Medical expert of the article
New publications
Premature detachment of the normally located placenta
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epidemiology
The incidence of abruptio placentae is estimated to range from 0.6–1% of pregnancies in the United States,[ 3 ] but the reported incidence is lower (0.4–0.5%) in Northern European countries 5 and higher (3.5–3.8%) in some South Asian countries.[ 4 ]
Maternal mortality in this pathology is 1.6–15.6%, perinatal mortality is 20–35.0‰. [ 5 ], [ 6 ] The risk of cesarean section ranged from 2.4 to 61.8 (incidence range: 33.3–91%) and was the most frequently reported birth outcome associated with abruption. [ 7 ]
Symptoms premature detachment of the normally located placenta
Typically, premature separation of a normally situated placenta presents with maternal symptoms of vaginal bleeding, abdominal pain and contractions, and/or abnormal fetal heart rate.[ 8 ],[ 9 ] The condition is also characterized by chronic placental dysfunction and separation from the uterine wall, which, as it progresses, can lead to a corresponding decrease in the placental surface area available for oxygen exchange and nutrient supply to the fetus.[ 10 ] This process can lead to an increased risk of low birth weight, preterm delivery, and perinatal mortality. Severe cases of abruption can rapidly progress to significant maternal blood loss, fetal hypoxia, and fetal death, which may lead to the need for emergency cesarean section.[ 11 ]
Forms
There is no single classification of premature detachment of a normally located placenta.
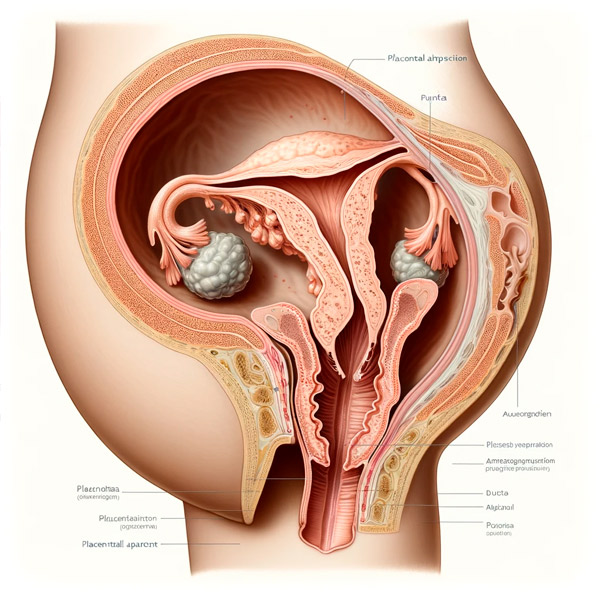
In case of detachment of a normally located placenta, a distinction is made between:
- detachment with external or visible bleeding - bleeding from the vagina;
- detachment with internal or hidden bleeding - blood accumulates between the placenta and the uterine wall, forming a retroplacental hematoma;
- detachment with combined or mixed bleeding - there is both hidden and visible bleeding. According to the area of detachment, there are:
- partial (progressive or non-progressive);
- complete.
According to the severity of the clinical picture, detachment is divided into:
- mild (detachment of a small area of the placenta);
- medium (detachment of 1/4 of the placental surface);
- severe (detachment of more than 2/3 of the placental surface).
Diagnostics premature detachment of the normally located placenta
Pregnant women are often diagnosed with long-term sluggish gestosis, hypertension, kidney disease, and acute infectious diseases. Less often, premature detachment occurs after external obstetric version of the fetus, amniocentesis, abdominal trauma of various etiologies, and rapid changes in uterine volume due to the rupture of amniotic fluid in polyhydramnios. [ 12 ]
- In case of premature detachment of a normally located placenta of a mild degree during pregnancy, the condition of the pregnant woman is satisfactory. The visible mucous membranes and skin are of normal color or slightly pale, the pulse is rapid, but of satisfactory filling, there is slight pain in the uterus, there are often no signs of external bleeding, sometimes there is scanty blood discharge from the genital tract. The condition of the fetus is satisfactory. During pregnancy, the diagnosis can be made using ultrasound (detection of a retroplacental hematoma if blood is not released). The final diagnosis is established after childbirth, when a crater-shaped depression and a blood clot are determined on the maternal surface of the placenta.
- In case of premature detachment of a normally located placenta of moderate degree during pregnancy, the condition of the pregnant woman is moderate. Symptoms of hemorrhagic shock appear: visible mucous membranes and skin become sharply pale, the skin is cold to the touch, moist. The pulse is frequent, weak filling and tension, arterial pressure is low, breathing is rapid. The uterus is tense, of a dense consistency, asymmetrical in shape due to a retroplacental hematoma and is sharply painful upon palpation in a certain area. Often, a local bulge and tension are determined over the place of placental abruption when it is localized on the anterior wall of the uterus. Due to the painfulness of the uterus, it is impossible to palpate small parts of the fetus. Fetal motor activity is expressed or weakened, tachycardia or bradycardia is noted in the fetus upon auscultation. Its death is possible as a result of acute hypoxia. Bloody discharge (bright or dark) from the genital tract is determined.
