Crohn's disease
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Crohn's disease is a chronic transmural inflammatory disease of the gastrointestinal tract, which usually affects the distal ileum and large intestine, but can develop at any level of the gastrointestinal tract. Symptoms of the disease include diarrhea and abdominal pain. Abscesses, internal and external fistulas, intestinal obstruction can develop.
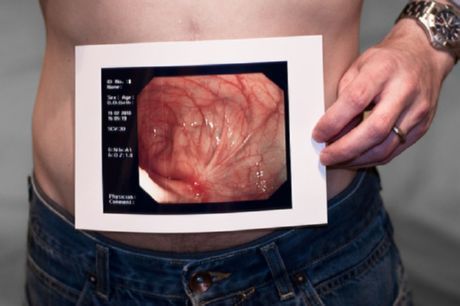
Crohn's disease - intestinal pathology
Since this disease can be localized in any part of the gastrointestinal tract, there is a certain classification for the differentiation of the forms of the disease. So, with ileocolitis, mainly the abdominal and large intestine is affected. With gastro-duodenal form - stomach and 12-duodenum. With ileitis, the abdominal colon is affected. In the case of an ejinoileitis, the small intestine is damaged. With Crohn's disease of the colon, other parts of the gastrointestinal tract are not affected.
There may be extra-intestinal symptoms, especially arthritis. Diagnosis of Crohn's disease is established by colonoscopy and X-ray contrast studies with barium. Treatment consists of the use of 5-ASA, glucocorticoids, immunomodulators, anticytokines, antibiotics and often requires surgical treatment.
 [1], [2], [3], [4], [5], [6], [7], [8]
[1], [2], [3], [4], [5], [6], [7], [8]
ICD-10 code
ICD Crohn's disease is defined as the inflammation of the gastrointestinal tract of an unknown origin, which is characterized by the defeat of individual segments, the recurring course, the appearance of ulcerative formations, which in some cases may be accompanied by complications. The disease can affect the small and large intestine together or separately. For one hundred thousand people, the frequency of the disease is about twenty-five cases. In this case, the most common is a mixed form of the disease, when the thick and small intestine are immediately affected. The risk factors for the development of the disease include genetic predisposition, chronic intestinal pathology. Macroscopic examination distinguishes between ulceration and granulomatous growths, with microscopic examination - puffiness in the damaged area and hyperplasia of the submucosal lymphafollicles. Stages of the disease development:
- The acute stage. Characterized by severe diarrhea, exhaustion, pain syndrome in the right side of the abdomen.
- Subacute stage. It is characterized by an increase in the number of ulcerative formations, the appearance of granulomas, the development of stenosis of the intestine. The pain syndrome has a cramping character.
- Chronic stage. Characterized by the further development of the disease and the occurrence of complications.
Causes of Crohn's Disease
The causes of Crohn's disease are not completely understood. There are assumptions that this disease can be transmitted by inheritance, and can also be provoked by infectious pathologies and immunological factors.
 [9], [10], [11], [12], [13], [14]
[9], [10], [11], [12], [13], [14]
How is Crohn's disease developing?
Crohn's disease begins with inflammation of the crypt and abscess formation, which progresses with the formation of small focal aphthoid ulcers. These lesions of the mucous membrane can go into deep longitudinal and transverse ulcers with anterior edema of the mucous membrane, forming characteristic changes in the gut as a "cobblestone pavement".
The spread of transmural inflammation leads to lymphedema and thickening of the intestinal wall and mesentery. Fatty tissue of the mesentery usually extends to the serous surface of the gut. The lymph nodes of the mesentery often increase. Extensive inflammation can lead to hypertrophy of the muscular layer, fibrosis and the formation of constriction, which can cause intestinal obstruction. Characteristic of the formation of abscesses and the formation of fistulas with a number of located structures, including other loops of the intestine, bladder or so. Psoas; they can even open on the front or side walls of the abdomen. Regardless of the intra-abdominal activity of the process, the formation of perianal fistulas and abscesses occurs in 1 / 4-1 / 3 cases; these complications are often the most unfavorable aspects.
Noncaseating granulomas can develop in the lymph nodes, on the peritoneum, in the liver and affect all layers of the intestinal wall. Pathognomonic sign is the detection of granulomas, but Crohn's disease in 50% of patients is not characterized by the presence of granulomas. Their presence, most likely, is not related to the clinical course.
