Medical expert of the article
New publications
Azoospermia
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When the analysis of a man's ejaculate reveals the absence of spermatozoa, it is called azoospermia. The causes of this disorder can be different: from primary and secondary gonadal insufficiency (cryptorchidism, degeneration of the epithelium of the testicular tubules, hyporchidism, etc.) to other mechanical barriers that can block the transport of sperm from the testicles to the seminal vesicles. The quality of libido may not be affected. Azoospermia is diagnosed by repeated microscopic examination of semen. [1]
Therapy is long-term, pathogenetic.
Epidemiology
Infertility in men is the inability to fertilize a woman. To date, doctors have the results of numerous studies, according to which in 40% of infertile marriages, the "culprit" of the inability to conceive is a man. Another indicator of statistics: about 15-20% of marriages have similar difficulties associated with infertility.
The modern concept of "infertile marriage" implies that spouses are unable to conceive for 12-24 months of regular sexual activity without the use of contraception.
A man's ability to impregnate a woman is determined by the properties of his seminal fluid and the number and quality of sperm present in it. The ejaculate is a mixed secretion of the testicles and appendages, as well as the glandular system represented by the seminal vesicles, prostate, Littre's and Cooper's glands. Spermatic fluid is alkaline in reaction, with pH fluctuating between 7.0 and 7.6. It is within this range that sperm are most comfortable traveling. In addition, an alkaline environment makes sperm more resistant to the acidic vaginal environment (the average pH in the vagina is 4.5 and in the cervical canal is 7.5).
According to statistics, azoospermia is diagnosed in about 2% of infertile couples.
Causes of the azoospermia
Azoospermia is accompanied by a violation of sperm formation, as a result of which the seminal fluid does not contain sperm. Depending on the underlying causes, experts distinguish obstructive and nonobstructive variant of pathology.
Azoospermia entails the loss of a man's ability to conceive naturally, and for some patients, assisted reproductive technologies are also unsuccessful.
Azoospermia can have obstructive and nonobstructive onset. In the first case, the cause is the blockage of the sperm ducts, and in the second case, the direct production of sperm is impaired. [2]
Sperm transport problems can occur due to the following reasons:
- Infectious and inflammatory processes affecting the male reproductive system and negatively affecting a man's ability to fertilize;
- Traumatic injuries, surgical interventions in the spinal column (lumbosacral region), abdominal cavity, genital organs;
- Dilation and enlargement of the scrotal venous vessels (Varicocele );
- Specific contraceptive methods like vasectomy - a procedure in which the ejaculatory ducts are cut and tied;
- Congenital absence or fusion of the spermatic ducts.
Non-obstructive type of azoospermia is not related to the blockage of sperm excretion, but has to do with the disruption of sperm production in the body. The causes that provoke such a malfunction are as follows:
- Taking certain medications - particularly antibiotics, steroid hormones, and chemotherapy;
- Alcohol abuse, smoking and drug use;
- Unfavorable heredity (e.g. klinefelter or kallman syndromes);
- Hormonal imbalance affecting testicular functionality;
- Retrograde ejaculation, in which sperm fall into the bladder instead of the urethra (occurs against the background of spinal cord injuries, diabetes mellitus, etc.);
- Exposure to radioactive radiation, radiation therapy;
- Severe or prolonged elevation of body temperature, chronic intoxication, poisoning by pesticides, heavy metals;
- Testicular failure.
Risk factors
Since disorders of spermatogenesis and azoospermia are quite common problems among men, scientists initiated a study in which they were able to identify basic risk factors for the development of male infertility:
- Bad habits (smoking, drinking alcohol);
- Improper diet (consumption of mainly fatty, salty and spicy food);
- Occupational hazards for five years or more (high and too low temperature exposure, gassy and dusty air, chemical intoxication);
- Unfavorable environmental conditions;
- Ignoring diseases, untimely seeking medical help, chronicization of pathologies;
- Hypodynamia, predominantly sedentary and sedentary lifestyle;
- Excessive psycho-emotional stress, frequent conflicts, worries, fears;
- Excessive exercise.
One of the leading factors in the development of azoospermia is considered to be unhealthy lifestyle of modern representatives of the stronger sex. Harmful habits have a rather pronounced negative impact on the health and reproductive capacity of men, and even more so in combination with other existing factors. [3]
At-risk groups can include:
- Patients who have a history of sexually transmitted infections;
- Men who have been exposed to ionizing rays or chemically active substances;
- Persons whose immediate family members have suffered from hormonal disorders;
- Men with a history of traumatic injuries to the external genital system.
Pathogenesis
Azoospermia in general is provoked by one of three basic causes:
- Impaired function of the ducts through which sperm are excreted.
- Impaired testicular functionality.
- Other diseases and conditions.
The first cause, disturbed output channels, is due to factors such as:
- Traumatic spinal cord injuries, in which there is a discharge of sperm secretion into the bladder cavity;
- Prostate surgeries (surgical treatment of prostatitis, prostate adenomas, etc.);
- Diabetes;
- Infectious-inflammatory pathologies such as tuberculosis or venereal diseases;
- Genetic pathologies accompanied by metabolic failure (e.g., cystic fibrosis);
- Congenital defective abnormalities of the vas deferens.