- In case of severe premature abruption, the onset of the disease is sudden. There are sharp abdominal pains, severe weakness, dizziness, and often fainting. The skin and visible mucous membranes are pale, the face is covered in cold sweat. The pulse is rapid, weak in volume and tension. Arterial pressure is low. The abdomen is sharply distended, the uterus is tense, painful to palpation, with local swelling, small parts of the fetus and heartbeat are not determined due to the pronounced tone and soreness of the uterus. External bleeding from the genital tract is absent or moderate, it is always secondary and less abundant than internal bleeding. The type of placental abruption is of great importance for diagnosis.
- In case of marginal placental abruption, external bleeding is observed, usually not accompanied by pain syndrome. In case of central placental abruption and hematoma formation, external bleeding is absent even with severe pain syndrome. This is an extremely dangerous form, leading to fetal death, severe hypovolemic disorders in the mother. The classic picture of premature detachment of a normally located placenta is observed in only 10% of women. In 1/3 of pregnant women, pain syndrome is absent as one of the important diagnostic signs of this pathology. The leading clinical symptoms of detachment are bloody discharge from the genital tract and signs of intrauterine hypoxia of the fetus.
Special research methods
Assessing the severity of blood loss.
- Biochemical blood test (protein less than 60 g/l).
- Hemostasis: [ 13 ]
- hypercoagulation phase - increased amounts of thromboplastin and prothrombin, clotting time less than 4 minutes, paracoagulation tests (ethanol, b-naphthol, protamine sulfate) are unchanged;
- transitional phase - fibrinogen level less than 2 g/l, paracoagulation tests are positive, the amount of fibrin degradation products is increased, thrombin time is more than 30–35 s, prothrombin time is more than 20 s, the amount of antithrombin III is less than 75%;
- hypocoagulation phase: fibrinogen level less than 1.5 g/l, paracoagulation tests are often negative, fibrin degradation product level more than 2×10 -2 g/l, thrombin time more than 35 s, prothrombin time more than 22 s, antithrombin III level 30–60%, platelet count decreased.
- Ultrasound (determines the location of placental abruption, the size of the retroplacental hematoma, its structure). In case of marginal placental abruption with external bleeding, it is not always detected.
- CTG.
- Doppler.
Indications for consultation with other specialists
- Anesthesiologist: need for abdominal delivery.
- Neonatologist-resuscitator: the need for resuscitation measures at the birth of a child in a state of moderate or severe asphyxia.
What do need to examine?
How to examine?
Differential diagnosis
Differential diagnosis should be made with the following conditions.
- Bleeding with placenta previa is rarely combined with vascular pathology ( gestosis, hypertension ), pyelonephritis. Hemorrhagic shock is not typical. Repeated bleeding without pain symptoms is typical. The uterus is painless on palpation, normal in shape and size. The fetus is often in the breech, oblique, transverse position. The presenting part is located high above the entrance to the small pelvis. The fetus suffers slightly.
- Bleeding from a ruptured marginal sinus of the placenta occurs suddenly at the end of pregnancy or the first stage of labor. It usually stops within 10 minutes. The blood that flows out is scarlet. Repeated bleeding may occur. Pregnant women with this pathology often have gestosis and multiple pregnancies. The prognosis for the fetus is favorable. The final diagnosis is established after childbirth, when a damaged sinus and blood clots fixed to the edge of the placenta are determined.
- Rupture of the umbilical cord vessels with pleural attachment. Bleeding (of fetal origin) develops suddenly with spontaneous or artificial rupture of the amniotic sac, moderate, scarlet in color, quickly leads to the death of the fetus. A dead fetus is pale white (anemia). This pathology should be assumed if the fetal heartbeat begins to suffer immediately after the rupture of the membranes and the onset of bleeding. The final diagnosis is established after examining the placenta: damaged umbilical cord vessels are attached to the membranes or to an additional lobe of the placenta.
- Uterine rupture during pregnancy (along the scar). The uterus after the rupture decreases in volume, the fetus is dead, palpated under the abdominal wall. The pregnant woman is in a state of shock (skin is pale, pulse is threadlike, blood pressure is sharply reduced). Emergency laparotomy and, as a rule, removal of the uterus are indicated.
- Bleeding from ruptured varicose veins of the vagina, ectopia, polyps, and cervical carcinoma can be excluded by examining the vagina and cervix using heated mirrors.
Who to contact?
Treatment premature detachment of the normally located placenta
The goal of treatment is to stop bleeding.