The affected segment of the gut is clearly delineated from the normal gut ("silent zone"); hence the name - regional enteritis. Crohn's disease affects in about 35% of cases only the ileum (ileitis); in 45% - the ileum and large intestine (ileocolitis) with the primary lesion of the right flank of the colon are involved in the process; approximately 20% of cases affect only the large intestine (granulomatous colitis) and in most cases, unlike ulcerative colitis (YAC), the rectum is not always affected. Sometimes the entire small intestine is involved in the process (ejnoileitis). Very rarely the stomach, duodenum or esophagus is affected. In the absence of surgical intervention, the disease usually does not extend to the areas of the small intestine, which were not involved in the process of primary diagnosis.
There is an increased risk of developing cancer in the affected parts of the small intestine. Patients with colon lesions have a long-term risk of developing colorectal cancer, similar to ulcerative colitis, given the degree and duration of the disease.
Symptoms of Crohn's Disease
Crohn's disease is characterized by such initial symptoms: chronic diarrhea with abdominal pain, fever, anorexia and weight loss. The abdomen is painful and with palpation it is possible to determine volumetric formation or tension. Significant rectal bleeding is uncommon, with the exception of isolated colon lesions, which can occur with ulcerative colitis. Some patients develop a picture of the acute abdomen, which simulates acute appendicitis or intestinal obstruction. Approximately 1/3 of the patients experience perianal lesions (especially cracks), which are sometimes the main manifestations or even the cause of complaints. In children, extraintestinal manifestations often predominate over the symptoms of the gastrointestinal tract; arthritis, fever of unclear etiology, anemia or growth retardation may be the main manifestations of the disease, and abdominal pain or diarrhea may be absent.
If Crohn's disease recurs, then her symptoms change. Pain is the main symptom and occurs with an ordinary relapse. In patients with severe exacerbation or abscessing, palpation tenderness, protective tension, peritoneal symptoms and signs of general intoxication are noted. Sites of intestinal stenosis can cause intestinal obstruction with characteristic colic pain, bloating, stool retention and vomiting. Adhesive process after previous surgical interventions also can cause intestinal obstruction, which begins acutely, without raising the body temperature, pain and malaise, characteristic of obstruction in exacerbation. Formation of the vesicovirus fistula can cause the appearance of air bubbles in the urine (pneumouuria). Free perforation in the abdominal cavity is uncharacteristic.
Crohn's disease with a chronic course causes a variety of common symptoms, including fever, weight loss, weight loss and extraintestinal manifestations.
Crohn's disease according to the Vienna classification is divided into three main forms: (1) primarily inflammatory, which after several years of the disease usually passes either to (2) stenotic or obstructive, or (3) to the primary penetrating or fistulous. These different clinical forms define different approaches to treatment. Some genetic studies suggest a molecular rationale for this classification.
Crohn's disease and pregnancy
Crohn's disease and pregnancy are treated differently by different specialists in different ways. Some of them argue that Crohn's disease does not have a significant effect on the course of pregnancy, the birth process and the fetus, except for cases of exacerbation of the disease in this period. But most experts believe that pregnancy can have a negative impact on the development of the disease, as the enlarged uterus exerts pressure on the intestines, and also increases the level of endogenous cortisol, which after delivery rapidly falls. The prognosis of the disease also depends on whether pregnancy occurred during remission or exacerbation. If the disease runs without complications, it usually does not affect the course of pregnancy. In severe cases, Crohn's disease can trigger the risk of miscarriage, and can also pose a threat to the life of the fetus during delivery. Complications in the generic process occur most often if the disease has arisen or worsened during pregnancy. Exacerbation of the disease during pregnancy is not easy to detect, as the clinical picture is practically unchanged. In cases of intestinal obstruction, intestinal stenosis, fistula formation, a negative effect on the course of pregnancy occurs even during the remission of the disease. With a persistent weakening of the symptoms of the disease, pregnancy in the presence of Crohn's disease is permissible, while its aggravation is a contraindication for conception.
Where does it hurt?