The second cause, impaired testicular functionality, is a consequence:
- Of undescended testicles (cryptorchidism);
- Of low male sex hormone production;
- Traumatic and other testicular lesions;
- Radiation exposure, bad habits;
- Inflammatory reactions involving the testicular area;
- STDs, orchitis;
- Genetic defects, congenital anomalies.
Among other pathologies that can provoke the development of azoospermia, experts call such diseases:
- A lesion of the hypothalamus, the brain region that controls the production of sex hormones;
- Lesion of the pituitary gland - a department "subordinate" to the hypothalamus, which can be affected as a result of prolonged intoxication (including alcohol and drugs), tumor processes and hemorrhages.
The process of spermatogenesis is the formation and maturation of spermatozoa: it begins at puberty and lasts until old age. Male sex cells are formed in the tortuous testicular seminal ducts. This occurs sequentially: from the proliferation of spermatogoniums to the processes of meiosis and spermiogenesis. The peak activity of the process is observed at a temperature regime of about 34°C. Such a regime is maintained, due to the anatomical localization of the testes not in the abdominal cavity, but in the scrotum. The spermatozoa mature completely in the testicular appendage. The entire cycle of sperm formation in the male body lasts about 74 days.
Symptoms of the azoospermia
The main sign of azoospermia is the inability of a couple to conceive a child. As a rule, it is with this problem that men seek medical help, since in general sexual function is most often not impaired. Other symptoms may appear only if they are caused by the main, primary disease. For example, insufficient testicular function - hypogonadism - is manifested by underdevelopment of the secondary sexual picture, which is manifested by underexposed hair, female body type, gynecomastia. Secretory azoospermia is often detected against the background of testicular hypoplasia, decreased sexual ability, erectile dysfunction, small penis syndrome.
Different types of obstructive azoospermia are sometimes accompanied by a feeling of discomfort, pulling pain in the genital area, swelling or swelling of the scrotum. Palpatory disorders of the testicles are often not detected, but the appendages may be enlarged - due to the accumulation of male germ cells in them. Obstruction often occurs simultaneously with retrograde ejaculation.
In the vast majority of cases, a man suffering from azoospermia does not notice any pathological signs. The first "bell" appears when the spouses start planning a pregnancy, but regular unprotected sexual contacts do not lead to the long-awaited result: the woman does not get pregnant.
Doctors distinguish a number of symptoms that should be paid attention to, as they can indicate the presence of malfunctions long before the patient suspects male infertility and azoospermia:
- Mild intermittent pain in the groin area;
- Swelling, swelling in the scrotal area;
- Weakening of erections and libido;
- A constant feeling of fatigue;
- Swelling, enlargement of the breast glands (gynecomastia);
- Chronic and frequent infectious processes;
Poor hair growth in the face and body, as well as other signs of a probable decrease in the production of male sex hormones.
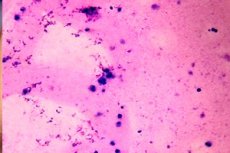
Semen in azoospermia
Semen evaluation is performed as follows:
- Normosemia - 1 to 6 ml of sperm fluid.
- Multisemia - the volume of sperm fluid exceeds 6 ml.
- Normospermia - the number of male sex cells per 1 ml of semen is 60-120 million.
- Polyspermia - the number of male sex cells per 1 ml of sperm fluid exceeds 120 million.
- Aspermia - spermatozoa and spermatogenesis cells are absent.
- Oligozoospermia - the number of male sex cells in the sperm fluid does not exceed 20 million per 1 ml.
- Hypospermia - the sperm count is between 20 and 60 million sperm per 1 ml.
- Azoospermia - spermatozoa are absent in the semen, but immature forms of spermatogenesis are present.
Forms
Azoospermia is a type of infertility in men in which spermatozoa are not detected in the ejaculate analysis. Andrologists and urologists point out the presence of several forms of abnormal spermatogenesis: it is not only azoospermia, but also oligozoospermia, asthenozoospermia, teratozoospermia.
In addition, a combination of pathologies is possible - for example, diagnoses such as oligoasthenozoospermia, asthenoteratozoospermia, oligoteratozoospermia, etc. Are often encountered.
|
Asthenozoospermia |
The presence of less than half of the spermatozoa with type I (progressive linear) and type II (slow linear or progressive non-linear) movement, or the presence of less than 25% of the cells with type I movement. The number and shape of male germ cells are within normal limits. |
|
Oligozoospermia |
A decrease in the number of living male germ cells - less than 20 million per 1 ml of seminal fluid. |
|
Teratozoospermia |
More than 50% of male germ cells are characterized by abnormalities in structure (head and tail). |
|
Azoospermia |
No sperm in the sperm secretion. |
According to the etiologic (causal) factor, specialists divide such types of violation:
- Nonobstructive azoospermia is a disorder not associated with obstruction of the seminal tract. The pathology is most often a secretory type of disorder.
