Medical expert of the article
New publications
Vasoresection and vasectomy in men: what is the difference?
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Surgical intervention on the male reproductive system, in particular on the vas deferens – vasoresection – is considered a method of permanent male contraception through sterilization (i.e. the absence of sperm in the seminal fluid).
The essence of this procedure is the excision of a part of the vas deferens, making it impossible for sperm to enter the ejaculate, which achieves a state of programmed excretory azoospermia, and as a result, men lose fertility - the ability to fertilize. After vasoresection, the testicles still produce sperm, but their movement is blocked. But all sexual functions, primarily erectile, are preserved.
This operation has another name, more common among doctors - vasectomy. Vasoresection and vasectomy, what is the difference between them? These are synonymous terms. Vasoresection: from vas (Latin - vessel) and resectio (Latin - cutting off), and vasectomy - from vas (Latin - vessel) and ektome (Greek - excision, removal).
Indications for the procedure
Among the indications for this operation, first of all, is the man's decision not to have offspring at all, or if there are enough children in his family and he does not want to increase it. Perhaps, as a result of genetic counseling, it was discovered that the man has chromosomal mutations, or there are severe congenital Y-linked pathologies in his family, and there is a fear of their transmission along the male line.
In addition, the decision to have a vasectomy may be due to the fact that, due to the wife’s health condition, pregnancy is associated with a threat to her life and is therefore highly undesirable.
Medical indications for vasoresection: tuberculous lesion of the vas deferens or its abscessing inflammation (deferentitis), as well as recurrent inflammation of the epididymis - epididymitis, developing with chronic inflammation of the seminal vesicle - vesiculitis (spermatocystitis).
Abroad, vasoresection (vasectomy) in men has become a fairly common method of preventing unwanted pregnancy in women in the last 40 years (according to WHO, approximately 40-60 million men worldwide have undergone this procedure).
In the USA, according to official information, husbands have undergone vasectomy in almost 10% of married couples with children. Approximately the same figures are in Canada, Great Britain, and the Netherlands. And in first place in terms of vasectomy is New Zealand, where 25% of all married men prevent the birth of children in their families.
It should be borne in mind that a vasectomy is likely to be irreversible, so potential patients should be warned about this. Although the functions of the vas deferens can be restored surgically, for which a reverse vasectomy is performed (reversal of a vasectomy). However - despite all the achievements of microsurgery - such an operation is still technically very complex and only in 40-45% of cases leads to the desired result. At the same time, as surgeons say, an attempt at a reverse vasectomy has a greater chance of success if it is carried out no later than five years after sterilization.
Preparation
Preparation for vasoresection includes blood tests (general, for STDs, HIV, hepatitis viruses and coagulation - coagulogram) and urine tests (general), as well as an ultrasound of the urogenital area and an ECG.
About two weeks before the procedure, stop taking acetylsalicylic acid (Aspirin) and other blood thinning medications (Warfarin, any NSAIDs).
For three days before the operation, it is recommended to wash the scrotum and surrounding areas with antibacterial soap, and shave the hair in the genital area. In the morning of the operation, take a shower, and bring clean, tight-fitting underwear (to support the scrotum and minimize postoperative swelling).
 [ 1 ]
[ 1 ]
Technique vasoresection
Vasoresection is performed under local anesthesia – injection of local anesthetic (for some patients, sedation is additionally used); the duration of the operation is up to 30 minutes.
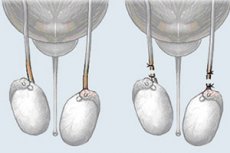
The urological surgeon, through a small incision in the lateral inguinal fossa, performs a longitudinal split of the muscle that lifts the testicle and exposes the spermatic cord, separating the vas deferens and vessels in it (they are held together with the perivasal tissues by a clamp).
Next, the vas deferens is vasoligated: it is tied in two places (at a distance of up to two cm) (i.e. ligatures are applied). After which the duct is dissected in the middle of this gap, and the ends are either buried in nearby tissues and secured with an absorbable suture (this is called fascial interposition), or cauterized using electrocoagulation. An open vasoligature technique can be used, when only the part of the duct leading to the penis is blocked (ligated).
The wound is closed by layer-by-layer suturing; interrupted sutures are applied to the skin, pulling the edges of the incision together.