Crohn's disease and ulcerative colitis
Crohn's disease and ulcerative colitis presumably have a relationship with hereditary predisposition, as well as the impact on the intestinal tract of infectious agents. The main difference in these diseases is that in ulcerative colitis, only the large intestine is usually vulnerable, while in Crohn's disease various parts of the gastrointestinal tract are affected. The lesion focus in ulcerative colitis, as a rule, is concentrated in any one segment of the large intestine. With Crohn's disease, the affected area can cover multiple areas of the intestinal tract. Symptoms of Crohn's disease and ulcerative colitis are very similar, and they can not always be distinguished with precision. To differentiate these two diseases, a biopsy is usually administered. Common signs of these pathologies are diarrhea and the body's temperature reaction, pain in the abdomen, deterioration or total lack of appetite, weight loss, general weakness. Nausea and vomiting, soreness in the joints may also be present. It should be noted that similar symptoms can also be observed in other pathologies of the digestive tract, so qualified diagnosis is extremely important for establishing the correct diagnosis.
What is the danger of Crohn's disease?
In order not to delay treatment and promptly seek help from a specialist, the patient needs to know what is dangerous for Crohn's disease:
- With a progressive course of the disease, the number of segments of intestinal lesions increases.
- Re-development of the disease due to surgical intervention (damage to the proximal part of the intestine).
- Formation of fistulas in the rectum and other parts of the digestive tract.
- Development of extraintestinal pathologies (erythema, pyoderma, episcleritis, uveitis, ankylosing spondylitis).
- Intestinal obstruction.
- Risk of adenocarcinoma formation.
- Perforation of the large intestine, development of intestinal bleeding.
- Enlargement of the colon.
- Inadequate absorption of nutrients in the small intestine.
Diagnosis of Crohn's disease
Crohn's disease should be suspected in patients with symptoms of inflammation or obstruction, in patients without visible gastrointestinal symptoms, but with perianal abscesses, and with unexplained symptoms of arthritis, nodal erythema, fever, anemia, or (in a child) slow growth. Family history also increases the suspicion of Crohn's disease. Similar symptoms of Crohn's disease and signs (eg, abdominal pain, diarrhea) may be a consequence of other gastrointestinal diseases. Crohn's disease differentiates with ulcerative colitis; Diagnosis can be difficult in 20% of cases in which Crohn's disease is limited only to the large intestine. However, in view of the fact that the treatment of these diseases is similar, this difference is important only when considering indications for surgical treatment or empirical therapy.
Patients with symptoms of an acute abdomen (for the first time or with relapse) need direct and lateral radiography of the abdominal cavity and CT of the abdominal cavity. These studies can identify obstruction or other possible causes of an acute abdomen (eg, appendicitis). Ultrasound can better assess gynecological pathology in women with pain in the lower abdomen and in the pelvic region.
If the initial manifestations of the disease are not so acute, it is preferable to examine the upper sections of the gastrointestinal tract and small intestine with targeted radiography of the terminal ileum than CT. Studies of the gastrointestinal tract can establish a diagnosis if they reveal a sharp narrowing (producing a "string feature") or separation of the intestinal loops. If the data obtained is doubtful, surface enterohoz and linear ulcers can be detected with enteroclysm or enteroscopy with a video cassette. You can use irrigoscopy in case of predominance of symptoms from the side of the large intestine (eg, diarrhea), in which it is possible to detect barium reflux into the terminal ileum in case of insufficient shutter, tuberosity, stiffness, thickening of the walls and narrowing of the lumen. Similar radiographic data are observed in cancer of the cecum, ileum carcinoid, lymphosarcoma, systemic vasculitis, radiation enteritis, tuberculosis of the ileocecal region and amoeba granuloma.
In unusual cases (eg, the prevalence of diarrhea with minimal pain syndrome), Crohn's disease is diagnosed similarly in case of suspected ulcerative colitis, with colonoscopy (including biopsy, studies of pathogenic intestinal microflora and, if possible, visualization of terminal ileum). Endoscopy of the upper gastrointestinal tract can reveal a lesion of the stomach and duodenum even in the absence of symptoms from the upper part of the gastrointestinal tract.
It is necessary to perform laboratory tests for the diagnosis of anemia, hypoalbuminemia and electrolyte imbalance. Functional liver tests should be performed; an increase in the levels of alkaline phosphatase and y-glutamyltranspeptidase suggests a possible development of primary sclerosing cholangitis. Leukocytosis or an increase in the levels of acute phase reactants (eg, ESR, SRV) are nonspecific, but their periodic monitoring can be used to control the activity of the disease.