- Obstructive azoospermia is associated with obstruction of the passage of the seminal ducts. This leads to the fact that male sex cells can not get from the testicles to the sexual organ. This variant of azoospermia occurs in 40% of cases. Ductal obstruction can be acquired or congenital.
- Obturator azoospermia is caused by obstruction of the spermatic ducts. This pathology may be the result of complete or partial aplasia of the appendages, ducts or seminal vesicles, acquired obstruction of the ducts as a result of post-inflammatory obstruction, cystic and tumor processes that compress the duct of the appendage. Iatrogenic obstruction due to surgical interventions in this area is also possible.
- Secretory azoospermia is accompanied by impaired sperm formation due to bilateral cryptorchidism, epidparotitis, tumor processes, radiation or toxic effects.
- Temporary azoospermia is a transient condition in which sperm are not always absent in the seminal secretion, but only periodically. For example, the disorder is noted in the exacerbation of certain diseases, after severe stress, against the background of treatment with certain drugs (hormones, antibiotics, chemotherapy drugs). Temporary malfunction often occurs if a man abuses visiting baths and saunas, or too often has sexual intercourse.
- Genetic azoospermia is caused by a hereditary factor and is a congenital pathology. The causes are numerical or structural aberrations of sex chromosomes. Carriers of CFTR gene mutation (cystic fibrosis) often have obstructive azoospermia associated with the absence or obstruction of the seminal ducts. [4]
- Congenital azoospermia, which develops in the fetus during fetal development, can be caused by hypopituitarism, Cullman or Prader-Willi syndromes, other disorders resulting in gonadotropin or GnRH deficiency, and Klinefelter syndrome. More than 10% of patients with diagnosed azoospermia have abnormal spermatogenesis due to an abnormality of the Y chromosome. Such abnormalities most often extend to the long arm of the chromosome: this section is designated by specialists as AZF (azoospermia factor).
According to the etiological factor, such forms of azoospermia are distinguished:
- The pretesticular form is associated with hormonal malfunctions and represents a secondary lack of testicular function.
- Testicular form is a primary testicular dysfunction due to an abnormality from the testicles themselves.
- The post-testicular form is due to impaired ejaculation or blockage of the ejaculatory ducts.
The first and third forms of the disease are the easiest to treat. Testicular variant is often irreversible (exception - varicocele).
Complications and consequences
Azoospermia itself is already considered a complication of infectious-inflammatory, endocrine disorders affecting the urogenital system.
However, what can turn out azoospermia, if you do not treat the pathology?
Often society has a stereotypical thinking: if there are no children in the family, the problem is in the woman. However, statistics say quite differently: women's health does not allow getting pregnant in only 1/3 of cases. Another 1/3 are violations on the part of male reproductive health. The remaining 33% are problems on the part of both partners at once, or cases when the reason for the lack of pregnancy can not be determined. So, if a woman fails to get pregnant for 1-2 years with regular unprotected sexual intercourse, both partners should be diagnosed.
In some men, azoospermia is triggered by serious medical conditions that can cause equally serious complications over time:
- Congestion;
- Inflammatory pathologies (prostatitis, orchitis, vesiculitis, epididymitis).
In addition, the immediate fact of inability to conceive often becomes the cause of depressive disorders in men, stressful situations, leads to family conflicts and misunderstandings.
Male infertility with azoospermia
If no male sex cells are detected in the seminal fluid during diagnosis, it does not mean that the male body does not produce such cells at all. It often happens that the testicles are fully functioning, but there is an obstacle on the way to the exit, blocking the sperm from entering the seminal fluid.
There is a certain threshold number of sperm that must be produced in the testis for the cells to reach the sperm. If spermatozoa are produced in lower numbers, they may not reach the ejaculate, but may well be present directly in the testis.
In order to determine the root cause of azoospermia and assess the likelihood of resumption of fertility and further use of assisted reproductive methods, the doctor recommends the patient to undergo diagnostics - in particular, a testicular biopsy. This procedure often helps to find mature spermatozoa in the tissues, and also allows to determine the treatment tactics.
Diagnostics of the azoospermia
In order to succeed in the treatment of azoospermia, it is necessary to identify the underlying cause of the disorder. Interviewing the patient begins with the collection of anamnesis: the doctor needs to know about some features of the patient's sexual life, for example - the degree and quality of sexual activity, the duration of the period during which it is not possible to conceive a child. In addition, such points as transferred or existing pathologies, bad habits, occupational intoxication, etc. Become important information. Next, the specialist evaluates the external data of the man: the features of the physique, the condition of the genitals, the degree of secondary sexual characteristics.
In many diagnostic centers, a diagnosis of azoospermia is made only after at least two microscopic examinations of semen confirming the absence of male sex cells. If necessary, additional diagnostics are prescribed:
- Prostate ultrasound, seminal vesicles, testicles, etc.;
- Testicular measurement with an orchidometer and other measuring devices;
- Spermogram (performed at least twice with a time interval of 2-3 weeks);
- A blood test showing levels of follicle-stimulating hormone (FSH), testosterone, prolactin, inhibin B;
- Genetic studies (karyotype, CFTR gene, AZF-factor).
