Bacteria in the urine of a child: reasons, how to treat
Last reviewed: 18.10.2021

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
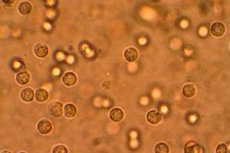
Clinical tests, including urine tests, help to monitor the child's health. There are a number of external criteria by which certain deviations are determined: volume, color, odor, transparency, etc. Biochemical indicators are more informative, because identify protein, sugar, bilirubin. The presence of bacteria in the urine of a child is established as a result of microscopic examination of its sediment and is a dangerous signal. What does it mean? It indicates a viral disease of the urinary system. [1]
The norm of bacteria in the urine of a child
A healthy child's urine contains microorganisms. The indicator of bacteria correctly collected in a sterile container of urine should not exceed 100 units per milliliter of its volume. Exceeding this threshold is called bacteriuria and indicates the development of an infectious and inflammatory process of the urinary system. [2]
Causes of the bacteria in the urine of a child
The most commonplace of reasons for the increased number of bacteria in a child's urine is the lack of hygiene when collecting it. Re-analysis will either dispel suspicions, or become a reason to look for another nature of the deviations, among which may be:
- cystitis;
- urethritis;
- pyelonephritis;
- urolithiasis disease;
- inflammation of the external genital organs.
Risk factors
Factors provoking pathology include a decrease in immunity due to hypothermia, the ingress of bacteria from the anus with improper actions after a bowel movement, ignoring hygiene procedures, bathing in dirty water. Sometimes medical procedures performed without proper antiseptic measures, and even constipation due to improper diet, lead to the development of infection. [5]
Pathogenesis
The infection can develop along the ascending path from the genitals or the large intestine through the urinary tract upward. Another way is downward, from top to bottom, for example, with inflammation of the kidneys.
Symptoms of the bacteria in the urine of a child
As a rule, bacteriuria proceeds with severe symptoms, but in some cases they may be absent. It manifests itself by frequent and painful urination , sometimes urinary incontinence , pain in the lower abdomen. The spread of infection to the kidneys leads to fever, nausea, vomiting, and pain in the lower back. [6]
Changes in the urine are visually noticeable: it becomes cloudy, flakes float in it, blotches of blood may be present, an unpleasant odor appears.
The presence of leukocytes, mucus, protein, nitrites in the urine are sure signs of an infection of the urinary system.
Complications and consequences
The identification of bacteria in urine requires an immediate response, otherwise serious and dangerous consequences for health are possible. Without treatment, inflammation of the lower urinary tract can spread to the kidneys, and pyelonephritis is fraught with further complications, as a result of which you can even lose an organ.
Diagnostics of the bacteria in the urine of a child
The very first test to diagnose a urinary tract infection (UTI) is a urinalysis . It will reveal the presence of protein, an increase in leukocytes, erythrocytes. Bacteria can be detected by examination under a microscope of sowing on a nutrient medium. Its results are received only after 6-7 days, but they will indicate the causative agent of the infection, determine its sensitivity to an antibiotic, which is necessary for the selection of drug treatment. [7]
There is also a rapid nitrite test, but it is not very informative, since not all bacteria convert the nitrates contained in them into nitrites. It will not do without an ultrasound of the kidneys : their inflammation will show the expansion of the pelvis.
Differential diagnosis
The task of differential diagnosis is to determine which organ is covered by the inflammatory process and to make one of the above diagnoses or others.
Who to contact?
Treatment of the bacteria in the urine of a child
The identification of bacteria in the urine of a child and the diagnosis requires an integrated approach in the treatment of infection, which implies not only drug therapy aimed at eliminating pain, normalizing urinary disorders, eliminating the inflammatory process, but also organizing a healthy diet, drinking plenty of fluids, and using physiotherapeutic methods. [8]
Antibiotic therapy for pyelonephritis is longer than cystitis or urethritis, and is 10-14 days against a week of treatment. [9]
Drug treatment
The choice of antibiotic depends on the type of bacterial flora, but since it will be revealed only a few days after the delivery of urine culture, first, broad-spectrum drugs are prescribed, excreted mainly through the kidneys and maximally concentrated in the bladder, and then, if necessary, the appointment is adjusted. [10]
Of the entire list of antibacterial drugs, amoxicillin, ciprofloxacin, cefaclor, ceftibuten, monural are most often prescribed. [11]
Amoxicillin - granules in a bottle for preparing a suspension are poured with purified water to the mark on it and shaken until they are completely dissolved. Children under 2 years old are given half a measuring spoon (125 ml), from 2 to 5 years old - in full, 5-10 years old - 1-2 spoons, older - 2 tablespoons three times a day.
