Medical expert of the article
New publications
Trophoblastic disease
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Trophoblastic (gestational) disease is a general term for a spectrum of pregnancy-related proliferative anomalies derived from the trophoblast. An important feature of trophoblastic disease is the formation of ovarian luteal cysts, which is observed in 50% of cases. Most patients have bilateral luteal cysts, which can reach large sizes and fill the entire abdominal cavity.
Epidemiology
The incidence of trophoblastic disease has a certain geographical pattern - varying from 0.36% in Asian to 0.008% in European countries (in relation to the number of pregnancies). Such epidemiology is associated with a violation of the immune status of women with a large number of pregnancies and a short interval between them. However, an exact explanation for this fact has not yet been found.
Symptoms trophoblastic disease
The leading symptom of trophoblastic disease is that after amenorrhea, uterine bleeding occurs, sometimes accompanied by the release of multiple bubbles with transparent contents.
Other symptoms of trophoblastic disease:
- severe early gestosis (nausea, vomiting), preeclampsia;
- the size of the uterus exceeds the expected gestational age;
- during vaginal examination - the uterus is of a hard elastic consistency, longer than the expected pregnancy period;
- palpation of the uterus (if large - no signs of the fetus);
- absence of fetal heartbeat and movement;
- absence of signs of a fetus in the uterine cavity (according to ultrasound data);
- qualitative and quantitative detection of human chorionic gonadotropin in urine and blood (in case of hydatidiform mole, the level of human chorionic gonadotropin exceeds its level in normal pregnancy by 50-100 times).
- pain in the lower abdomen with the development of choriocarcinoma;
- symptoms caused by the predominant localization of tumor metastases (hemoptysis, neurological symptoms, etc.).
Stages
Clinical classification of choriocarcinoma (FIGO, 1992):
- Stage I - the lesion is limited to the uterus, there are no metastases.
- Stage II - the lesion extends beyond the uterus, but is still limited to the genitals.
- Stage III - metastasis to the lungs.
- Stage IV - metastatic lesions of other organs.
Forms
Trophoblastic disease includes:
- hydatidiform mole,
- invasive (malignant) mole,
- choriocarcinoma,
- trophoblastic tumor of the placental site.
 [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
[ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
Hydatidiform mole
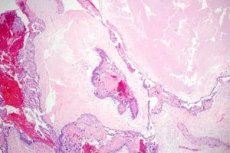
Hydatidiform mole is characterized by edema and enlargement of the placental villi with hyperplasia of both layers of the trophoblast. It has two varieties - complete and partial; the latter is distinguished by the presence of the fetus or its parts along with intact villi.
Invasive mole is a hydatidiform mole with myometrial invasion, trophoblast hyperplasia and preservation of the placental villus structure.
In case of hydatidiform mole, luteal cysts may appear during the first 2 weeks. Their presence serves as an unfavorable prognostic sign. The regression of luteal cysts is observed within 3 months after removal of the hydatidiform mole.
Placental site trophoblastic tumor
Placental trophoblastic tumor arises from the trophoblast of the placental bed and consists mainly of cytotrophoblast cells; it can be of low or high malignancy grade.
 [ 16 ]
[ 16 ]
Chorionic carcinoma
Pregnancy-associated choriocarcinoma arises from the cyto- and syncytiotrophoblast, i.e. from both layers of the trophoblast, is most often localized in the uterus, and can occur both during and after the completion of a normal or pathological pregnancy (abortion, miscarriage, childbirth, hydatidiform mole, ectopic pregnancy). In the case of an ectopic pregnancy, it is localized in the tube or ovary, which is extremely rare. Ovarian choriocarcinoma can develop from germ cells, it is not associated with pregnancy and is classified as a germ cell tumor (i.e., it is not trophoblastic).
Macroscopically, choriocarcinoma may be a nodular tumor located on the inner surface of the uterine cavity, intermuscularly, under the serous cover, or in the form of diffuse growths. The tumor is dark purple in color, has a soft consistency, does not contain vessels, and is from 0.5 to 12 centimeters or more in size. In most cases, it is located submucosally.
