Medical expert of the article
New publications
What is aspermia?
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A disorder of the spermatogenesis system in the form of absence of sperm (seminal fluid) secretion during ejaculation (ejaculation) with normal sexual arousal is defined as aspermia (or aspermatism). The ICD-10 code of pathology is N46 (male infertility). [1]
Epidemiology
Statistically, aspermia with obstruction of the ejaculatory ducts is the cause of male infertility in 6-10% of cases.
Although not more than 2% of male infertility cases are associated with retrograde ejaculation, but it is recognized as one of the major causes of aspermia.
In addition, almost 14% of infertile men with aspermia have an associated chromosomal abnormality. Microdeletions of the Y chromosome are second among the genetic causes of lack of sperm during ejaculation, accounting for up to 10% of cases.
And the first place is occupied by Klinefelter syndrome, detected in 11% of men with aspermia (with the overall prevalence of this genetic disorder - 0.2% of the male population). [2]
Causes of the aspermia
What can cause a lack of sperm in the ejaculate or ejaculate in general (the fluid secreted during sexual intercourse containing spermatozoa and secretions of the representative gland and seminal vesicles)? Obviously, either because of problems with its formation - spermatogenesis - or with an obstacle to its release at the time of ejaculation.
Possible causes of aspermia are primarily attributed by experts to its entry into the bladder - so-called reversed or retrograde ejaculation, which is most often the result of partial or complete occlusion of both ejaculatory ducts (ductus ejaculatorius) that pass through the prostate and open into the prostate part of the urethra (prostate urethra).
Obstruction of these ducts can be acquired: by traumatic injury, bilateral orchitis (inflammation of the testicles), by inflammation of the testicular appendages (epididymis) - epididymitis, due to frequent urinary tract infections with strictures of the urethra; by damage to the urogenital structures by Mycobacterium tuberculosis and TORCH infection. And affecting the genital glands cystic fibrosis, in which there is underdevelopment of the seminal ducts is a congenital cause of this pathology.
Absence of semen and ejaculate discharge in cases may be noted:
- Testicular failure to descend into the scrotum - cryptorchidism;
- Testicular atrophy;
- Bilateral testicular tumors (from Sertoli cells or Leydig cells);
- Tubular ectasia (cystic transformation) of the testicles;
- Abnormal dilation of the testicular spermatic cord veins - varicocele;
- Del Castillo syndrome (sertoli cell syndrome);
- Idiopathic or secondary hypogonadism, resulting in a hormonal imbalance with insufficient androgen production;
- The presence of so-called sperm antigens or antisperm antibodies (AsAt).
Absence of semen during ejaculation may be due to prostate secretory dysfunction in malignancy, adenoma, hyperplasia and diffuse changes of the prostate parenchyma, as well as agenesis, hypoplasia or cysts of the seminal vesicles.
The hereditary klinefelter syndrome (with aplasia of the testicular epithelium) and microdeletions of the sex Y chromosome - loss of its microscopic region in the spermatogenesis-specific region (the aspermia/azoospermia factor region - AZF) have a significant place in the etiology of aspermia/azoospermia.
Risk factors
To date, risk factors for decreased spermatogenic function with aspermia are considered to be:
- Trauma and overheating of the testicles;
- The presence of chronic diseases and tumor formations of the genitourinary sphere;
- Congenital dysfunction of the adrenal cortex - adrenogenital syndrome;
- Hypothalamic dysfunction;
- Insufficient levels of thyroid hormones (hypothyroidism);
- Spinal cord nerve lesions in the upper lumbar region and diabetic neuropathy with damage to peripheral nerve fibers;
- Long-term use of certain medications, particularly alpha-blockers, anabolic steroids, antidepressants, antihypertensives;
- Pelvic radiation therapy;
- Complications of prostate, scrotal and testicular surgery, inguinal hernia or bladder tumor surgery, after epididymectomy and retroperitoneal lymphadenectomy.
The risk of spermatogenesis disorders is increased with obesity, diabetes, frequent stress and depression. The organs of the male reproductive system are negatively affected by nicotine, alcohol and narcotic substances; prolonged exposure to heavy metals, phenol and benzene derivatives; high doses of ionizing radiation.
Pathogenesis
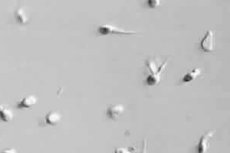
Sperm (from Greek spermatos - semen) is produced in the seminiferous tubules located in the lobules of each testis, the male sex gland. Sertoli cells located here support and nourish undeveloped progenitor cells (spermatogonia), which are successively transformed by mitosis and meiosis into spermatocytes, then into spermatids, and then mature into spermatozoa. This process is called spermatogenesis. In this process, mature spermatozoa (ready for fertilization of the female egg) due to the contractions of the tubules get to the testicular appendages (epididymis), and from there - through the seminal ducts (ductus deferens) - to the seminal vesicles (s.glandula seminalis), where they are stored for subsequent ejaculation with seminal fluid.