For newborns and very young children, the dose is calculated: 30 mg of the substance per kilogram of body weight and is divided into 2 doses, the interval between which is 12 hours.
Possible side reactions in the form of rashes on the body, nausea, upset stools, headache, tinnitus. Amoxicillin is contraindicated in case of hypersensitivity to its components, with mononucleosis, lymphocytic leukemia.
Monural is a powder packaged in sachets. Before use, it dissolves in half a glass of water. Recommended for the treatment of girls over 12 years old. Drink once a day on an empty stomach before bedtime after emptying the bladder. A side effect most often occurs from the gastrointestinal tract in the form of diarrhea, rarely dizziness. It is not prescribed for allergy to the drug.
Pain syndrome is relieved by antispasmodics: no-spa, papaverine, belladonna, baralgin.
Baralgin - prescribed for children from 13 years old on a tablet 2-3 times a day, after 15 years, the dose can be increased to 2 pieces once, the frequency is the same. The drug can cause dry mouth, exacerbation of gastritis and peptic ulcer disease, tachycardia, visual impairment. An obstacle to the use of baralgin is blood diseases, severe pathologies of the kidneys and liver, bronchial asthma.
Herbal preparations are also used to reduce inflammation. One of the most popular is urolesan.
Urolesan is a combined herbal preparation in the form of capsules, drops and syrup. For children, the most suitable form is syrup. It is taken before meals, a dose in the age range of 2-7 years 2-4 ml, 7-14 years old 4-5 ml three times a day. The drug is not used for allergies to the plants from which it is made (mint, fir, wild carrots, hops, oregano), gastritis with increased stomach acidity, peptic ulcer disease, with caution in diabetes mellitus. [12]
Vitamins
In the fight against pathogenic bacteria, vitamins A will help (the daily dose should be at least 50 thousand IU), C (1-1.5 g), but the main emphasis is on natural flavonoids - vegetables and fruits with bright colors (orange, purple, red)...
Physiotherapy treatment
Hydrotherapy is widely used as a physiotherapeutic treatment, including the unique mineral water "Naftusya". Mineral baths, applications of ozokerite, paraffin are also used. Electrophoresis and electrotherapy are effective.
Alternative treatment
Many alternative therapy recipes focus on drinking plenty of fluids to flush bacteria out of the urinary tract.
Here are some:
- squeeze juice from the pulp of a watermelon, drink half a glass every 3 hours;
- mix 100ml of carrot juice with a tablespoon of celery leaf juice, drink 3 times a day;
- squeeze juice from 500g of fresh strawberries, drink half a glass 4 times a day.
Treatment of UTIs with herbs that have antimicrobial, anti-inflammatory, tanning, regenerating properties is very effective. These include bearberry, shepherd's bag, half-half, wild rosemary, chamomile, birch buds, lingonberry, juniper. Not only infusions, decoctions are prepared from them, but they are used for taking warm sitz baths.
Homeopathy
Homeopathic remedies have worked well in the treatment of urinary tract infections. They not only help in the fight against inflammation, but also increase the body's defenses, activate the processes of self-regulation of its functions. Among them are Berberis (barberry), Borax (borax), Cannabis sativa (planting hemp), Cantharis (Spanish fly), Equisetum (horsetail), Petroselinum (parsley), etc.
The appointment can only be made by a homeopath, since it depends not only on the symptoms and diagnosis, but also on the sex of the child, his anatomical features, psychoemotional state. In addition, most homeopathic remedies have not been tested on children, so they are recommended only for older people.
Surgery
Only severe anomalies of the urinary tract require surgical correction; in other cases, conservative treatment is sufficient.
Prevention
In order to prevent infection of the urinary tract, one should adhere to an abundant drinking regime, do not overcool, regularly empty the bladder, observe the hygiene of the external genital organs, and periodically resort to appropriate herbal remedies. For those who have had a UTI, it is recommended to carry out ultrasound of the kidneys and bladder for control. [13]
Forecast
In most cases, the disease has a favorable outcome. The earlier the inflammation is detected and its active treatment is started, the higher the chance of not going into a chronic course and not getting cicatricial changes in the kidneys with pyelonephritis.
Использованная литература

