Liver metastases
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The liver is the most common localization of hematogenous metastases of tumors, regardless of whether the primary tumor is drained by the portal vein or other veins of the pulmonary circulation.
Liver metastases are characteristic of many types of cancer, especially those originating from the gastrointestinal tract, breast, lung and pancreas. Initial symptoms are usually non-specific (for example, loss of body weight, discomfort in the right upper quadrant of the abdomen), but sometimes manifest as symptoms of primary cancer. Liver metastases can be assumed in patients with weight loss, hepatomegaly and in the presence of primary tumors with an increased risk of liver metastasis. Diagnosis is usually confirmed by instrumental methods of research, most often ultrasound or spiral CT with contrast. Treatment usually involves palliative chemotherapy.
Epidemiology
Metastasis to the liver is detected in about one third of patients with cancer, and in case of cancer of the stomach, breast, lung and colon, they are observed in half of the patients. The next in terms of the frequency of metastasis to the liver are cancers of the esophagus, pancreas, and melanoma. Metastases to liver cancer of the prostate and ovary are extremely rare.
Metastatic liver cancer is more common than primary cancer, and is sometimes the first clinical manifestation of a malignant tumor in the gastrointestinal tract, mammary gland, lung or pancreas.
Pathogenesis
Liver invasion by germinating into it malignant tumors of neighboring organs, retrograde metastasis through the lymphatic ducts and spreading along the blood vessels is relatively rare.
Portal emboli enter the liver from malignant tumors of the portal vein organs. Sometimes, primary tumors of the uterus and ovaries, kidneys, prostate gland or bladder can affect adjacent tissues, the blood from which flows into the portal vein system, which can lead to embolic metastases to the liver; however, liver metastases from these organs are extremely rare.
Metastatic dissemination through the hepatic artery, which seems to occur frequently, is difficult to establish histologically, since the picture is the same as in intrahepatic metastasis.
 [20], [21], [22], [23], [24], [25], [26], [27], [28], [29]
[20], [21], [22], [23], [24], [25], [26], [27], [28], [29]
Macroscopic picture
The degree of liver damage may be different. It is possible to detect only microscopically 1-2 nodes or a significantly enlarged liver “stuffed” with metastases. Often the mass of the liver reaches 5000 g. A case is described when the mass of the liver affected by metastases was 21,500 g. Metastases usually have a white color and clear boundaries. The consistency of the tumor depends on the ratio of the volume of tumor cells and the fibrous stroma. Sometimes there is a softening of the central part of the tumor, its necrosis and hemorrhagic soaking. Central necrosis of metastatic nodes - a consequence of insufficient blood supply; it leads to the appearance of impingement on the surface of the liver. Perihepatitis often develops above the peripheral metastatic nodes. Nodes are sometimes surrounded by a zone of venous hyperemia. Often there is an invasion of the portal vein. Arteries are rarely affected by tumor clots, although they may be surrounded by malignant tissue.
Tumor cells quickly metastasize with the involvement of large areas of the liver along the perivascular lymphatic ducts and along the branches of the portal vein.
The results of angiography suggest that, unlike hepatocellular carcinoma, the arterial blood supply to liver metastases is poorly expressed. This is especially characteristic of metastasis of primary tumors of the gastrointestinal tract.
Histological examination
Liver metastases can have the same histological structure as the primary tumor. However, this is not the rule; often the primary lesion is a highly differentiated tumor, while its liver metastases can be so poorly differentiated that it is impossible to establish their origin by means of histological examination.
Symptoms of the liver metastases
Early liver metastases may be asymptomatic. Initially, non-specific signs most often appear (for example, loss of body weight, anorexia, fever). The liver can be enlarged, dense and painful; severe hepatomegaly with easily palpable nodes demonstrates a progressive lesion. Rare, but characteristic symptoms are friction of the peritoneum over the liver and pleurisy-like pain in the chest. pain in the right side. Splenomegaly sometimes develops, especially in case of pancreatic cancer. Dissection of a tumor with peritoneal lesions can cause ascites, but jaundice is usually absent or only slightly expressed if the tumor does not cause biliary obstruction. In the terminal stage, progressive jaundice and hepatic encephalopathy are precursors of death.
The clinical picture may consist of the symptoms of liver metastases and the symptoms of a primary tumor.
Patients complain of indisposition, fatigue and weight loss. The feeling of fullness and heaviness in the upper abdomen is due to an increase in the size of the liver. Sometimes acute or paroxysmal abdominal pain is possible, which simulates biliary colic. Fever and sweating are possible.
