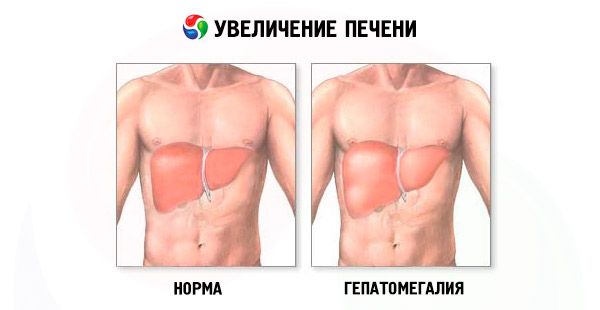
Enlarged liver
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
An enlarged liver — hepatomegaly — is noted in cases where the size of this vital organ exceeds the natural, anatomically determined parameters. As doctors emphasize, this pathology cannot be considered a single liver disease, since it is a symptom characteristic of many diseases, including those affecting other human organs and systems.
The danger of an increase in the liver lies in the complications of liver failure and other pathological conditions, which interfere with the normal functioning of this organ and create many serious health problems.
Therefore, about such a common pathology, as an increase in the liver, it is worth talking more thoroughly.
Causes of liver enlargement
Perhaps the list below, including the causes of an enlarged liver, is incomplete, but it should make it aware of the true extent of its pathogenesis and get an answer to the question - is an enlarged liver dangerous?
So, an increase in the liver in an adult can be due to:
- excessive drinking;
- cirrhosis of the liver;
- taking large doses of certain drugs, vitamin complexes and dietary supplements;
- infectious diseases (malaria, tularemia, etc.);
- defeat viruses hepatitis A, B, C;
- infections with enteroviruses, pathogens of intestinal infections, leptospira, Epstein-Barr virus (mononucleosis);
- toxic damage to the parenchyma by industrial or vegetable poisons;
- fatty hepatosis (fatty degeneration or liver steatosis);
- disorders of copper metabolism in the liver (hepatolenticular degeneration or Wilson's disease);
- disorders of iron metabolism in the liver (hemochromatosis);
- inflammation of the intrahepatic bile ducts (cholangitis);
- genetically determined systemic diseases (amyloidosis, hyperlipoproteinemia, glucosylceramide lipidosis, generalized glycogenosis, etc.);
- obliterating endarteritis of the veins of the liver;
- liver cancer (hepatocarcinoma, epithelioma, or metastatic cancer);
- leukemia;
- diffuse non-Hodgkin lymphoma;
- the formation of multiple cysts (polycystic).
As a rule, an increase in the liver lobe is observed, while an increase in the right lobe of the liver (which has a higher functional load in the organ) is diagnosed more often than an increase in the left lobe of the liver. However, this is also not good, since the left lobe is so close to the pancreas that, perhaps, the problem is precisely this gland.
A simultaneous increase in the liver and pancreas is possible with inflammation of the pancreas (pancreatitis). Inflammation is accompanied by intoxication, and the liver is involved in the elimination of toxins from the blood. If the course of pancreatitis takes on particularly severe forms, the liver may not cope with its task and increases in size.
Diffuse enlargement of the liver is a clearly not localized change in the size of its segments, consisting of hepatocytes (hepatic cells). For one of the above reasons, the hepatocytes begin to die, and the glandular tissue gives way to fibrous tissue. The latter continues to grow, thereby increasing (and deforming) certain parts of the organ, squeezing the hepatic veins and creating prerequisites for inflammation and edema of the parenchyma.
Symptoms of liver enlargement
Slightly pronounced pathology - an increase in the liver by 1 cm or an increase in the liver by 2 cm - a person may not feel. But the process of changing the natural size of the liver sooner or later begins to show more obvious clinical symptoms.
The most typical symptoms of an increase in the liver are: weakness and fast fatigue, which patients feel even in the absence of intense exertion; discomfort (heaviness and discomfort) in the abdominal cavity; bouts of nausea; weight loss. Further, heartburn, halitosis (persistent bad breath), itchy skin and dyspepsia can join.
An increase in the liver in hepatitis is accompanied not only by general malaise, but also by yellowing of the skin and sclera, fever, aching in all joints, and pulling pain in the right hypochondrium.