Perinuclear antineutrophil cytoplasmic antibodies are present in 60-70 % of patients with ulcerative colitis and only 5-20% of patients with the disease. Crohn's disease is characterized by the presence of antibodies aHiw-Saccharomyces cerevisiae. However, these tests unreliably differentiate these two diseases. They have some value in cases of "indeterminate colitis" and are not recommended for routine diagnosis.
Algorithm for diagnosing Crohn's disease
Diagnosis of Crohn's disease is performed by X-ray and endoscopy, which allows to assess the state of the gastrointestinal tract. When analyzing feces, the presence of leukocytes is determined in it. The presence of leukocytes in the feces indicates an inflammatory process of the walls of the intestine. If the disease appears liquid stool, it is examined for the presence of infectious agents, eggs, helminths and clostridia. When performing the diagnosis of Crohn's disease using the method of irrigoscopy - X-ray of the large intestine with the introduction of a contrast agent (aqueous solution of barium sulfate with tannin). Two to three days before the start of the examination, a patient is recommended a special diet, for a day - ingestion of castor oil (about thirty grams). In the evening, put an enema and do not eat until the end of the procedure. An x-ray examination of the passage of barium is performed in order to assess the evacuation capacity of the colon and its interaction with other organs. The method of intubation enterography allows to study the small intestine by introducing into it barium nasogastric tube. After X-rays, scintigraphy can be performed to differentiate inflammatory and non-inflammatory processes. This method allows you to investigate the activity of the gastrointestinal tract and is based on the fact that the patient takes food labeled with a radioactive isotope, after which the process of its movement along the digestive tract is monitored with the help of special equipment. As part of a comprehensive diagnosis, blood, feces, and immunograms are also performed.
 [27], [28], [29], [30], [31], [32]
[27], [28], [29], [30], [31], [32]
Analyzes for Crohn's disease
Analysis of blood in Crohn's disease shows an increase in the rate of erythrocyte sedimentation, a disturbance of the water-salt balance, a low level of protein in the blood plasma, a deficiency of folic acid, vitamins B12 and D. At a coprologic examination, an increased content of fatty acids and salts is detected, undigested starch, an increased content of nitrogen in the feces. Fibrogastroscopy allows to detect lesions in the upper sections of the gastrointestinal tract. When performing a sigmoidoscopy, pathological changes in the rectum are detected. With endoscopy at the initial stage of the disease, aphthous erosive formations are visible, on the intestinal walls mucus containing pus is present.
X-ray
When diagnosing Crohn's disease, X-ray is important enough, because it can be used to precisely locate the location of the inflammatory process. Of particular importance is the radiography when examining the small intestine, since it is the only way to study it. Before starting the procedure, the patient uses inside the barium-containing fluid, which can also be injected through the rectum (barium enema). On the radiograph the liquid is recognized by white color, which allows to see ulcer formations, narrowing of the intestine, etc. If such an investigation proved ineffective, other types of X-rays are additionally assigned.
Colonoscopy
For the diagnosis of Crohn's disease, colonoscopy is of great importance. Colonoscopy in Crohn's disease allows you to get the most complete picture of the condition of the large intestine. It helps to identify the presence of ulcerative formations, foci of inflammation and bleeding. The sounding of the large intestine allows you to examine it completely - from the cecum to the rectum. Usually the procedure is performed without prior anesthesia. Local anesthesia is done in those cases when a pronounced pain syndrome is localized in the anus, as well as in severe processes that disrupt the functioning of the small intestine, the formation of adhesions in the abdominal cavity. The procedure is carried out in the lying position with the introduction through the anus in the rectum of a special device (a colonoscope). Two days before the colonoscopic examination, the patient was shown a slag-free diet, the day before, and on the day of the procedure the food should consist only of liquid (broths, teas). The reception of castor oil the day before the study is also shown. Two tablespoons of butter dissolve in about half a glass of kefir and take it inside, which helps to completely clean the large intestine. In the morning before the procedure, put one or two enemas - until the bowels are completely cleared and water is extracted from it.
What do need to examine?
Who to contact?
How to treat Crohn's disease?