In addition, tests are performed to determine sexually transmitted diseases. Non-obstructive azoospermia is indicated if FSH levels rise to 7.6 MF/L or more, with a general disorder of testicular development.
Instrumental diagnostics can be extended. Transrectal ultrasound of the prostate gland, ultrasound Doppler ultrasonography of scrotal vessels are performed.
The spermogram is complemented by MAR-testing, which is accompanied by an assessment of the content of anti-sperm antibodies in the blood.
Of particular importance is the determination of hormonal status, which helps to assess the quality of pituitary-hypothalamic regulation of the functionality of the sex glands.
As we know, sexually transmitted infections can also negatively affect the quality of semen in men. To rule out such pathologies, ELISA, RIF, or polymerase chain reaction (PCR) tests are performed.
In order to exclude the entry of sperm fluid not into the urethra but into the bladder (so-called retrograde ejaculation), a post-ejaculatory urine examination is performed.
Testicular biopsy for azoospermia.
If there are no contraindications, biopsy is performed in the standard way: a puncture of the testicular wall is made with a thin needle, after preliminary general or local anesthesia. The whole procedure lasts only a few minutes. If the anesthesia was local, the patient is released home within an hour.
In some cases, it is necessary to perform a so-called "open" biopsy: this method is used if a larger amount of tissue needs to be taken for examination. During the procedure, a skin incision is made in the scrotum (up to 10 mm), then take the desired amount of tissue. The manipulation is completed by applying one or more sutures (usually using absorbable threads). The patient can go home after 2-3 hours, or remain in the hospital (if further medical supervision is required).
The microsurgical method of testicular biopsy, which involves making a larger skin incision in the scrotum, is less commonly practiced. This technique allows a complete revision using a surgical microscope.
All of these methods require simple but special preparation of the patient. The doctor collects the results of pre-procedural tests in advance, discusses with the anesthesiologist possible methods of anesthesia. He talks to the patient, explains the essence of the procedure, finds out if he has implants, artificial valves, pacemakers, asks about medications, especially those that thin the blood (acetylsalicylic acid, warfarin, etc.).
The immediate preparatory stage is as follows:
- The evening before the procedure should not overeat, it is advisable not to have dinner, or eat something light (cottage cheese, some vegetables, etc.);
- Do not drink or eat on the day of the biopsy;
- Wash in the shower in the morning, shave off the hair in the scrotum and anterior thigh area.
The materials obtained during the biopsy go directly to the embryologist. He assesses the man's chances of successfully conceiving a child, conducts additional studies, consults with a reproductologist, geneticist.
Cytogenetic study of the karyotype of a male with azoospermia
Men who have difficulty conceiving and have a somatically adequate karyotype have a risk of developing sperm aneuploidy, a disruption of chromosome number in the diploid set, with a frequency of chromosome defects in the germline ranging from 6 to 18%.
It is difficult to overemphasize the role of chromosome Y in sperm formation. But diagnostics that allows to detect chromosomal changes and their impact on the decrease in the number of male germ cells is currently difficult. It is known that the development of infertility is closely related to the absence of chromosome Y in the gene material.
In azoospermia, genetic defects in the Y chromosome are found in about 35-50% of cases.
The following chromosomal defects can lead to impaired spermatogenesis:
- Chromosome number disorder (XXY, YYY);
- Structural chromosomal abnormalities;
- Chromosomal translocations.
Karyotype in azoospermia and other similar disorders are examined in such cases:
- In secretory azoospermia with elevated serum FSH levels;
- In oligospermia with a rate of less than 5 million sperm per 1 ml of semen;
- Teratozoospermia (presence of a large number of dead sperm in the sperm fluid).
In azoospermia, a 47,XXY karyotype change is often detected: an additional X chromosome is observed in patients with cryptorchidism and Klinefelter syndrome. In all metaphases, a Robertson translocation is detected (chromosome 13, 14, as well as 47,XY, -13, rob. T. (13,14).
Presumably, in such cases, the translocation is characterized by late development, since there is no evidence of congenital and hereditary nature of fertility disorders and chromosomal abnormalities.
The types of chromosome defects in men with diagnosed azoospermia are shown in the Table: [5]
|
Karyotype |
% of cases of patients with azoospermia |
|
46, XY. |
More than 92% |
|
Chromosomal abnormalities |
Less than 8% |
|
Classic 47, XXY |
About 2% |
|
Full Form 48, XXYY |
Less than 1% |
|
Mosaic variant 46, XY/47, XXY |
Less than 1% |
|
Clinical variant 47, XXY |
Less than 1% |
Differential diagnosis
Characteristic features that are identified during the examination of a man with primary testicular dysfunction:
- Insufficient expression of secondary sexual characteristics;
- Gynecomastia;
- Undersized testicle (less than 15 cm);
- The testicles are dense or absent;
- FSH is elevated or within the normal range.