An enlarged liver in cirrhosis takes place against the background of the same complex of symptoms, which are joined by the following symptoms of the disease: abdominal pain and an increase in its size, a rapidly advancing feeling of satiety while eating, increased daytime sleepiness and insomnia at night, nose bleeding and bleeding gums, weight loss, hair loss, reduced ability to remember information. In addition to increasing the liver in cirrhosis (first both lobes, and then to the left more), the size of the spleen in half of the patients also increases, and doctors determine they have hepatosplenomegaly — an enlarged liver and spleen.
In the clinical manifestation of the body's lesion with a human immunodeficiency virus, an increase in liver in HIV is diagnosed at stage 2B - in acute HIV infection without secondary diseases. In addition to an increase in the liver and spleen, at this stage there is a feverish state, skin rash and rashes on the mucous membranes of the mouth and throat, an increase in lymph nodes, and dyspepsia.
Fatty hepatosis with liver enlargement
According to the latest WHO data, 25% of adult Europeans and up to 10% of children and adolescents suffer from fatty hepatosis (or steatosis). In Europe, "fatty liver" develops in 90% of alcohol abusers and in 94% of obese people. Regardless of the root cause of the occurrence of pathology, fatty hepatosis with an enlarged liver for eight years in 10-12% of patients progresses to cirrhosis. And with concomitant inflammation of the liver tissue - in hepatocellular carcinoma.
In addition to alcohol intoxication of the liver and obesity, the disease is associated with impaired glucose tolerance in type II diabetes mellitus and the pathology of the metabolism of cholesterol and other fats (dyslipidemia). From the point of view of pathophysiology, fatty hepatosis with an enlarged liver or without it develops due to damage to the metabolism of fatty acids, which may be caused by an imbalance between energy consumption and its expenditure. As a result, abnormal accumulation of lipids, in particular triglycerides, occurs in the liver tissues.
Under the pressure of accumulated fat and the resulting fatty infiltrates, the parenchyma cells lose their vitality, the size of the liver increases, and the normal functioning of the organ is disrupted.
In the early stages of fatty hepatosis, there may be no obvious symptoms, but over time there are complaints from patients about nausea and increased flatulence in the intestines, as well as heaviness or pain in the hypochondrium on the right.
Enlarged liver in heart failure
The functional interaction of all body systems is so close that an increase in the liver in heart failure is an indicator of a decrease in the right ventricular blood flow and a consequence of impaired blood circulation.
At the same time, blood circulation in the liver vessels slows down, venous congestion is formed (hemodynamic dysfunction), and the liver swells, increasing in size. Since heart failure is most often chronic, prolonged oxygen deficiency inevitably leads to the death of part of the liver cells. In their place, the connective tissue cells grow, forming whole areas that disrupt the liver. These zones are enlarged and compacted, and with it there is an increase in the liver (most often its left lobe).
In clinical hepatology, this is referred to as hepatocellular necrosis and is diagnosed as cardiac cirrhosis or cardiac fibrosis. And in such cases, cardiologists are diagnosed with cardiogenic ischemic hepatitis, which, in fact, is an increase in the liver in heart failure.
Enlarged liver in a child
An enlarged liver in a child has enough causes. So, it can be syphilis or tuberculosis, generalized cytomegaly or toxoplasmosis, congenital hepatitis or bile duct abnormalities.
With this pathogenesis, not only a moderate enlargement of the liver, but also a strong enlargement of the liver with significant parenchyma compaction can be established by the end of the first year of a child’s life.
Enlarged liver and spleen in infants - the so-called hepatolienal syndrome or hepatosplenomegaly - is the result of congenital elevated blood levels of immunoglobulins (hypergammaglobulinemia). This pathology, in addition to the increase in these organs, is manifested in a delay in the overall development of the child, poor appetite and very pale skin. Enlarged liver and spleen (with icteric symptoms) occurs in newborns with congenital aplastic anemia, which occurs due to the destruction of red blood cells, as well as due to extramedullary hematopoiesis - when red blood cells are formed not in the bone marrow, but directly in the liver and spleen.