In cases of significant weight loss, patients look exhausted, an increase in the abdomen is noted. The liver may have normal size, but sometimes it grows so much that its contours are seen in the upper abdomen. Metastatic nodules have a dense texture, sometimes with umbilical stresses on the surface. Above them can hear the noise of friction. Due to poor blood supply, arterial noise is absent. Often there is splenomegaly, even with normal patency of the portal vein. Jaundice is mild or absent. Intense jaundice indicates an invasion into the large bile ducts.
Edema of the lower extremities and varicose veins of the anterior abdominal wall indicate compression of the inferior vena cava affected by the liver.
Supraclavicular lymph nodes may be affected on the right.
A pleural effusion, along with some other local symptoms, may indicate lung metastases or the presence of a primary lung in the lung.
The development of ascites reflects the involvement in the process of peritoneum, and in some cases - portal vein thrombosis. Bleeding may develop as a result of portal vein thrombosis and portal hypertension. A rare complication of liver metastases of breast, colon or small cell lung cancer is the development of obstructive jaundice.
Metastases are the most common cause of true liver enlargement.
Hypoglycemia is a rare symptom of liver metastases. The primary tumor is usually sarcoma. In rare cases, massive tumor infiltration and infarction of the liver parenchyma can lead to fulminant liver failure.
If malignant carcinoid tumors of the small intestine and bronchi are accompanied by vasomotor disorders and bronchus stenosis, then multiple metastases are always detected in the liver.
Discoloration of feces occurs only with complete obstruction of the bile duct. With the localization of the primary tumor in the digestive tract fecal occult blood test can be positive.
Where does it hurt?
What's bothering you?
Diagnostics of the liver metastases
If liver metastases are suspected, functional liver tests are usually performed, but most often they are not specific for this pathology. An early increase in alkaline phosphatase, gamma-glutamyl transpeptidase, and sometimes - to a greater extent than other enzymes - LDP, levels of aminotransferases vary. Instrumental studies are quite sensitive and specific. Ultrasound is usually informative, but spiral CT scan with contrast is more likely to provide more accurate results. MRI is relatively accurate.
A liver biopsy provides a definitive diagnosis and is performed in case of insufficient information content of other studies or, if necessary, histological verification (for example, the type of liver metastasis cells) for the choice of treatment method. It is preferable to perform a biopsy under ultrasound or CT control.
 [47]
[47]
Biochemical indicators
Even with a large liver, its function may be preserved. Compression of relatively small intrahepatic bile ducts may not be accompanied by jaundice. The outflow of bile at the same time can be through the unobstructed ducts. An increase in serum bilirubin level above 2 mg% (34 µmol / l) indicates a violation of the patency of the large bile ducts in the region of the gate of the liver.
Biochemical criteria for liver metastases include increased activity of alkaline phosphatase or LDH. Perhaps an increase in the activity of serum transaminases. If the concentration of bilirubin in the serum, as well as the activity of alkaline phosphatase, LDH and transaminases is within the normal range, the probability of the absence of metastases is 98%.
Serum albumin concentration is normal or slightly reduced. The level of serum globulins can increase, sometimes significantly. Electrophoresis may reveal an increase in alpha 2- or y-globulin.
Some patients in the serum detect carcinoembryonic antigen.
Protein content is increased in ascitic fluid, sometimes carcinoembryonic antigen is present; LDH activity is 3 times higher than that in serum.
 [48], [49], [50], [51], [52], [53], [54]
[48], [49], [50], [51], [52], [53], [54]
Hematologic changes
Neutrophilic leukocytosis is quite common, sometimes the number of leukocytes increases to 40-50 • 10 9 / l. Light anemia is possible.
Liver biopsy
The diagnostic significance of liver biopsy increases when it is performed under visual control with ultrasound, CT, or peritoneoscopy. Tumor tissue has a characteristic white color and loose texture. If it is not possible to obtain a column of tumor tissue, any blood clot or detritus should be examined for the presence of tumor cells. Even if tumor cells could not be aspirated, the identification of proliferating and abnormal bile ducts and neutrophils in the edematous portal tracts, as well as focal dilatation of sinusoids indicates the presence of metastases in adjacent areas.
Histological examination of drugs does not always allow to establish the localization of the primary tumor, especially in severe anaplasia of metastases. Cytological examination of aspirated fluid and fingerprints of preparations obtained by biopsy can somewhat increase the diagnostic value of the method.