Obstructive azoospermia is detectable:
- Testicular volume norm;
- Enlargement, density of the appendage, the presence of nodules in it;
- History of surgery to remove neoplasms in the appendage, or sterilization;
- A picture of urethroprostatitis;
- Prostate defects, enlarged seminal vesicles;
- Endocrine system, hormonal balance are within normal limits.
In case of cryptorchidism, the testicle does not descend into the scrotum, the signs can be detected at birth. Unilateral or bilateral pathology is possible. Microscopic calcification of the testis may develop, which becomes a risk factor for tumor development. [6]
For varicocele:
- The growth and development of the testicle is impaired;
- The venous vessels of the seminal canal are dilated mainly on the left side;
- There is pain and discomfort in the testicle.
|
Azoospermia |
Varicocele | |
|
External inspection |
The testicles are reduced in size, inelastic. |
Varicose dilated venous vessels of the seminal canal are present. Positive Valsalva test. |
|
ULTRASOUND |
Changes in the structure of the testicles and appendages are noted. |
Varicose dilated venous vessels of the bunched plexus are visualized. |
|
Spermogram results |
Signs of azoospermia. |
Signs of asthenozoospermia. |
Who to contact?
Treatment of the azoospermia
The main direction of treatment of azoospermia is to stimulate the natural development of male germ cells. However, therapeutic manipulations can be different, which depends on the root causes of the disorder. [7] Most often the doctor recommends to the patient such therapeutic techniques:
- Hormonal treatment - involves taking estrogen and LH (luteinizing hormone) preparations to stimulate spermatogenesis. The duration of such therapy is prescribed on an individual basis and most often lasts several months, up to six months.
- Surgical treatment is used for obstructive disorders that provoke azoospermia. Reproductive function is restored after the correction of patency: for example, the surgeon eliminates congenital developmental defects, varicocele and so on.
- Sperm extraction by biopsy is performed when all the above methods have failed to solve the problem. Doctors extract active spermatozoa from the seminal canal cavity and use them for artificial insemination.
Patients with azoospermia caused by pathologies such as varicocele, cryptorchidism, prostate cyst, require surgery.
If the problem is a consequence of inflammatory processes in the reproductive system, then anti-inflammatory drug treatment is carried out.
Disruption of hormonal balance is stabilized by appropriate hormone therapy.
In all cases, the treatment regimen is determined and selected individually, because it is important to take into account many characteristics of both the patient and the state of his health in general. If the treatment does not bring the desired effect, it is possible to help the couple by performing microsurgery, which allows to obtain male sex cells from testicular tissue. The obtained biomaterial is delivered to embryologists who select spermatozoa for subsequent artificial insemination. [8]
Is azoospermia treatable or not?
Azoospermia can be treated if the cause of the problem can be eliminated. For example, if the pathology is provoked by obstruction - blockage of the seminal canal, then a reconstructive operation is performed, which may include urethral plasty, anastomosis, surgical removal of varicocele, etc.
Treatment success after surgical correction of obstruction is observed in about 30-55% of cases.
If azoospermia was a consequence of endocrine, hormonal disorders, then therapy of hormone-replacement or stimulating nature is carried out. There are many cases of full-fledged male germ cells appearing in the sperm after a course of hormonal therapy.
If pregnancy in azoospermia does not occur despite all the measures taken, the patient is recommended to consult a reproductologist for an artificial insemination procedure - for example, ICSI (sperm injection into the cytoplasm). The technique involves obtaining sperm from the testis or appendage by open or aspiration biopsy.
In complicated cases, when it is considered impossible to detect and eliminate the cause of azoospermia, the only option is to use donor sperm for conception. [9]
Medications
In secondary hypogonadism for treatment use preparations of chorionic gonadotropin: hCG, Choragon, Pregnyl, Profazi, etc., in a dosage of 2 thousand IU three times a week. Menotropin is also administered in the amount of 0.5-1 ampoule in the form of intramuscular injections three times a week.
Complementary Medications:
- Cephalosporin antibiotics (Cefazolin, Cefotaxime 1.0 twice a day;
- Uroseptic agents of fluoroquinolones group (Ciprofloxacin 250 mg twice a day);
- Local anti-inflammatory drugs (Vitaprost suppositories 1 pc. In the rectum in the evening before bedtime);
- Analgesics (Ketonal 2.0 intramuscularly, Analgin 1.0, Nospazine 2.0 intramuscularly);
- Drugs to optimize microcirculation (Pentoxifylline 5.0 as an intravenous drip);
- Antimycotic agents (Fluconazole 150 mg once a day, Intraconazole solution);
- Ascorbic acid 2.0 daily for four days.
The indicator of positive dynamics of treatment is the disappearance of pulling pains in the groin area, the presence of single spermatozoa during spermogram, the absence of inflammatory processes. Spermogram and hormonal tests are repeated with an interval of 4 weeks.