Fatty hepatosis with an increase in the liver in children almost in half of the cases develops due to a significant excess of the age norms of body weight. Although this pathology may occur in some chronic diseases of the gastrointestinal tract, after long-term use of nonsteroidal anti-inflammatory drugs, antibacterial or hormonal therapy.
Where does it hurt?
What's bothering you?
Diagnosis of liver enlargement
Diagnosis of an increase in the liver begins with a physical examination of the patient and palpation of the internal organs of the abdominal cavity to the right of the midline of the abdomen - in the epigastric region.
During a medical examination, the doctor may detect a strong enlargement of the liver. What does it mean? This means that the liver protrudes from under the edge of the costal arch much more than the anatomical rate suggests (in an adult of average height this is no more than 1.5 cm), and it is felt well below the edge of the ribs. Then an increase in the liver by 3 cm, an increase in the liver by 5 cm or an increase in the liver by 6 cm is noted. But the final “verdict” is taken out only after a comprehensive examination of the patient, first of all, with the help of ultrasound.
An enlarged liver on ultrasound confirms that there are, for example, an “enlarged liver of a homogeneous hyperechoic structure shifted to the stomach, the outlines are fuzzy” or that “a diffuse hyperechogenicity of the liver and vagal pattern and liver boundaries are revealed”. By the way, in an adult, a healthy liver has the following parameters (on ultrasound): the anteroposterior size of the right lobe is up to 12.5 cm, the left lobe is up to 7 cm.
In addition to ultrasound in the diagnosis of liver enlargement use:
- blood test for viral hepatitis (serum markers of viruses);
- biochemical blood test (for amylase and liver enzymes, bilirubin, prothrombin time, etc.);
- urinalysis for bilirubin;
- laboratory studies of the functional reserves of the liver (using biochemical and immunological tests);
- X-ray;
- hepatoscintigraphy (radioisotope liver scan);
- CT scan or MRI of the abdominal cavity;
- Precision puncture biopsy (if necessary, obtain a sample of liver tissue to test for oncology).
An increase in the lymph nodes of the liver in the study of ultrasound is noted by specialists-hepatologists for all types of cirrhosis, viral hepatitis, tuberculosis of the lymph nodes, lymphogranulomatosis, sarcoidosis, Gaucher disease, drug lymphadenopathy, HIV infection, pancreatic cancer.
 [17]
[17]
What do need to examine?
Who to contact?
Liver augmentation treatment
Treatment of an increase in the liver is the treatment of a symptom, but, by and large, we need complex therapy for a specific disease, which has led to a pathological change in the organ.
Drug therapy of hypertrophied liver must be supported by proper nutrition with diet and vitamins. According to experts, in certain diseases involving an enlarged liver, it is possible to restore the damaged parenchyma and normal organ size.
For the regeneration of liver cells, their normal functioning and protection from negative effects, hepatoprotectors are used - special drugs with an enlarged liver.
Drug Gepabene - hepatoprotector of plant origin (synonyms - Carsil, Levasil, Legalon, Silegon, Silebor, Simepar, Heparsil, Hepatofalk-Planta). The active ingredients of the preparation are obtained from extracts of a smoked medicinal (protypin) and milk thistle fruit (silymarin and silibinin). They stimulate the synthesis of proteins and phospholipids in damaged liver maple, inhibit the formation of fibrous tissue and accelerate the process of restoring the parenchyma.
This drug is prescribed for toxic hepatitis, chronic inflammatory diseases of the liver, disorders of its metabolism and functions with an increase in the liver of various etiologies. It is recommended to take one capsule three times during the day (with meals). The minimum course of treatment is three months. Among the contraindications of this drug are acute forms of inflammation of the liver and bile ducts, age up to 18 years. For hemorrhoids and varicose veins, Gepabene is used with caution. During pregnancy and lactation, the drug is used only on prescription and under its control. Possible side effects include laxative and diuretic effects, as well as the appearance of skin rashes. Admission Gepabene incompatible with the use of alcohol.
