Medical expert of the article
New publications
Duodenal bulb ulcer: acute, chronic, mirror ulcer
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

When we feel pain in the stomach area, we most often attribute this symptom to it. Inventing various reasons (stale or indigestible food, poisoning with drugs or chemicals, incipient gastritis or even a stomach ulcer), we do not think that the cause of pain and discomfort in the abdomen may not be related to the stomach at all. The nature of the pain, as well as the results of a gastroscopic examination, which clearly show erosions on the mucous membrane of the initial section of the intestine adjacent to the stomach, allow the doctor to make a diagnosis of "ulcer of the duodenal bulb" with great accuracy, and thereby completely confuse us.
Let's figure out what kind of organ it is in the digestive system, what its functions are and why ulcers form on its mucous membrane, causing such unpleasant sensations, reminiscent of the symptoms of gastritis with high acidity. And we will also try to understand how to identify and effectively combat peptic ulcer disease affecting the stomach or duodenum, and often both organs at once.
Some anatomy
The digestive system is one of the most multifunctional and longest systems in the human body. It includes many organs that perform the functions of grinding, moving, digesting and assimilating food. Some organs, such as the intestines, have such a complex structure that its different sections perform different functions related to the work of the gastrointestinal tract. The initial section of the intestine is called the duodenum (DPC), which got its name due to its length (about 12 fingers folded together).
The upper (initial) section of the duodenum is a kind of continuation of the pylorus of the stomach, which performs the function of further transporting food through the gastrointestinal tract. Due to its unusual shape, reminiscent of an onion head, and its size, which is about 5 cm, it is called the bulb of the duodenum. Its function is to regulate the acidity of the stomach contents for its safe movement to the lower sections of the intestine, i.e. to protect the intestine from irritation.
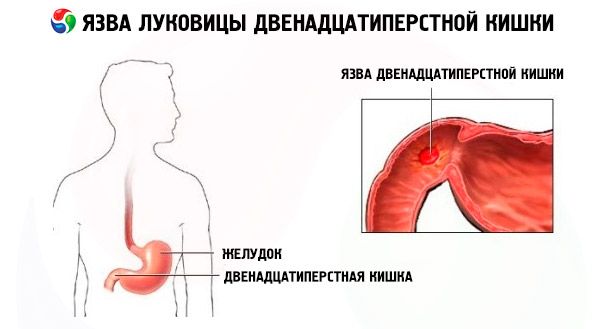
An ulcer of the duodenal bulb can not only bring a certain discomfort to the life of a patient with this diagnosis, but also prevent the initial section of the intestine from performing its function, as a result of which the rest of the digestive system will suffer.
Epidemiology
Epidemiological studies show that most often, duodenal bulb ulcers develop against the background of gastric ulcers, which is quite understandable due to the proximity of these organs and the functions they perform. Therefore, the diagnosis in most cases sounds like "gastric ulcer and duodenal ulcer."
Ulcerative lesions of the gastrointestinal tract are a fairly common disease, affecting about 3-5% of the adult population worldwide. At the same time, this pathology occurs in men almost 4 times more often than in women. In addition, the course of the disease in young women is characterized by a mild pain syndrome, although all other symptoms are present in full.
Ulcer of the duodenal bulb can be considered a disease of the young, in contrast to gastric ulcer, which often develops in old age.
By the way, city dwellers suffer from ulcers twice as often as villagers and towns. Perhaps the reason lies in the food preferences of city dwellers and the increased stress associated with work and difficulties in everyday life, especially in large cities.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
Causes duodenal ulcers.
Both stomach ulcers and ulcerative lesions of the duodenum are caused by an elevated level of hydrochloric acid, which sort of corrodes the mucous membrane of the organs. The stomach itself and the bulbous region of the initial section of the small intestine, which is designed to combat increased acidity, providing an alkaline environment for the chyme (semi-digested food) at the exit from the stomach, are most susceptible to the negative effects of acid in the gastric juice.