Tribestan
The treatment of endocrine forms of azoospermia is often carried out using preparations of plant origin. Currently, there is a particular interest in phytomedicines, which are both effective and safe. Plant preparations usually combine a mild complex effect and the absence of pronounced side effects, as well as the possibility of use in conjunction with traditional medicines.
There are a number of herbal preparations containing saponins, or so-called steroidal glycosides, capable of gently regulating the hormonal balance in the male body. It is noteworthy that such remedies correct the disturbed work of endocrine glands, without affecting the normally functioning glandular system.
One of the means in the composition of which saponins are present is Tribestan. The drug is actively used to correct libido and fertility disorders in men.
The rich complex composition of Tribestan provides multistage action of the drug, which is reflected at the level of the pituitary gland, sex glands, adrenal cortex. With the help of saponins and sapogenins, the function of endocrine glands is stabilized, and alkaloids help to dilate blood vessels, accelerate blood circulation in the sexual system.
Tribestan affects hormonal balance, has an indirect estrogenic effect without interfering with regulatory mechanisms.
In addition, the drug has a positive effect on the psycho-emotional balance, improves the state of the autonomic nervous system, optimizes well-being, reduces fatigue, increases physical and mental performance. It is important that Tribestan is safe, non-toxic, does not cause functional and morphological changes. It can be used as a monotherapy or in combination with hormonal drugs.
Men with azoospermia are recommended to take Tribestan 1-2 tablets three times a day, for at least three consecutive months. The therapeutic course may be repeated until the required positive effect is achieved.
As a rule, the treatment is well tolerated, no cases of overdose and pronounced side effects have been noted. Allergic reactions were rarely detected.
Spermactin
Scientists have found that taking drugs containing antioxidants and trace elements in many cases helps to increase the chances of fertilization and reduces the risk of reproductive disorders. The most widespread and interest from the side of specialists received medication complexes that affect different types of disorders of spermatogenesis (including azoospermia). Doctors have noted the effect of Spermactin, acetyl-L-carnitine, L-carnitine fumarate and alpha-lipoic acid complex on oxidative stress values and the degree of DNA fragmentation of male germ cells.
Numerous studies have revealed positive statistically significant dynamics of basic spermogram values, in particular motility and morphology. Stable improvement was observed already closer to the third month of the therapeutic course. At the same time, the free radical count decreased. The main conclusion was made: stimulation of spermatogenesis with the complex preparation Spermactin is an effective and safe way to correct male reproductive function.
The drug is taken one sachet (10 g) in the morning immediately after breakfast. The powder should be diluted in 150-200 ml of water or juice (milk, hot tea and alcohol-containing drinks are not suitable).
In rare cases, Spermactin can cause an individual hypersensitivity reaction. If this happens, the complex remedy is canceled and replaced with other, more suitable drugs.
Selzinc
For adequate functioning of the male reproductive system, it is important to maintain a physiological level of concentration of vitamins and trace elements that take part in biochemical reactions and are their catalysts. Some essential micronutrients are produced by the male reproductive organs. The most important elements for normal fertility are considered to be zinc and selenium ions.
Today, many patients have vitamin and microelement deficiency in the body. In particular, this is associated with nutritional disorders, with a lot of bad habits and unfavorable environmental conditions. Uniform and limited nutrition quite quickly entails a decrease in the intake of useful substances and, as a consequence, the development of various pathological conditions.
Zinc controls gene expression during cell proliferation and differentiation, and is involved in sensitization to hormones and growth factors. Zinc deficiency is particularly affected in the early phases of the cell cycle. It is its deficiency that causes delayed sexual development in adolescents and decreased male fertility. Interestingly, zinc tends to accumulate in the prostate gland and serves as one of the ingredients of the secreted fluid. It helps regulate the activity of spermoplasmic enzymes, takes part in the processes of coagulation and liquefaction of seminal fluid. The presence of zinc in male germ cells is the highest in the whole organism and amounts to 1900 µg/kg.
Another trace element, selenium, has a protective effect against biochemically aggressive free radicals. Selenium is necessary as an antioxidant defender of cell membranes, stimulates the work of other antioxidants. In case of deficiency of this trace element, male infertility develops, as it not only provides protection of male germ cells, but is also responsible for their motility.
Many studies have confirmed the effectiveness of Selzinc in relation to sperm concentration, motility and morphology in men suffering from fertility disorders. This drug remains absolutely safe even when taking two daily doses, and no side effects and symptoms are noted. Selzinc is taken one tablet daily, for several months (at the discretion of the doctor).
Prostagut forte
Polycomponent herbal remedy Prostagut forte is used for azoospermia associated with benign prostatic hyperplasia and prostatitis. The drug is considered absolutely safe, and at the same time is not inferior in effectiveness to known synthetic drugs.
The composition of the product is represented by an extract of serenoa creeping berry and Sabal palm, as well as a dry extract of the rhizome of nettle creeping.
Prostagut forte is characterized by a pronounced anti-inflammatory, anti-edematous effect, the ability to inhibit cellular development by suppressing RNA production. Additional properties of the drug: stimulation of the nervous system, inhibition of testosterone consumption by prostate cells. The active composition of the drug helps to reduce in patients painful and burning sensations during urinary excretion in benign prostatic hyperplasia.