The therapeutic effect of the drug Essentiale (Essentiale Forte) is based on the action of phospholipids (complex fat-containing compounds), which are similar in structure to the natural phospholipids contained in human tissue cells, ensuring their division and restoration in case of damage. Phospholipids block the growth of fibrous tissue cells, thereby reducing the risk of developing cirrhosis of the liver. Essentiale is prescribed for liver steatosis, hepatitis, liver cirrhosis and its toxic lesions. The standard dose is 1-2 capsules three times a day (during meals). Side effects (in the form of diarrhea) are rare.
The drug Essliver differs from Essentiale by the presence in its composition - along with the phospholipids - vitamins B1, B2, B5, B6 and B12. A combined hepatoprotective drug Phosphogliv (in capsules), in addition to phospholipids, contains glycyrrhizic acid, which has anti-inflammatory and antioxidant properties. It helps to reduce damage to the membranes of hepatocytes during inflammation and enlargement of the liver, as well as the normalization of metabolic processes. The method of administration and dosage of the last two drugs are similar to Essentiale.
Drugs with an increase in the liver include the drug based on the plant artichoke - Artihol (synonyms - Hofitol, Tsinarix, Artichoke extract). This drug helps to improve the condition of the liver cells and bring them back to normal functioning. Doctors recommend taking this drug 1-2 tablets three times a day (before meals). The course of treatment lasts from two weeks to a month, depending on the severity of the disease. As a side effect, heartburn, diarrhea, pain in the stomach can be observed. Contraindications to its use are obstruction of the urinary tract and bile ducts, gallstones, as well as severe forms of renal and hepatic failure.
In addition to the fact that medicinal plants are the basis of many drugs, hepatoprotectors, herbs with liver enlargement are widely used in the form of homemade infusions and decoctions. With this pathology, phytotherapists advise using dandelion, corn silk, calendula, sandy immortelle, yarrow, peppermint. The standard recipe for water infusion: 200-250 ml of boiling water takes a tablespoon of dry grass or flowers, brewed with boiling water, infused before cooling, filtered and taken 50 ml 3-4 times a day (25-30 minutes before meals).
Diet with increasing liver
Strictly observed diet with an increase in the liver - the key to successful treatment. In hypertrophied liver, it is necessary to completely abandon the use of fatty, fried, smoked and spicy foods, since such food overloads the liver and the entire digestive system.
In addition, a diet with an enlarged liver is incompatible with such foods as legumes, radishes, radishes, spinach and sorrel; sausage and sharp cheeses; margarine and spreads; white bread and pastry; vinegar, mustard and pepper; confectionery with cream, chocolate and ice cream; carbonated drinks and alcohol.
Everything else (especially vegetables and fruits) can be eaten, and at least five times a day, but little by little. After 19 hours, it is not recommended to eat with a healthy liver, and it’s absolutely impossible with an enlarged liver. But a glass of water with a spoon of natural honey can and should be.
In the daily diet should be 100 g of animal protein, about the same amount of vegetable proteins and 50 g of vegetable fats. The amount of carbohydrate food is 450-500 g, while the sugar intake should be reduced to 50-60 g per day, and salt to 10-12 g. The daily volume of liquid (excluding liquid food) should be at least 1.5 liters.
More information of the treatment
Prevention of liver enlargement
The best prevention of liver enlargement due to overweight or addiction to hot drinks, you know, what. Here, without observing the principles of a healthy lifestyle, it will not work...
Unfortunately, it is impossible to predict how the liver will behave and how much it may increase, for example, in hepatitis, mononucleosis, Wilson's disease, hemochromatosis, or cholangitis. But even in such cases, rational nutrition, the use of vitamins, physical exertion, hardening and avoiding bad habits will help the liver to cope with cleaning the blood of toxins, producing bile and enzymes, regulating protein carbohydrate and fat metabolism in the body. Also, to help the liver in case of the threat of hepatomegaly, vitamins of group B, vitamin E, zinc (to restore liver tissue) and selenium (in order to increase general immunity and reduce the risk of inflammatory liver diseases) are especially needed.
Liver Prediction
The prognosis for liver enlargement is quite alarming. Since the pronounced signs of this pathology do not appear immediately, treatment in one third of cases begins when the process reaches the “point of no return”. And the most likely consequences of an increase in the liver are the partial or complete loss of its functional capabilities.