This means that it is the increase in acidity that, due to a number of reasons, causes the appearance of erosions on the mucous membrane of the duodenum. Based on this, the reasons for the development of the ulcer of the duodenal bulb can be considered the same reasons that contribute to the increase in the acidity of the gastric juice, in particular:
- increased secretion of a special hormone (gastrin) that regulates the digestive function of the stomach,
- poor nutrition with a large amount of bitter, salty, sour foods, uncontrolled consumption of fatty and fried foods, pickles, marinades, preservatives,
- a tendency to snack on dry food at the expense of a full breakfast and lunch, overeating in the evening,
- long-term use of certain medications, especially when taken orally. Most often, this applies to hormonal and anti-inflammatory drugs (corticosteroids and some NSAIDs),
- psychological trauma (both isolated stressful situations and regular nervous tension),
- bad habits such as smoking and alcoholism, which affect the normal functioning of the gastrointestinal tract due to their irritating effect on receptors.
Even a slight increase in the acidity of gastric juice creates the best conditions for the reproduction and increased activity of the Helicobacter Pylori bacteria, which causes the development of inflammatory processes in the stomach and duodenum. Therefore, such a stomach disease as gastritis often becomes the main cause of the development of an ulcer of the duodenal bulb. However, as well as duodenitis, which is an inflammation of the mucous membrane of the duodenum.
As for severe stress, it is one of the main reasons for the development of this pathology, although many patients are still inclined to deny the influence of nervous reactions on the development of gastrointestinal diseases, not recognizing the universally recognized truth that all diseases are from nerves.
Sometimes doctors diagnose ulcers on the mucous membrane of the duodenum, which appeared as a result of the development of such pathologies as increased calcium content in the body (hypercalcemia), insufficient functionality of the kidneys and liver, in particular with cirrhosis of the liver, COPD with difficulty breathing, chronic inflammation of the gastrointestinal tract (Crohn's disease). The presence of HIV infection in the body and some other diseases can also become real, albeit rare, risk factors for the development of an ulcer of the duodenal bulb. Doctors do not exclude a hereditary factor in the development of this pathology, which significantly increases the risk of its development among the patient's relatives.
Pathogenesis
Ulcer of the duodenal bulb is a chronic disease characterized by alternating periods of exacerbation and remission. There are 3 main stages of the disease:
- exacerbation stage (acute course of the disease) with pronounced clinical symptoms, the presence of ulcers and an inflammatory process on the duodenal mucosa,
- the stage of fading (or subsiding) exacerbation, when clinical manifestations are absent, but the inflammation still persists, and fresh scars form at the site of the ulcers,
- the stage of remission, when the inflammatory process is sluggish, but cicatricial changes on the mucous membrane remain.
In the pathogenesis of ulcerative lesions of the duodenal bulb, scientists attribute the main role to the imbalance between the agents of aggressive action and protection of the duodenal mucosa, in the direction of strengthening the former and reducing the activity of the latter. In a healthy person, such a balance is maintained by the coordinated work of various parts of the neuroendocrine system (this is the answer to the question of why nervous reactions affect the work of the gastrointestinal tract).
The discrepancy between the factors of aggression and protection within the body leads to the formation of erosions and ulcers on the mucous membrane of the gastrointestinal tract. In the case of an ulcer of the duodenal bulb, the decisive role is still played by the increased activity of the factors of aggression, among which we can highlight the increased acidity of the gastric juice due to the increased production of gastrin, the activity of the harmful gastric bacterium Helicobacter Pylori and other factors mentioned above.
Thus, an ulcer of the duodenal bulb is characterized by an increase in the tone of the stomach muscles and its increased peristalsis, an increase in the number of parietal cells of the stomach, which produce hydrochloric acid (НСl) and a violation of the inhibitory function, which limits the activity of the stomach glands to produce pepsin andНСl. This state of affairs is the cause of increased secretion of gastric juice even outside of meals and a sharp increase in the level of acidity of the stomach, leading to the destruction of the cells of the mucous bulb of the duodenum.
 [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ]
[ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ]
Symptoms duodenal ulcers.
Cases when the ulcer of the duodenal bulb occurs without symptoms corresponding to this disease are so rare that it is not worth dwelling on them. Usually, this pathology of the gastrointestinal tract is characterized by symptoms that are notably intense. In general, the manifestations of the ulcer of the duodenal bulb (duodenal ulcer) are similar to the main signs of a stomach ulcer (in particular, its pyloric section).