Microscopically, choriocarcinoma has 3 histotypes: syncytial, cytotrophoblastic and mixed. Characteristic features include invasion of the chorionic epithelium, extensive areas of necrosis and hemorrhage, and isolated clusters of Langhans cells.
Diagnostics trophoblastic disease
Diagnosis of trophoblastic disease is based on the following data:
- anamnesis;
- clinical examination;
- radiation, histological and hormonal research methods.
Clinically important: detailed anamnesis, gynecological examination with detection of cyanosis of the mucous membranes of the vagina and cervix, enlargement and soreness of the uterus, possible metastases.
Radiological diagnostics includes ultrasound, Doppler ultrasonography, angiography, magnetic resonance imaging (MRI) and computed tomography (CT).
Ultrasound and Dopplerography are informative, simple, reliable and can be used to diagnose hydatidiform and invasive mole and choriocarcinoma, as well as metastases to the liver, kidneys, and ovaries. Being noninvasive and harmless, they are indispensable for monitoring the effectiveness of chemotherapy. Contrast angiography allows for a more precise diagnosis of choriocarcinoma, especially with negative histological data from endometrial scraping and trophoblastic hormones.
How to examine?
Who to contact?
Treatment trophoblastic disease
Trophoblastic disease is one of the rare forms of malignant diseases, characterized by a high rate of cure with chemotherapy even in the presence of distant metastases.
The main method of treating trophoblastic disease is chemotherapy, which is used both independently and in complex therapy. In the complex treatment of certain forms of trophoblastic disease, surgical and radiation therapy are used.
Principles of treatment of hydatidiform mole
- Vacuum aspiration or removal of a hydatidiform mole by curettage of the uterus with the administration of uterine contraction agents (intravenous oxytocin, etc.).
- Hysterectomy for large hydatidiform moles, significant bleeding, lack of conditions for emptying the uterus; the woman's unwillingness to have further pregnancies. Ovaries with theco-luteal cysts are not removed.
- After removal of the mole, observation is carried out for two years (monitoring the content of human chorionic gonadotropin in the urine once a month).
- Preventive chemotherapy (methotrexate) after evacuation of the hydatidiform mole using vacuum aspiration is performed in the following cases: age over 40 years, discrepancy between the size of the uterus and the expected pregnancy period, presence of luteal cysts during the period of hydatidiform mole, elevated levels of human chorionic gonadotropin over 20,000 IU/ml after 2-3 evacuations or after surgical treatment of invasive mole, lack of dynamic monitoring of human chorionic gonadotropin levels.
Principles of treatment of choriocarcinoma
- First-line chemotherapy (methotrexate, actinomycin D, chlorambucil, 6-mercaptopurine, adriamycin, platinum drugs and alkaloids).
- Surgical treatment. Indications: profuse uterine bleeding, tumor tendency to perforation, large uterus, tumor resistance to chemotherapy. Volume of surgery: in young women with a tumor without metastases - extirpation of the uterus without appendages, after 40 years - extirpation of the uterus with appendages.
- Discharge is made after 3 negative tests for human chorionic gonadotropin, carried out at intervals of 1 week.
- Observation. Human chorionic gonadotropin titer determination (once every 2 weeks) for 3 months, then once every 6 months for 2 years. Chest X-ray once every 3 months (for a year). Contraception (COC) is recommended for a year.
The choice of treatment regimen is currently carried out taking into account the degree of risk of developing tumor resistance to chemotherapy according to the WHO scale.
According to the WHO scale, there are 3 degrees of risk of resistance development: low (sum of points less than 5), moderate (5-7 points) and high (8 points or more).
In case of low risk of tumor resistance to chemotherapy (absence of metastases, small, up to 3 cm, size of uterine tumor, low level of hCG in blood serum and disease duration less than 4 months), first-line monochemotherapy with methotrexate or dactinomycin is performed. The effectiveness of monochemotherapy ranges from 68.7 to 100%.