An unequivocal answer to the question of how to treat Crohn's disease does not exist at the moment, as the causes that cause the disease are not precisely established. Therefore, the main treatment for the development of this pathology is aimed at reducing inflammatory processes, stabilizing the patient's condition and preventing the occurrence of complications. The doctor-gastroenterologist and proctologist are engaged in treatment of this disease. If there is an immediate threat to the life of the patient, surgery is prescribed, for example, with the development of an abscess, as well as ineffectiveness of conservative methods of treatment. Conservative therapy in Crohn's disease involves, first of all, the appointment of a diet, for example, table number 4 B. It helps to reduce irritation of the digestive tract and fermentation processes, reduce gastric secretion and the separation of bile. Various variations of dietary nutrition are aimed at minimizing the pain syndrome and correcting the work of the digestive system. Medicamentous treatment is aimed at the removal of inflammation and symptoms of the disease, strengthening the body's defenses. The drug sulfasalazine is taken before meals four times a day for one to two grams in the acute phase of the disease. In the period of relief, the dosage is gradually reduced to five hundred milligrams. The drug mesalazine is taken orally 400-800 mg three times a day for two to three months. In the process of treatment, short-term use of corticosteroids, immunosuppressants, immunosuppressive agents that block cytokines, which cause erosive and ulcerative formations on the walls of the intestine, is also possible. As an antibacterial therapy with the appearance of purulent formations using drugs metronidazole, ciprofloxacin. Depending on the symptoms of the disease, the patient may be prescribed funds for diarrhea or constipation, as well as anesthetic and haemostatic drugs, vitamin-mineral complexes.
Symptomatic treatment
Manifestations of seizures and diarrhea can be reduced by oral intake up to 4 times a day (preferably before eating) of loperamide at 2-4 mg. Such symptomatic therapy is safe, except in cases of severe, acute colitis, which can progress to a toxic megacolon as in ulcerative colitis. Hydrophilic mucilloids (eg methyl cellulose or psyllium preparations) sometimes prevent irritation of the rectum and anus, increasing the stool density. It is necessary to avoid rough food with stenotic form of the disease or active inflammation of the colon.
Treatment for easy flow
This category includes patients on outpatient treatment who are shown oral administration of drugs and who have no signs of intoxication, soreness, bulging in the abdomen or obstruction. 5-amino-salicylic acid (5-ASA, mesalamine) is usually used as a drug of treatment in the first stage, although its effectiveness in the disease of the small intestine is very limited. Pentase is the most effective formulation for the disease of the proximal ileum; Asakol is effective in affecting the distal ileum; all formulations are approximately equivalent in colitis, although none of the newer drugs compete with sulfasalazine in effectiveness depending on the dose.
Some clinicians consider antibiotics as the main drug; they can be used in patients with ineffectiveness of 5-ASA for 4 weeks; their application is strictly empirical. Treatment with any of these drugs can last for 8-16 weeks.
With the effectiveness of treatment, patients who have Crohn's disease need maintenance therapy.
Treatment in severe conditions
Patients without abscesses, but with pain syndrome, palpation pain, fever and vomiting, or with ineffective therapy for mild disease, show the use of glucocorticoids, orally or parenterally, depending on the severity of the manifestations of the disease and the frequency of vomiting. Prednisolone is more rapidly and efficiently administered orally than oral administration of budesonide, but the latter has fewer undesirable effects. Patients with ineffectiveness of glucocorticoids or in which their dose can not be reduced should be prescribed azathioprine, 6-mercaptopurine or, possibly, methotrexate. Infliximab by some authors is considered as a second-line drug after glucocorticoids, but its use is contraindicated in case of active infection.
If the obstruction occurs as a result of the adhesion process, nasogastric aspiration, intravenous fluid transfusion and sometimes parenteral nutrition are performed first. Uncomplicated Crohn's disease, which led to obstruction is resolved within a few days; the absence of a rapid effect indicates a complication or other etiology of obstruction and requires direct surgical treatment.
Fulminant course of the disease or abscess formation
Patients with intoxication, high fever, persistent vomiting, peritoneal symptoms, painfulness and palpable volume formation in the abdominal cavity should be hospitalized with the appointment of intravenous infusion and antibacterial therapy. Abscesses must be drained by percutaneous puncture or surgically. Intravenous administration of glucocorticoids should be administered only if infection is eliminated or suppressed. If the use of glucocorticoids is ineffective within 5-7 days, surgical treatment is indicated.