The drug does not directly affect the cure of azoospermia.
Capsules of the medicine are taken orally, in whole form, with water. Duration of treatment - at least one month, one capsule in the morning and evening. Prostagut is well tolerated, side effects in the form of unpleasant sensations in the abdominal area rarely occur. Some patients may develop allergy to the drug.
What can be concluded? The drug Prostagut forte has an effect only on the external manifestations of disorders, but directly azoospermia, as well as the growth of prostate neoplasms, this medication is not able to cure. However, as part of a comprehensive treatment, the drug can be used.
Physiotherapy treatment
Medical and surgical methods are not the only way to get rid of azoospermia. Doctors use current, laser, magnetotherapy as an addition to the main therapeutic methods, which allows for a better restoration of male fertility.
Meanwhile, the effectiveness of physical procedures is not always noted: they help if it is necessary to cure chronic genitourinary pathologies, or to accelerate the recovery of the body after surgery. The main effect of such procedures is to increase or decrease the tone of muscles, dilate vessels, improve microcirculation, block sluggish inflammatory processes.
Physiotherapy is not prescribed for acute inflammatory reactions, infectious processes, suspected malignant tumors, as well as in periods of fever, with a severe course of systemic pathologies.
- Vacuum massage is the most popular procedure for the treatment of azoospermia and is a local negative pressure technique called LOD therapy. The procedure involves placing the penis in a special baro-chamber from which air is slowly pumped out. As a result, the penis area is actively flowing blood, there comes a state of erection. After restoring the pressure, the procedure is repeated. Such a specific massage is prescribed if azoospermia in a man is combined with erectile dysfunction. What gives such treatment? Prevents blood stasis, improves microcirculation, enriches the organs with oxygen, which has a positive effect on the work of the prostate and testicles. The method is contraindicated in patients with a pronounced varicocele, inguinal hernia, as well as at increased risk of blood clots.
- Laser therapy involves the use of a low-intensity laser that does not destroy tissue: the red range of radiation reaches a depth of two millimeters, and infrared - up to eight millimeters. The main property of laser therapy is immune stimulation, optimization of metabolic processes, blocking the inflammatory response, activation of testosterone production, which directly affects the motor activity of spermatozoa.
- Magnetic therapy normalizes the vascular network, stabilizes hormone production, has hypotensive and antitumor effects.
- Electrostimulation involves the application of pulsed currents that cause the muscles to contract. With the help of electrophoresis, drugs are delivered to the required area - in particular, enzyme and anti-edema drugs. This method of drug delivery to the tissues helps to increase the concentration of the drug in the necessary area of the body, to reduce the severity of side effects. Electrostimulation is not prescribed to patients with tumor processes, complex inflammatory diseases, as well as in the presence of skin lesions in the area of the procedure.
Other physical therapy techniques for azoospermia may include:
- Ozone therapy;
- Mud treatment;
- Transurethral microwave therapy.
The methods can be used alone or in combination with each other.
Herbal treatment
Folk remedies for azoospermia are usually ineffective. However, in some cases, medicinal plants in combination with lifestyle and dietary changes help to slightly improve the quality of seminal fluid.
If there are problems with spermatogenesis, it is recommended to brew and drink an infusion of hawthorn fruit every morning, afternoon and evening instead of tea. In addition to it, herbal teas of elderberry and hollyflower help well.
To restore the quality of semen grate carrots, squeeze 100 ml of juice and mix it with two tablets of mumie. The drug is consumed daily before breakfast. Additionally, during the day you should drink an infusion of the herb ergot. The course of such treatment continues for a month.
Boil 2 tablespoons of Adam's root plant with boiling water. After cooling, the remedy is filtered and used 1 tbsp. Daily.
Prepare a herbal collection based on walnut leaves, pine shoots, Icelandic moss and white mulberry. Ingredients are taken in equal amounts. Then 2 tbsp. L. Of the mixture is poured boiling water (450 ml) and insist in a thermos for half an hour. Then strain and take 150 ml instead of tea three times a day. You can add honey and lemon juice.
A good effect is characterized by a tincture of lapchatka. To prepare it, take the rhizome of the plant (100 g), pour 0.5 liters of vodka, insist for two weeks. Then the tincture is filtered and taken one teaspoon three times a day, between meals, drinking a small amount of water.
Folk healers advise to eliminate azoospermia season food with dried and fresh basil, or drink an infusion of leaves. To prepare an infusion of 20 g of fresh basil leaves poured 250 ml of boiling water, insist for half an hour. The remedy is drunk three times a day for half an hour before breakfast, lunch and dinner.
The products of beekeepers - in particular, royal jelly in combination with honey - also do a good job. Such a mixture is eaten one spoonful immediately after a meal, holding it in the mouth until it dissolves completely. It is not necessary to drink water or other liquids.
Surgical treatment
In the case of azoospermia, a pathology in which the ejaculate lacks spermatozoa, surgical methods are used to obtain male sex cells. These methods include PESA, TESA and TESE.