The first signs of a duodenal ulcer are severe pain localized in the navel area. They are easily relieved with antacids, which reduce stomach acidity. Depending on the physiological characteristics of the patient's body and the nature of the food consumed, the pain can be either sharp or dull aching. Pain (usually in the right epigastric region, radiating to the lower back) can occur at night or 1-2 hours after eating (late pain).
There are frequent cases of pain when the stomach is completely emptied of food residues. Eating removes such manifestations of the ulcer as "hunger" pains, as well as accompanying symptoms in the form of belching, nausea and even vomiting.
Belching and nausea can also be observed after eating, along with heartburn, a sour taste in the mouth, and a feeling of heaviness in the pit of the stomach and in the throat area.
A feeling of hunger that often arises out of nowhere, a short time after eating, can also be a symptom of a duodenal ulcer. As well as the appearance of constipation, cases of bloating and flatulence, which are characteristic of this type of ulcerative gastrointestinal tract lesion.
The symptoms of duodenal ulcers are characterized by periodicity of manifestation. Symptoms worsen in the spring and autumn, as well as under the influence of stressful situations. During periods of remission, the ulcer may not manifest itself in any way, even if the patient does not adhere to a special diet.
Mirror ulcer of the duodenum
Among the ulcerative lesions of the duodenum, one can distinguish such varieties as ulcers of the lower (descending) section, bulbous and mirror ulcers, when deep ulcers are observed not only on the mucous membrane of the bulb, but also on the opposite end of the duodenum.
Bulbous forms of pathology are considered the most common, but ulcers of the descending section are much less common.
Mirror ulcer of the duodenum is of particular interest. It is not a rare phenomenon, but its course is complicated by the presence of not one, but several ulcers, resulting in slow scarring of ulcers and frequent exacerbations. Along with the number of ulcers on the mucous membrane of the duodenum, the likelihood of developing various complications also increases.
This type of pathology is characterized by the same symptoms as with an ulcer of the duodenal bulb, but the localization of pain may be somewhat different. Most often, patients with a mirror ulcer complain of severe pain in the epigastric region on the left side. And sometimes the pain is localized in the left hypochondrium.
Complications and consequences
An ulcer of the duodenal bulb is a rather dangerous disease that cannot be ignored. The consequences of an irresponsible attitude to one's health against the background of the appearance of symptoms of a peptic ulcer can be various complications, both chronic, developing over a long period of time (penetration, stenosis, periduodenitis), and arising suddenly and posing a threat to the patient's life (bleeding and perforation).
Penetration of an ulcer is its spread to the area of nearby organs. In the case of a bulbous ulcer, there is a high probability of its expansion to the pancreas. Pain sensations change, girdle pains appear, which cannot be relieved by taking antacids.
Stenosis is a narrowing of the lumen in the initial section of the small intestine, where the duodenal bulb is located, which negatively affects the entire digestion process, making it difficult for food to move from the stomach to the intestine. Now the ulcer symptoms, depending on the stage of stenosis, are complicated by a constant feeling of heaviness in the stomach, pale skin, constant weakness, dry skin and mucous membranes, and general exhaustion. Belching changes its smell from sour to rotten, and vomit contains undigested food.
The further prognosis depends on the stage of development of the pathology. Compensated stenosis, if it is caused by functional disorders (edema or spasm during exacerbation of peptic ulcer), responds well to treatment. Subcompensated and decompensated forms of stenosis are already pathologies that are difficult to treat and life-threatening.
Periduodenitis is characterized by an inflammatory process in the serous membrane of the duodenum, which is a fairly common complication of ulcers and is often accompanied by the formation of adhesions and deformation of the duodenal bulb. Subsequently, the pathological process can spread to other organs (stomach, gallbladder, etc.), causing partial obstruction of the duodenum and other serious diseases that can cause limited ability to work.
I think there is no need to talk about the danger of bleeding. But they are the most common complications of the duodenal bulb ulcer. Almost every exacerbation is accompanied by hidden bleeding, which does not pose a particular danger, which cannot be said about obvious bleeding with a large loss of blood. They are characterized by bloody vomiting, loose stools, the color of which resembles tar, pale skin, weakness and other symptoms of acute blood loss.