Histochemical staining is particularly important for cytological examination and the small size of the obtained tissue sample. Monoclonal antibodies, in particular HEPPARI, which react with hepatocytes, but not with the epithelium of the bile ducts and non-parenchymal cells of the liver, allow us to distinguish primary liver cancer from metastatic.
The probability of detecting metastases during liver biopsy is higher with a significant tumor mass, large liver size and the presence of palpable nodes.
X-ray examination
Survey radiography of the abdomen reveals an increase in the size of the liver. The diaphragm can be raised and have uneven contours. Calcification of primary cancer or hemangioma and metastases of colon cancer, mammary, thyroid and bronchus are rarely observed.
A chest x-ray can reveal concomitant metastases to the lungs.
X-ray contrast study of the upper gastrointestinal tract with barium allows visualization of the varicose veins of the esophagus, displacement of the stomach to the left, and rigidity of the lesser curvature. Irrigoscopy reveals the descent of the hepatic angle and transverse colon.
Scanning
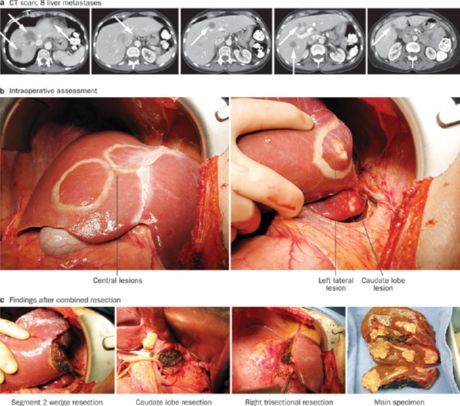
Scanning usually reveals lesions with a diameter of more than 2 cm. It is important to establish the size of the tumor nodules, their number and localization, which is necessary to assess the possibility of liver resection and to monitor the patient.
Ultrasound is a simple, effective diagnostic method that does not require large expenditures. Ultrasound metastases look like echogenic foci. Intraoperative ultrasound is especially effective for the diagnosis of liver metastases.
In hypertension, metastases are foci with low absorption of radiation. Metastases from the colon usually have a large avascular center with accumulation of a contrast agent around the periphery in the form of a ring. Approximately 29% of patients who underwent colon resection for cancer have latent metastases to the liver in CT. Delayed accumulation of the contrast agent increases the frequency of detection of metastases. CT is also used with contrast iodolipol.
MRI in T1 mode is the best method for detecting metastasis of colon cancer to the liver. T2-weighted images reveal edema adjacent to the foci of metastasis of liver tissue.
MRI with the introduction of iron oxide or gadolinium has a greater sensitivity. Duplex color Doppler ultrasound reveals a less pronounced stagnation in the portal vein than in liver cirrhosis and portal hypertension.
 [62], [63], [64], [65], [66], [67], [68],
[62], [63], [64], [65], [66], [67], [68],
Diagnostic difficulties
In a patient with a diagnosed primary tumor and suspected metastasis to the liver, it is usually not possible to confirm the presence of metastases based on clinical data. Possible metastatic liver damage is indicated by an increase in serum bilirubin level, serum transaminase activity and alkaline phosphatase. To confirm the diagnosis, aspiration liver biopsy, scanning and peritoneoscopy are performed.
Another diagnostic problem, which, as a rule, is of purely scientific interest, is the unknown localization of the primary tumor in the diagnosed metastatic liver damage. Primary tumor may be breast cancer, thyroid cancer and lung cancer. Positive results of the fecal occult blood test indicate the localization of the tumor in the gastrointestinal tract. Instructions in the history of remote skin tumors and the presence of nevi suggest melanoma. Suspected pancreatic body cancer dictates the need for endoscopic retrograde cholangiopancreatography. Usually, the results of puncture biopsy of the liver can determine the localization of the primary tumor. However, sometimes a biopsy can only reveal squamous, skirrozny, cylindrical or anaplastic cells, but the localization of the primary focus remains unknown.
What do need to examine?
What tests are needed?
Who to contact?
Treatment of the liver metastases
Treatment depends on the degree of metastasis. For single or multiple metastases in colorectal cancer, resection can prolong the patient's life. Depending on the characteristics of the primary tumor, general chemotherapy can reduce the tumor and prolong life, but does not lead to recovery; intra-arterial chemotherapy sometimes achieves the same results with fewer or less severe systemic adverse events. Radiation therapy of the liver sometimes relieves pain in common metastases, but does not prolong life. A common disease is fatal, so the best tactic in this case is palliative treatment of the patient and help to the family.