The earliest sign of tumor resistance to chemotherapy is the absence of a decrease or an increase in serum hCG in two repeated tests at an interval of 1 week.
WHO scale for determining choriocarcinoma resistance to chemotherapy
Risk factor |
Number of points |
|||
0 |
1 |
2 |
3 |
|
Age, years |
Up to 39 |
Over 39 |
||
Outcome of previous pregnancy |
Hydatidiform mole |
Abortion |
Childbirth |
|
Interval*, month |
Less than 4 |
4-6 |
7-12 |
More than 12 |
HCG level, IU/L |
Less than 10** |
10 3 -01 4 |
10 4 -10 5 |
More than 10 5 |
Blood group |
0 or A |
B or A B |
||
Largest tumor, including uterine tumor |
Less than 3 cm |
3-5 cm |
More than 5 cm |
|
Localization of metastases |
Spleen, kidney |
Gastrointestinal tract, liver |
Brain |
|
Number of metastases |
1-3 |
4-8 |
More than 8 |
|
Previous chemotherapy |
1 drug |
2 cytostatics or more |
||
- * The interval between the end of the previous pregnancy and the start of chemotherapy.
- ** Low levels of human chorionic gonadotropin may occur with trophoblastic tumors at the site of the placenta.
For the treatment of patients with resistant forms of tumors, various chemotherapy regimens (2nd line) are used with an increase in the dose of administered drugs and the frequency of courses.
In case of moderate and high risk of tumor resistance development (presence of metastases, tumor size more than 3 cm, high level of human chorionic gonadotropin, duration of symptoms more than 4 months, onset of the disease immediately after childbirth), combination polychemotherapy is used according to various regimens: MAC (methotrexate, dactinomycin, chlorambucin); EMA-CO (etoposide, dactinomycin, methotrexate, vincristine, cyclophosphamide, leucovorin), SNAMOSA (hydroxyurea, dactinomycin, methotrexate, leucovorin, vincristine, cyclophosphamide, doxorubicin); PVB (cisplatin, vinblastine, bleomycin), EHMMAC (etoposide, hydroxyurea, dactinomycin, methotrexate, vincristine). The most effective and less toxic combination of second-line drugs is the EMA-CO regimen.
For the treatment of resistant tumor foci, a combination of their surgical removal and second-line chemotherapy is of great importance. In case of distant metastases to the brain, combined polychemotherapy is performed in combination with radiation therapy to the entire brain; radiation therapy is possible in case of metastasis to the parametrium.
Thus, surgery and radiation therapy are additional treatment methods.
Drugs
Prevention
The follow-up of patients after a hydatidiform mole is carried out for 4 years. It is aimed at early diagnosis of possible choriocarcinoma and includes the following: monitoring of the menstrual cycle, contraception for 2 years, general examination and gynecological examination, determination of the level of hCG in the blood serum once every 2 weeks until the indicators are normalized and then every 6 weeks in the first six months, then every 8 weeks in the following 6 months.
Once every 4 months - in the second year and once a year during the third and fourth years; ultrasound of the pelvic organs and chest X-ray 2 weeks after evacuation of the hydatidiform mole and then once a year during the first two years. The following observation periods are recommended for patients who received preventive chemotherapy after a hydatidiform mole: the first 3 months - once every 2 weeks, then monthly for 3 months, then according to the specified scheme.
The follow-up of patients with choriocarcinoma is carried out for 5 years and also includes a menogram, contraception for 2 years, a general examination with examination of the mammary glands, a gynecological examination, determination of the level of hCG in the blood serum monthly in the first year, once every 3 months in the 2nd year, once every 4 months in the third year and twice a year in the fourth and fifth years, then once a year. Ultrasound of the pelvic organs and radiography or CT of the lungs once every 2 months in the first year and then once a year during follow-up.