Perforation is also one of the most common complications of duodenal ulcers, and in the male population this complication develops a couple dozen times more often than in the fair sex.
Perforation, or puncture, of the ulcer of the duodenal bulb is a through breach of the integrity of the duodenal wall, in which partially digested food can get beyond the intestine, causing inflammatory processes in the abdominal cavity (peritonitis). It is accompanied by sharp severe pain in the epigastric region, increased muscle tone of the abdominal wall, fever and other symptoms of pneumoperitoneum, and subsequently peritonitis.
Diagnostics duodenal ulcers.
When we feel pain in the lower part of the stomach, we rarely think about the fact that the painful condition may be associated with its continuation, which is the duodenum, or with the pancreas, located in the same area. It is almost impossible to diagnose an ulcer of the duodenal bulb or the development of the same pancreatitis on your own due to the symptoms and localization of unpleasant sensations similar to other gastrointestinal pathologies. Therefore, a gastroenterologist should make a diagnosis.
The symptoms of various types of gastric ulcer and duodenal ulcer are so similar that it is difficult even for a specialist to distinguish one pathology from another. However, an important point in differential diagnostics is the study of subjective symptoms from the patient's words: the frequency and localization of pain, the reaction to acid-reducing drugs, the presence of other dyspeptic disorders (nausea, vomiting, heartburn, etc.).
The study of the anamnesis should be accompanied by palpation, which will most likely help to determine the development of the ulcerative process. But it is possible to determine its localization only with the help of a set of studies, which include instrumental diagnostics, laboratory tests (complete blood count, biochemical blood test, stool tests: general and Gregersen reaction, tests to determine the level of gastrin and tests for the presence of Helicobacter Pylori), histological studies and other diagnostic methods.
The most popular and accurate methods of instrumental diagnostics that allow you to determine the location of the ulcer and make a final diagnosis are esophagogastroduodenoscopy and radiography of the abdominal organs. The first method is not only more accurate, but also the most informative, because it allows you not only to assess the condition of the gastrointestinal mucosa and determine the localization of ulcers and large ulcers, but also the degree of development of peptic ulcer disease, as well as conduct an analysis that allows you to identify the presence of pathogenic bacteria, in particular Helicobacter Pylori.
The use of radiographic method is advisable if there are dystrophic changes in the bulb of the duodenum, reducing its patency and the ability to visually examine it from the inside. Radiography can also provide useful information if there are various neoplasms in the gastrointestinal tract. Often, in parallel with the radiographic examination, ultrasound of the abdominal organs is prescribed.
Additional, quite informative methods that allow assessing the dysfunction of the gastrointestinal tract organs are considered to be electrogastrography, phono- and balloonography. Using these methods, the doctor monitors changes in the motor function of the intestine and other organs involved in the digestion process.
This comprehensive approach allows for a highly accurate diagnosis, without making mistakes or confusion in the need to distinguish between an ulcer of the duodenal bulb and other pathologies of the initial section of the small intestine.
What do need to examine?
Who to contact?
Treatment duodenal ulcers.
Treatment of a duodenal ulcer is a long and multi-stage process. It includes drug therapy, folk remedies, physical therapy, and diet. All these methods are not used simultaneously; their purpose depends on the stage of development of the pathology.
Since the ulcer of the duodenal bulb can be caused by many reasons of different nature, the approaches to treatment in this regard should be different. After all, first you need to identify and remove the pathogenic factor, and then fight its consequences. Drug therapy for ulcers of the duodenal bulb is used for this purpose.
The formation of ulcers on the mucous membrane of the duodenum occurs against the background of increased acidity, which means that it is necessary to fight it first. Drugs called antacids help to reduce the acidity of gastric juice and slightly reduce the production of hydrochloric acid and pepsin.
There are currently many medications that belong to the antacid group. But the most popular of them are considered to be "Omez" or its analogue "Omeprazole". The drugs "Gastrozol", "Zerocid", "Omitox", "Peptikum", "Ultop" and some others are also analogues of the above medications, since they are based on the same active substance - omeprazole.