The first two methods, PESA or TESA, are most commonly practiced by specialists. The TESE technique of bilateral testicular biopsy using microsurgical technology is used to treat non-obstructive azoospermia. [10]
- PESA is a needle biopsy performed in several areas of the testicular appendages. PESA is a needle biopsy performed in several areas of the testicular appendages and is considered 100% effective in the presence of vas deferens obstruction, but the procedure itself can further worsen the degree of vas deferens blockage.
- The TESA technique involves performing a needle biopsy in several areas of the testicles. It is a minimally invasive procedure that successfully obtains the required number of spermatozoa. However, the method has its disadvantages: it is effective only if there are foci of spermatogenesis, but even existing foci can not always be detected due to the lack of visual control of the tissue structure. If the doctor performs up to six punctures on each testicle and no male germ cells are found, a TESE microsurgical puncture is recommended.
- TESE is the aspiration of testicular tissue for further sperm extraction. This technique is considered to be the most effective. First, a biopsy is performed, and spermatozoa are separated from the extracted biomaterial. Practice closed puncture, for which a special gun is used: this procedure is characterized by frequent complications and relatively low efficiency. The most common is bilateral microsurgical multifocal testicular biopsy, which is often used in patients with nonobstructive azoospermia.
Pregnancy with azoospermia
Before making predictions about the possibility of fertilization of a woman with azoospermia in a man, the doctor must analyze the results of diagnosis, determine the type and find the cause of the disorder. Only after that, the optimal tactics of subsequent measures are developed in order to achieve pregnancy and the birth of a healthy child for the couple.
If a patient is diagnosed with obstructive azoospermia, it is possible to restore fertility with the help of a surgeon. Microsurgical reconstruction is performed to open the vas deferens, the subtleties of which depend on the location and extent of the obstructed area.
The case with secretory azoospermia is somewhat worse, because with such a diagnosis, the chances of successful treatment, although there are, but they are not so great. Nevertheless, some hormonal malfunctions can be eliminated with conservative treatment aimed at stabilizing the endocrine system and correcting spermatogenesis. If the root cause of azoospermia was the expansion of the scrotal vessels, then infertility can often be cured by surgery.
For many patients, the chances of cure are still slim. In such a situation, if the doctor sees that there is no prospect of ongoing therapy, the use of assisted reproductive methods - in particular, IVF - may be recommended. This technology has been successfully used by reproductologists for more than four decades, and over the years, the effectiveness of the method has been increasing.
IVF for azoospermia
Today, specialists successfully use the technique of extracting male germ cells directly from the testicle for their further use in in vitro fertilization (ICSI) programs. The technique of sperm extraction is biopsy. This procedure results in a long-awaited pregnancy in about 30-60% of cases.
The effectiveness of the biopsy may vary, depending on the severity of the azoospermia. In order to provide a clearer individualized treatment prognosis, a thorough examination of the patient is carried out. The doctor receives preliminary information about the type of pathology, thanks to which he assesses the chances of fertilization success.
There are different biopsy techniques: the doctor selects the most appropriate one that will be extremely effective in a particular situation.
Prevention
Preventing the development of azoospermia and preventing reproductive health disorders in men is, first and foremost, about leading a healthy lifestyle. Doctors should motivate their patients and explain to them the necessity of avoiding bad habits.
Doctors recommend:
- Refuse to engage in promiscuous sexual activity, do not have unprotected sexual intercourse with a questionable partner;
- Refuse to drink alcoholic beverages, use drugs or smoke;
- Practice reasonable moderate physical activity, avoid both hypodynamia and excessive physical activity;
- Periodically visit a doctor for preventive examinations, timely treat any infectious and inflammatory processes in the body;
- Not to forget to get adequate rest and sleep;
- Avoid conflict and stressful situations.
In addition, it is important to remember that in order to maintain male fertility, it is undesirable to abstain from sex and to have sexual intercourse too often. It is optimal to have sexual intercourse once every 3-4 days.
Forecast
The success of treatment for azoospermia depends on many factors. These are, first of all, the age and general state of health of the patient, his lifestyle. If a chromosomal defect is detected, then the specialist may insist on additional genetic diagnosis, which is necessary to assess the degree of risk for embryos. In addition, the prescription of hormonal agents requires a clear control of treatment: if you do not adhere to the scheme of taking such drugs, it can significantly and negatively affect the effectiveness of therapy.
The overall prognosis is as follows: patients with obstructive azoospermia have a better chance of conceiving after treatment, both naturally and using assisted reproductive technologies. Secretory azoospermia is more difficult to treat, but even here there are some chances of success of the therapy. The main thing is the fulfillment of all recommendations and prescriptions of the doctor, the exact adherence to the scheme of treatment. Only in this case it is possible to achieve the appearance and persistent presence of male sex cells in the sperm fluid, and further - and successful conception.
The most hopeless type of disorder is considered to be azoospermia, developed as a result of epidparotitis, or mumps. The worst prognosis is noted in the genetic or idiopathic form of pathology.