In addition, the interstitial Leydig cells, which are located next to the testicular tubules, produce the male sex hormones androgens (testosterone, androstenedione and dehydroepiandrosterone). This occurs only when these cells are stimulated by luteinizing and follicle-stimulating hormones (LH and FSH) released by the anterior lobe of the pituitary gland in response to gonadotropin-releasing hormone (GnRH or gonadoliberin), which in turn is released by the hypothalamus.
A disorder at any stage of spermatogenesis can trigger the mechanism of decreased or discontinued sperm production. For example, the pathogenesis of aspermia in men with Sertoli cell syndrome (Del Castillo syndrome) lies in the partial atrophy of the seminal tubules of the testicles, which may be completely absent spermatogonia - cells that after division become spermatozoa. In the presence of sperm antigens, the blood-brain barrier is breached and an autoimmune reaction to spermatozoa develops.
In retrograde ejaculation, there is insufficient tension of the bladder neck muscle, resulting in what is known as a dry orgasm, in which very little or no semen is released as it enters the bladder.
And in cases of abnormal dilation of the testicular veins of the spermatic cord, the mechanism of aspermia is explained by compression squeezing of the seminal duct passing in it, as well as local blood stasis in the scrotum and deterioration of trophic testicular tissues.
Also read:
Symptoms of the aspermia
The first signs of aspermia are the absence of sperm (seminal fluid) discharge after ejaculation. Other symptoms such as pain, swelling or lumpiness in the testicular area may be due to causative diseases (which have been listed above).
There may also be pain in the scrotum or when urinating, cloudy urine after sexual intercourse.
Aspermia is iatrogenic, psychogenic and idiopathic; there is a distinction between testicular and obstructive types of aspermia. Testicular, that is, caused by pathology of sperm formation in the testicles, is considered true aspermia, it is characterized by the absence of ejaculation and the feeling of orgasm. And false aspermia (another definition - obstructive or mechanical) - the result of a violation of sperm ejection into the prostate part of the urethra through the seminal ejection ducts. And in the obstructive type, there can be pelvic pain, especially pronounced shortly after ejaculation.
According to studies, testicular aspermia accounts for 87% of cases, while obstructive aspermia accounts for 13%.
Complications and consequences
The main consequences of aspermia are male infertility and the stress of not being able to conceive.
Diagnostics of the aspermia
Complete information with materials:
Required tests for diagnosis: semen analysis, also macroscopic semen analysis; post-ejaculatory urinalysis; blood tests for testosterone, dihydrotestosterone, LH, FSH, GnRH and thyroid hormone levels; Sertoli cell inhibin; anti-sperm antibodies; karyotype test; histology of testicular biopsy.
Instrumental diagnostics includes pelvic ultrasound, transrectal ultrasound of the prostate, ultrasound of the scrotum and testicles, scrotal thermography.
Differential diagnosis
Differential diagnosis is carried out to clarify the etiology of aspermia. In addition, it is necessary to distinguish such disorders of the reproductive system of men, which ensures their fertility, as a decrease in the number of spermatozoa in the ejaculate - oligospermia, absence of spermatozoa in the ejaculate - azoospermia, as well as pathological inability to ejaculate, i.e. absence of ejaculation (with or without orgasm) - anejaculation.
Who to contact?
Treatment of the aspermia
In almost all cases, treatment depends on the cause, and for each patient its strategy and choice of methods is based on individual factors.
Thus, infections are treated with antibiotics; treatment of chronic prostatitis; in case of low levels of gonadotropic hormones, hormone replacement (steroid) therapy is performed (with the appointment - depending on the nature of the identified hormone deficiency - Gonadotropin, Andriol, Menotropin, Pergonal, Horagon, Profazi, etc.).
Amino acid preparations (L-arginine, L-carnitine, L-carnosine), glycyrrhizic acid, zinc preparations, vitamins A and E are also used.
Retrograde ejaculation associated with iatrogenic effects of medications or surgical procedures that have caused relaxation of the bladder neck muscles, as well as with neurologic diseases and diabetes can be treated medically, in particular with drugs that stimulate the sympathetic nervous system (ephedrine derivatives, etc.).
Some patients may require surgical treatment: surgery to correct anatomical anomalies, reconstructive vascular surgery in the presence of varicocele, obstruction of the ejaculatory ducts.
For more information see. - male Infertility - Treatment
Prevention
As a prevention of aspermia and other disorders of the male reproductive system, experts give the following general recommendations: give up nicotine, limit the use and alcohol, maintain a healthy weight, avoid genital overheating, exposure to pesticides, heavy metals and other toxins, timely treat urinary tract infections and prostate diseases.
Forecast
The dependence of the prognosis of aspermia on its causes is obvious, and in many cases men remain infertile and have to resort to assisted reproductive technologies to have children.