The same proton pump inhibitors (H + -K + -AFTase), but with a different active ingredient - esomeprazole, are also used to treat ulcerative lesions of the duodenum. These are the drugs "Nexium", "Neo-Zext", "Esomeprazole".
Budget drugs such as Ranitidine and Famotidine have also proven themselves to be effective in inhibiting the secretion of hydrochloric acid. And the drugs Almagel and De-Nol will prove indispensable at the acute stage of the process to protect the mucous membrane from the aggressive effects of hydrochloric acid.
If the cause of increased acidity and the development of the ulcer process was a stressful situation, and its effect has not been stopped to this day, it makes sense to prescribe sedatives that normalize the mental state and sleep, and prevent the subsequent negative impact of nervous tension on the work of the gastrointestinal tract. In order not to injure the stomach and intestines once again, such drugs should be selected from a series of herbal remedies (motherwort tincture, "Barboval", soothing herbal teas). Doctors rarely resort to more serious drugs such as antidepressants or neuroleptics in connection with diseases of the duodenum.
Pathogenic bacteria, especially Helicobacter Pylori, are also a very common cause of gastritis, stomach ulcers and duodenal ulcers. And, as is known, the fight against bacterial infection without antibiotics is simply unthinkable. A good effect in the treatment of duodenal ulcers caused by Helicobacter Pylori is achieved by taking two drugs together: Clathrimycin and Amoxicillin. Sometimes, in addition to them or as the main drug, antimicrobial agents such as Metronidazole, Erythromycin, Ampiox, etc. can be prescribed.
Antibiotic therapy is carried out as part of a complex therapy, including mandatory intake of antisecretory drugs (antacids). Moreover, antacids are indicated for patients with ulcerative lesions of the stomach and duodenum throughout their life in certain courses or one-time to relieve heartburn and other symptoms of increased acidity.
To improve the nutrition of the intestinal mucosa and activate regenerative processes, Solcoseryl, Actovegin, vitamins and vitamin-mineral complexes containing vitamin A can be prescribed.
Taking antacids usually relieves pain, but if this is not enough, you can try taking antispasmodics such as No-shpa, Spazgan, etc.
You can combat nausea and vomiting with Metoclopramide, Motilium, Cerucal and similar drugs.
As for physiotherapy, it is applicable at the stage of remission or abating exacerbation. Effective procedures: mud therapy, mineral and pine baths with a temperature close to body temperature, novocaine electrophoresis, UHF procedures.
More about medicines
"Omeprazole" is a cheaper but no less effective analogue of the popular "Omez". It is used to treat the acute phase of the ulcerative process in the duodenum, as well as an anti-relapse agent. It is produced in capsule form, which allows it to begin to act exactly where its action (neutralization of acid) is needed.
If the exacerbation of the ulcer of the duodenal bulb was caused by stress or the negative influence of drugs, Omeprazole is taken in a dosage of 1 capsule (20 mg) per day for a course of 2 to 4 weeks.
If the development of peptic ulcer disease was not without the influence of Helicobacter Pylori, then Omeprazole is taken as part of complex therapy together with antibiotics (double and triple therapy).
With dual therapy using Omeprazole and 1 antibiotic, the course of treatment is 2 weeks. Treatment regimens:
- "Omeprazole" - 1-2 capsules plus "Amoxicillin" - 750 mg = 2 times a day.
- "Omeprazole" - 2 capsules (1 time per day) plus "Clarithromycin" - 500 mg (3 times per day).
- "Omeprazole" - 2 capsules (1 time per day) plus "Amoxicillin" - from 750 to 1500 mg (2 times per day).
With triple therapy (Omeprazole plus 2 antibiotics), the course of treatment is reduced to 1 week. Treatment regimens:
- "Omeprazole" - 1 capsule plus "Amoxicillin" - 1000 mg plus "Clathrimycin" 500 mg = 2 times a day.
- "Omeprazole" - 1 capsule plus "Clarithromycin" - 250 mg plus "Metronidazole" - 400 mg = 2 times a day.
- "Omeprazole" - 2 capsules (1 time per day) plus "Amoxicillin" - 500 mg (3 times per day) plus "Metronidazole" - 400 mg (3 times per day).