Similar manipulations are carried out on the second duct (from the opposite side).
There is a technique for performing vasoresection through one incision, as well as minimally invasive vasectomy - without a scalpel, through one small puncture of the skin of the scrotum (using a special instrument).
Contraindications to the procedure
Vasoresection is contraindicated in hemophilia and poor blood clotting caused by thrombocytopenia or diabetes mellitus. Contraindications also apply to cases of:
- the presence of sexually transmitted diseases and other urogenital infections that are transmitted through sexual contact;
- testicular diseases (orchitis, epidedymitis, orchoepidymitis, etc.);
- fungal and bacterial urethritis;
- chronic cystitis;
- tumor formations in the pelvic area.
Consequences after the procedure
Having studied the complaints and reviews of patients after vasoresection, specialists have compiled a list of short-term (quite quickly passing) consequences of this procedure and complications that arise later.
Most often, the consequences after the procedure manifest themselves in the form of pain in the scrotum (normally - for several days) and local hematomas and swelling of tissues in the genital area (up to two weeks).
Also after vasoresection there may be minor bleeding (as evidenced by the presence of bloody discharge from the penis or blood in the ejaculate). The development of a secondary bacterial infection (with an increase in body temperature to +38°C) is not excluded.
Complications after the procedure
Delayed complications after the procedure may include chronic orchialgia (testicular pain), which is reported by 1-3% of patients.
When the vas deferens is blocked due to increased pressure in the epididymis, varicocele may develop, accompanied by a feeling of pressure in the testicles and a pulling pain. Hydrocele formation around the testicle is also noted, which causes swelling in the scrotum and dull pain that intensifies during ejaculation. For the same reason, the duct in the epididymis stretches and ruptures (usually asymptomatic).
Due to the weakening of the ligature, spermatozoa continue to flow into the scrotum through the cut vas deferens, and after two to three weeks, spermatogenic (spermatozoal) granulomas may form. Most often, they are not felt by patients and resolve over time, but if the granulomas are large (less than 1% of cases), treatment (steroid injections) or surgical removal are necessary.
Congestive epididymitis (in 2.8-5.6% of cases) and abnormal cysts (spermatoceles) that form on the epididymis are possible.
Approximately 50-80% of men (according to the European Association of Urology, 52-68%) develop an immune reaction against their own spermatozoa after vasoresection, i.e. antisperm antibodies are detected in the blood. This can provoke inflammatory processes, since the body's own antibodies form circulating immune complexes that cause the same reaction as in the presence of an infection. It is for this reason, as foreign studies have shown, that vasectomy in the first years after surgery increases the risk of developing diseases of the genitourinary system.
Care after the procedure
What is the post-vasectomy care?
It is necessary to: stay in bed for at least two days; apply cold to the scrotum area (to prevent hematomas and swelling) – especially in the first 24 hours; keep the genital area clean, perform hygiene procedures; wear tight underwear or a support bandage.
Alcohol is excluded for at least two weeks, and any physical activity is excluded for a month and a half. Sexual activity can be resumed a couple of weeks after the operation, but the man or his partner should use other methods of contraception until the success of the vasoresection is confirmed by the results of the post-vasectomy sperm analysis (PVSA).
Patients can stop using other methods of contraception when PVSA shows azoospermia, or the presence of only single immotile sperm (RNMS or ≤ 100,000/mL), according to the American Urological Association.
Changes in the human body after vasoresection
After vasoresection, the man's body continues to produce both testosterone and pituitary gonadotropins. The physiology of the reproductive system does not change, that is, sexual problems (such as impotence) do not arise, since the nerves involved in erection and ejaculation are not affected.
Even the production of seminal fluid and spermatogenesis continues, but the man will not notice a decrease in sperm volume, since the spermatozoa that do not find an “exit” are utilized by macrophages in the lumen of the epididymal tubules.
True, there may be an increase in the thickness of the walls of the vas deferens due to interstitial fibrosis, and in 35% of patients, scar tissue forms at the site of their excision.
Vasoresection as a method of male contraception does not guarantee 100% effectiveness. For example, according to British doctors, pregnancy of the partner occurs in one out of two thousand patients who decide to undergo this operation.
 [ 13 ]
[ 13 ]