Treatment results remain unsatisfactory. In patients with a more favorable prognosis without treatment (for example, in patients with rectal cancer with metastases to the liver), it improves with specific treatment. Most of the published results were obtained in uncontrolled studies. Nevertheless, treatment should be carried out in all cases in order not to deprive the hopes of the sick and their relatives. Choose the treatment that is most likely to slow tumor growth with the least side effects.
Combined therapy is performed with 5-fluorouracil and mitoxantrone in combination with methotrexate and lomustine. It is accompanied by severe side effects, and there are no results from controlled studies. The best results of treatment are observed in breast cancer metastases.
Metastases are resistant to radiation therapy. In carcinoid syndrome, surgical intervention is indicated, which is associated with a high risk. At the same time, metastatic nodes are easily husked. Apparently, embolization feeding the tumor nodes of the branches of the hepatic artery is more preferable. In metastasis of other tumors, embolization of the arteries with gelatinous foam is also resorted to.
The introduction of chemotherapy in the hepatic artery
Primary and secondary tumors of the liver are supplied with blood mainly from the hepatic artery, although the portal vein also plays a small role in this. Cytostatics can be targeted to the tumor by catheterization of the hepatic artery. The catheter is usually installed in the hepatic artery, introducing it through the gastroduodenal artery. The gallbladder is removed. As a chemotherapy drug, floxuridine is usually used, 80-95% of which is absorbed during the first passage through the liver. It is administered using an implantable infuser gradually monthly for 2 weeks.
This treatment leads to regression of the tumor in 20% of patients and alleviates the condition in 50%. With cancer of the colon and rectum, life expectancy with such treatment increased to 26 months compared with 8 months in the control group. According to one study, the results of regional chemotherapy were better than the results of systemic therapy. In another study, with the introduction of chemotherapy through the hepatic artery, in 35 of 69 patients, an improvement was achieved, in 9 the state did not change and in 25 there was a progression of the tumor.
Complications included sepsis and catheter dysfunction, peptic ulcers, chemical cholecystitis and hepatitis, as well as sclerosing cholangitis.
Perfusion of drugs through the hepatic artery can be used as an additional method of treatment after liver resection.
There is a message about the combination of cryotherapy with regional perfusion of cytostatics through the hepatic artery.
Interstitial laser photocoagulation was also performed under ultrasound guidance. CT scan revealed a reduction in tumor volume by 50%.
Colon cancer metastasis removal
Metastatic tumors grow slowly, can be single, most of them are localized subcapsularly. Resection of the affected part of the liver can be performed in 5-10% of patients. Before surgery, a liver scan is performed. CT has high sensitivity during arterial porography. Intraoperative ultrasound is also necessary. Liver resection is indicated in cases where there are no more than four metastases and there are no damage to other organs and severe concomitant diseases. Every fourth patient during the operation has to increase the estimated volume of resection, and every eighth - to abandon it. Usually perform lobectomy or segmentectomy.
In a multicenter study, which included 607 patients with resected metastases, a relapse of liver metastases was observed in 43% of patients, and a relapse of metastases to the lungs - in 31%. In 36% of patients relapse was detected during the first year. Without signs of recurrence, 25% of patients experienced a 5-year period. In another study, the 10-year survival rate was quite high at 21%. If the concentration of carcinoembryonic antigen in the serum of patients did not exceed 200 ng / ml, the resection limit was not less than 1 cm from the tumor and the mass of the excised liver tissue was less than 1000 g, 5-year survival without signs of relapse exceeded 50%. An increased risk of recurrence is noted in cases where the resection fails to retreat from the tumor at a sufficient distance and when metastasis is localized in both lobes. In a study that included 150 patients, liver resection (46% of patients) allowed an increase in life expectancy to an average of 37 months, after a “non-radical” resection (12% of patients), life expectancy was 21.2 months, and in unresectable tumors (42% of patients) ) - 16.5 months
However, for the final evaluation of the effectiveness of surgical treatment of liver metastases, controlled studies are needed.
Liver transplantation
Two-year survival after liver transplantation in metastatic cancer averages only 6%.
Liver transplantation in patients with endocrine tumors of the pancreas and liver metastases proved to be more effective, provided that the primary tumor was also removed.
Forecast
The prognosis depends on the localization of the primary tumor and the degree of its malignancy. In general, patients die within a year after the detection of liver metastases. A relatively more favorable prognosis is observed for rectal and colon tumors. The average life expectancy of patients with liver metastases after resection of the colon is 12 ± 8 months.