"Omeprazole" is an effective drug that significantly reduces the acidity of gastric juice, but its use can cause some undesirable symptoms. Side effects of the drug in relation to the gastrointestinal tract include: bowel disorders in the form of diarrhea or constipation, the appearance of pain in the stomach, dyspeptic phenomena, taste disturbances, hepatitis. Other side effects: headaches, myasthenia, arthralgia, changes in blood composition, skin rashes accompanied by itching, allergic reactions, deterioration of vision, hyperhidrosis, swelling of the hands and feet, etc.
But there are very few contraindications to the use of the drug. These are periods of pregnancy and breastfeeding, as well as hypersensitivity to the drug. The drug is not used in pediatric practice. But adult patients with liver pathologies should be careful when using Omeprazole, for them the maximum dose is 2 capsules per day.
"Nexium" is another effective proton pump inhibitor that neutralizes hydrochloric acid in the gastric juice. For the treatment of ulcerative lesions of the duodenum, the drug is most often used in the form of tablets or granules for the preparation of a suspension taken orally (for children and those who have difficulty swallowing tablets).
The method of administration and dosage of the drug depend on the form of release. Thus, tablets are swallowed whole, without crushing, and granules are diluted in plain water at the rate of 1 packet per 15 ml of water. The dosage depends on the indications for use.
For the treatment and prevention of duodenal ulcers while taking NSAIDs, take 20 to 40 mg of the drug once a day. The therapeutic course can be from 4 to 8 weeks.
If the ulcer is caused by Helicobacter Pylori, then the treatment with the drug is carried out in combination with antibiotics. The scheme for treatment and prevention is one: "Nexium" - 20 mg plus "Amoxicillin" - 1000 mg plus "Clarithromycin" - 500 mg = 2 times a day for a course of 1 week.
The drug's side effects are similar to those of Omeprazole. And it does not have many more contraindications: childhood, fructose intolerance and hypersensitivity to any of the drug's components, parallel use of Atazanavir and Nelfinavir. Caution should be exercised during pregnancy, lactation, and renal failure.
"Famotidine" is an antiulcer drug available to almost all patients. It is available in tablets of 20 and 40 mg.
For the treatment of peptic ulcer disease in the acute stage, 40 mg per day is prescribed for 1-2 months; to prevent relapses, 20 mg is prescribed at night.
In addition to the side effects typical for the above-described drugs, in the case of Famotidine we can add decreased sexual desire, amenorrhea, disorders in the hematopoietic system, abnormal heart rhythms, decreased blood pressure, etc.
Contraindications are also not particularly diverse: periods of pregnancy and lactation, sensitivity to the components of the drug and age under 3 years.
Folk remedies
Folk treatment of the ulcer of the duodenal bulb is effective if the disease is not associated with the activity of Helicobacter Pylori. But again, to achieve quick and lasting results, the use of folk medicine recipes should be agreed with a doctor and take place in combination with drug therapy.
Here are some useful recipes that help relieve the unpleasant symptoms of the disease:
- Fresh potato juice does not require special advertising, since it is applicable everywhere where it is necessary to reduce acidity and protect the mucous membrane of the gastrointestinal tract. It should be drunk for 3 weeks, a quarter of a glass before main meals (15-20 minutes).
- An effective and tasty remedy that helps the ulcer to heal within 3 weeks can be made from butter and natural honey. Mix butter and honey in equal quantities and boil until brown. Store in a cool place. Take the composition in the morning on an empty stomach before meals in a dosage of 10 g.
- If there is no good oil, then honey itself is basically capable of treating ulcers. To do this, mix 35 g of honey in a glass of water and drink. You can eat no earlier than an hour and a half later. The treatment continues for a month.
- Sea buckthorn seed oil is irreplaceable for any ulcerative processes in the gastrointestinal tract. It should be taken 1 teaspoon before each meal.
Herbal treatment of ulcerative lesions of the duodenum is especially effective if the herbs are used in special medicinal mixtures, which can be found in pharmacies. Although some herbs can bring noticeable relief to ulcer patients on their own. These include: calendula, blue cyanosis, mint. Also useful: fennel, chamomile, cinquefoil, horsetail, yarrow, etc.
