics, the birthmark must be examined for malignant growth.
- D (Diameter) - the diameter of most melanomas is greater than 6 mm, although smaller lesions are not excluded.
Melanoma is characterized by lymphogenous metastasis with lesions, primarily regional lymph nodes and hematogenous metastasis with lesions of the lungs, brain, and other organs. The risk of metastaization increases with an increase in the thickness of the neoplasm and the depth of its invasion into the dermis and subcutaneous tissue.
Where does it hurt?
Stages
When assessing the primary tumor, the depth of invasion of the cancer into the skin and the underlying tissues matters. Clinical practice uses Clark's classification (Clark, 1969), which provides for five degrees of invasion.
- I degree of Clark invasion (melanoma in situ) - the cancer is located in the epithelium, not penetrating the basal membrane.
- II degree of invasion by Clark - the neoplasm penetrates the basal membrane and spreads into the papillary layer of the dermis.
- III degree of invasion by Clark - cancer spreads into the papillary layer of the dermis, while tumor cells accumulate at the border of papillary and reticular layers, not penetrating into the latter.
- IV degree of invasion by Clark - the neoplasm spreads into the reticular layer of the dermis.
- V degree of invasion by Clark - cancer extends to subcutaneous adipose tissue and other structures.
Breslow (1970) suggested evaluating the depth of penetration of melanoma into the skin and the underlying tissues along the thickness of the removed tumor. Both principles (Clark and Breslow) are combined in the classification proposed by the American Joint Committee on the Classification of Cancer (AJCCS) (it is recommended to give preference to the criteria for Breslow).
- Ia stage - the thickness is 0.75 mm and / or the degree of invasion according to Clark II (pT1), regional (N0) and distant (M0) metastases are absent.
- Ib stage - the thickness is 0.76-1.50 mm and / or the degree of invasion according to Clark III (pT2): N0. M0.
- IIa stage - thickness 1.51-4.00 mm and / or degree of invasion according to Clark IV (rTZ). N0. M0.
- IIb stage - a thickness of more than 4.00 mm and / or a degree of invasion according to Clark V (pT4); N0, MO.
- III stage - metastases to regional lymph nodes or metastases in-transit (satellites); any pT, N1 or N2, MO.
- IV stage - distant metastases: any pT. Any N. Ml.
Forms
There are four types of pigmented lesions on the skin.
- Melanoneopasnye: true pigmentary nevus, intradermal nevus, papillomas, warts, hairy nevus.
- Melaneopathic: border nevus, blue nevus, giant pigment nevus.
- On the border of malignancy: juvenile (mixed nevus, nevus Spitz) - does not give metastases, but has a tendency to recur.
- Malignant neoplasm is melanoma.
 [19]
[19]
Diagnostics of the melanoma
The diagnostic feature is a categorical prohibition of aspiration and incisional biopsy (partial excision of this tumor or a suspicious nevus). Such an intervention gives an impetus to intensive growth and metasgasation of the tumor. In relation to melanoma, only complete removal is possible within healthy tissues with subsequent histological examination. The method of pre-operative evaluation of the malignancy of education on the skin is thermography. In the presence of a bleeding, ulcerated tumor, it is possible to perform a print from its surface followed by a cytological examination.
Diagnosis of possible lymphogenous and hematogenous metastases is made according to the standard plan of examination of an oncological patient.
Compulsory diagnostic tests
- Complete physical examination with assessment of local status
- Clinical blood test
- Clinical analysis of urine
- Biochemical blood test (electrolytes, total protein, liver tests, creatinine, urea, lactate dehydrogenase, alkaline phosphatase, phosphoric-calcium metabolism)
- Coagulogram
- Thermography
- Ultrasound of the region of ultrasound of the organs of the abdominal cavity and retroperitoneal space
- Radiography of the chest cavity in five projections (spicy, two side, two oblique)
- ECG
- The final stage is the histological verification of the diagnosis. It is possible to make prints from the preparation for cytological examination.
 [24]
[24]
Additional diagnostic tests
- In the presence of an ulcerated bleeding tumor - a cytological examination of the impression from the surface of the tumor
- If there is a suspicion of lung metastasis - the chest wall of the thoracic cavity
- If there is a suspicion of metastases in the abdominal cavity - ultrasound, an abdominal cavity RCT
- If there is a suspicion of a metastasis in the brain - EchoEG and PKT of the brain
What do need to examine?
How to examine?
Differential diagnosis
Differential diagnosis of melanoma and non-malignant elements on the skin of a child is often difficult. Diagnostic criteria can be the rapid growth rates characteristic for this type of cancer, which outstrips the growth of the child, the irregular or dentate shape of the tumor's edges, often bleeding, the color change of the nevus upon its degeneration into a malignant neoplasm. The variability of the color of this tumor also complicates the diagnosis. In addition to the typical brown, its surface can have shades of blue, gray, pink, red or white.
Who to contact?
Treatment of the melanoma
In the treatment, the leading method is the radical surgical removal of melanoma - excision to the fascia within healthy tissues with a significant supply of unchanged skin along the periphery of the tumor. The reserve of healthy tissues along the periphery is selected depending on the thickness of the tumor: intraepithelial neoplasm - 5 mm; with a tumor thickness of up to 1 cm - 10 mm; more than 1 cm - 20 mm. When diagnosing metastatic lesions of regional lymph nodes simultaneously with the removal of the primary tumor, lymphadenectomy is performed.
Conservative treatment
Melanoma is considered to be one of the most resistant to chemoradiotherapy neoplasms. Nevertheless, conservative treatment is used for metastases of this tumor with a palliative purpose. In recent years, with III-IV stages of neoplasm, encouraging results have been obtained with the use of interferon preparations.
 [29], [30], [31], [32], [33], [34], [35], [36]
[29], [30], [31], [32], [33], [34], [35], [36]
Tactics in relation to formations
Any skin formation that is suspicious of melanoma, and also nevi, if any of the above listed signs of malignancy is present, must be removed with a scalpel within the healthy tissues to the fascia, followed by a histological examination. Cryolaser surgery methods are applicable to unaltered nevuses - for cosmetic purposes or for their localization in areas of potential trauma and / or increased insolation in open areas of the skin.
Forecast
The prognosis for melanoma progressively worsens, depending on the degree of invasion and the stage of the tumor. The depth of invasion affects 10-year survival as follows: I degree - survival rate is close to 100%, II degree - 93%, III degree - 90%. IV degree - 67%, V degree - 26%. Dependence of the 10-year survival rate from the stage of the process looks like this: at stage I, up to 90% of patients survive, at II - up to 70%, at III, according to different estimates - from 20 to 40%, at stage IV the prognosis is fatal. By localization, groups of favorable prognosis (head and neck), unfavorable (trunk) and indefinite (limb) are distinguished. It can be considered that more distal localizations are associated with a better prognosis than proximal and central ones. Melanoma on the skin area, usually closed by clothing, indicates a less favorable prognosis.