Fistulas
First of all, fistulas are treated with metronidazole and ciprofloxacin. If the treatment is ineffective for 3-4 weeks, patients should be given immunomodulators (immunosuppressants, eg, azathioprine, 6-mercaptopurine) with or without exposure to infliximab for a faster response. Cyclosporine is an alternative, but they often recur after treatment. Perianal fistula with severe course and untreatable treatment may be an indication for a temporary colostomy, but they almost always recur after the restoration of the passage; therefore, gut disconnection should be considered more in addition to radical surgical care than primary treatment.
 [40], [41], [42], [43], [44], [45], [46], [47], [48],
[40], [41], [42], [43], [44], [45], [46], [47], [48],
Supportive treatment
Patients in whom 5-ASA can achieve remission require maintenance therapy with this drug. Patients who need urgent treatment with glucocorticoids or infliximab generally require maintenance therapy with azathioprine, 6-mercaptopurine or methotrexate. Glucocorticoids are neither safe nor effective with prolonged maintenance therapy. Patients in whom infliximab was effective in the acute period of the disease, and the use of antimetabolites as maintenance therapy was ineffective, in the remission period, repeated doses of infliximab 5-10 mg / kg at an interval of 8 weeks may be prescribed. Monitoring during remission is based only on symptoms and blood tests and does not require an X-ray or colonoscopy study (except for the usual annual control of dysplasia) after 7 years of the disease.
Treatment with surgical methods
Even though approximately 70% of patients ultimately need surgical treatment, operations are always performed with caution. Indications for surgery patients who have Crohn's disease, are recurrent intestinal obstruction. Resection of the affected bowel can lead to the disappearance of symptoms, but does not cure the disease, since Crohn's disease most likely recurs even after resection of the entire apparent altered disease of the gut. The recurrence periods found during endoscopic examination of the anastomosis zone are more than 70% within 1 year and more than 85% within 3 years; clinical symptoms appear in approximately 25-30% of patients after 3 years and in 40-50% within 5 years. Ultimately, repeated surgical interventions are required in almost 50% of cases. However, the percentage of relapses decreases with early postoperative prophylaxis with 6-mercaptopurine, metronidazole or, possibly, 5-ASA. If the surgical intervention is performed according to the indications, almost all patients note an improvement in the quality of life.
Nutrition for Crohn's disease
Proper nutrition with Crohn's disease is quite important. With this disease, it is recommended to abandon dairy and cereal products, caffeine, sugar, spirits. The daily rate of water consumption for this disease should be about one and a half liters. As a therapeutic diet for Crohn's disease, diet No. 4 and its various variations are prescribed. In the acute phase of the disease, diet table No. 4 is prescribed, it should be eaten five to six times a day, then switch to diet No. 4b. To restore the functioning of the intestine before bedtime, you can take glutamine (five to ten grams of this substance should be diluted in a glass of water). Parenteral nutrition is recommended for severe exhaustion and persistent diarrhea. The approximate menu of diet table No. 4 can be as follows:
- Wheat biscuits.
- Low-fat broth.
- Rice or pearl soup on the water.
- Mashed porridge, cooked without using milk.
- Beef cutlet steamed.
- Boiled lean fish.
- Kissel.
- Strong tea.
- Kefir.
- Bilberry fruits or cherries.
- Broth of dogrose.
Dietary table No. 4b includes low-fat soups, except dairy and legumes, dry biscuits, wheat bread, beef, veal, chicken, steamed, lean boiled fish, fresh cottage cheese, kefir, boiled eggs, mashed porridges, boiled potatoes, carrot. The sample menu of this table is as follows:
- First breakfast: steamed omelet, mango, tea
- Second breakfast: baked apples
- Lunch: low-fat meat broth, boiled carrots, kissel
- Afternoon snack: rose hips infusion
- Dinner: low-fat boiled fish and mashed potatoes, tea or jelly
More information of the treatment
Prognosis for Crohn's disease
Crohn's disease is rarely cured and characterized by intermittent attacks of relapses and remissions. Some people have a severe course with frequent, debilitating periods of pain. However, with adequate conservative therapy and, if necessary, surgical treatment, most patients achieve good results and adaptation. The disease-related mortality is very low. Gastrointestinal cancer, including cancer of the colon and small intestine, is the leading cause of death associated with the disease.