 [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
[ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ]
Homeopathy
To reduce pain, especially "hunger" pains in duodenal ulcers, the most effective homeopathic remedy is Anacardium. The drug is also useful for constipation.
In this regard, women are well helped by the homeopathic preparation Cimicifuga, which relieves the symptoms of constant hunger and pain that intensifies during the premenstrual period.
For very severe pain that forces a person to bend forward, the drug Colocynthis taken in high potencies will be effective. And the drugs Acidum sulfuricum, Conium, Natrium sul-furicum and Capsicum help to get rid of painful heartburn, which is an indicator of an increase in the level of hydrochloric acid in the stomach.
Calcium fluoricum will help prevent the appearance of adhesions, coarse scars and intestinal stenosis in severe cases of duodenal ulcers.
All homeopathic preparations in doses prescribed by a doctor are safe for the health of patients. Having no serious contraindications and minor side effects in the form of allergic rashes, they are a good alternative to synthetic drugs.
Surgical treatment is considered appropriate only in severe cases of duodenal ulcer, when there are possible complications, such as gastrointestinal bleeding, ulcer perforation, cicatricial changes in the bulb or stenosis of the duodenum, creating intestinal obstruction.
Diet for duodenal ulcer
It is simply impossible to effectively combat gastrointestinal diseases without following a special diet that facilitates the work of the stomach and intestines, prevents the aggressive effect of certain foods on the mucous membrane and prevents increased acidity of gastric juice.
With a duodenal ulcer, it is not necessary to adhere to a strict diet all the time, but during periods of exacerbation, some restrictions and rules will help to significantly alleviate the patient's condition and make treatment more effective:
- Fractional nutrition is the basis of any diet for gastrointestinal diseases. It is necessary to eat every 3 hours, reducing the usual portions, so that the patient gets up from the table a little hungry.
- Slow and thorough chewing of food and consumption of strictly pureed foods are simply necessary during periods of exacerbation of the disease.
- Food should be warm, which will prevent the irritating effect of high or low temperatures on the gastric mucosa, helping it to work and not causing increased production of hydrochloric acid and pepsin.
- Some restrictions in the choice of food products are related to their ability to increase the acidity of gastric juice and irritate the mucous membrane of the stomach and intestines, because during illness, chemical or mechanical irritation can cause an exacerbation of the disease and the formation of new ulcers.
Rich broths from meat, fish or vegetables, bakery products, fresh vegetables, fatty meat, smoked and fried dishes, mushrooms, canned food, sorrel, tomatoes - you will have to give up all these products and dishes made from them (for a while or even forever).
A diet for duodenal ulcers also involves limiting the amount of salt consumed to a maximum of 15 g. But milk, fruits, mashed cereals, steamed vegetables and meat, eggs (up to 3 per day), and diluted juices will only be beneficial, because they will saturate the body with the vitamins and nutrients it needs.
Drugs
Prevention
Prevention of duodenal ulcer consists of eliminating factors from life that provoke the development of pathology. In order for this dangerous disease to never bother you, you need to adjust some things in your life:
- Give up bad habits (smoking and drinking alcohol), or reduce such manifestations to a minimum.
- Forget about all kinds of “dry” snacks, fast food, giving preference to wholesome nutrition.
- Do not get carried away with medications, especially from the NSAID group, take them under the supervision of a doctor in combination with drugs that protect the gastrointestinal mucosa from the negative effects of irritants.
A calm attitude towards life, the ability to cope with stress, proper and nutritious nutrition against the background of a healthy lifestyle are the best protection against ulcerative diseases of any etiology.
Ps If you undergo a full course of treatment for duodenal ulcer disease without evasion and continue to follow a gentle diet, the duodenal bulb ulcer will not make itself known for a long time. And it is quite possible that you can forget about it forever.
Forecast
A duodenal ulcer is not a tension headache that can be cured with one pill. It requires long-term treatment, dietary regimen, and a special diet.
The prognosis of peptic ulcer disease and the need (or lack thereof) for surgical intervention depend on how timely the patient sought help, how effective and correct the treatment was, and whether all additional dietary requirements were met.