Indications for hospitalization
Bleeding from the genital tract of any intensity.
Non-drug treatment
Bed rest.
Drug therapy
The choice of treatment method for premature placental abruption is determined by the severity of bleeding and the condition of the mother and fetus. [ 14 ]
In case of placental abruption during pregnancy (up to 34–35 weeks), if the condition of the pregnant woman and the fetus does not suffer significantly, there is no pronounced external or internal bleeding, a wait-and-see approach is possible.
Therapy is aimed at treating the disease that caused the detachment (hypertension, gestosis, etc.), reducing uterine tone, correcting hemostasis, and combating anemia and shock.
Treatment is carried out under the control of ultrasound, Doppler, CTG; it includes bed rest, administration of antispasmodics, antiplatelet agents, multivitamins, antianemic agents:
- drotaverine 2% solution 2–4 ml intramuscularly, intravenously;
- etamzilate intravenously, intramuscularly 2–4 ml, then every 4–6 hours 2 ml. In case of placental abruption, β-adrenergic agonists should not be used.
Basic principles of treatment of hemorrhagic shock.
- Stopping bleeding.
- Maintenance of macro- and microcirculation (controlled hemodilution).
- Correction of concomitant metabolic acidosis (4% sodium bicarbonate solution at a rate of 2 ml/kg body weight).
- Administration of glucocorticoids (0.7–0.5 g hydrocortisone or equivalent doses of prednisolone or dexamethasone).
- Maintaining adequate diuresis at a level of 50–60 ml/h with small doses of furosemide (10–20 mg) after the administration of each liter of fluid.
- Transfer of patients to artificial ventilation in case of increasing hypercapnia (increase in PCO2 to 60 mm Hg), presence of symptoms of respiratory failure.
- Use of antibiotics starting with cephalosporin drugs.
- Adequate pain relief.
Surgical treatment
In moderate and severe forms of premature detachment of a normally located placenta during pregnancy, emergency cesarean section is indicated in the interests of the pregnant woman, regardless of whether the fetus is alive. In the presence of multiple hemorrhages in the uterine wall (Kuveler's uterus), extirpation of the uterus without appendages is indicated due to the risk of bleeding in the postoperative period against the background of coagulopathy and uterine hypotension.
Patient education
A pregnant woman must be informed about immediate hospitalization if even minor bleeding from the genital tract occurs.
Further management
On the 2nd-3rd day, infusion therapy and correction of electrolyte balance are continued, a cleansing enema is given, and breathing exercises are performed. On the 5th-6th day, an ultrasound is performed to assess the size of the uterus, its cavity, the condition of the sutures, and the presence of hematomas. On the 6th-7th day, the sutures are removed from the anterior abdominal wall.
Prevention
Timely diagnosis and treatment of pregnant women with diseases leading to placental abruption (arterial hypertension, gestosis, etc.), reduction of uterine tone, correction of hemostasis.
Forecast
The prognosis for the life of the mother and fetus is ambiguous. The outcome of the disease depends on the etiological factor, the severity of the detachment, the timeliness of the diagnosis, the nature of the bleeding (external, internal), the choice of an adequate treatment method, the state of the pregnant woman's body, and the degree of maturity of the fetus.
Sources
- Ananth CV, VanderWeele TJ. Placental abruption and perinatal mortality with preterm delivery as a mediator: disentangling direct and indirect effects. Am J Epidemiol. 2011;174(1):99–108.
- Boisramé T, Sananès N, Fritz G, et al. Placental abruption: risk factors, management and maternal-fetal prognosis. Cohort study over 10 years. Eur J Obstet Gynecol Reprod Biol. 2014;179:100–104.
- Dars S, Sultana F, Akhter N. Abruptio placentae: Risk factors and maternal outcomes at a tertiary care hospital. J Liaquat Univ Med Health Sci. 2013;12:198–202.
- Tikkanen M. Placental abruption: epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand. 2011; 90(2):140–149.
- Hossain N, Khan N, Sultana SS, Khan N. Abruptio placenta and adverse pregnancy outcome. J Pak Med Assoc. 2010;60(6):443–446.
- Pitaphrom A, Sukcharoen N. Pregnancy outcomes in placental abruption. J Med Assoc Thai. 2006;89(10):1572–1578.
- Tikkanen M, Nuutila M, Hiilesmaa V, Paavonen J, Ylikorkala O. Clinical presentation and risk factors of placental abruption. Acta Obstet Gynecol Scand. 2006;85(6):700–705.
- Savelyeva, G. M. Gynecology: national guide / ed. G. M. Savelyeva, G. T. Sukhikh, V. N. Serov, V. E. Radzinsky, I. B. Manukhin. - 2nd ed., revised. and additional - Moscow: GEOTAR-Media, 2022.
- Obstetrics: national guide / ed. G. M. Savelyeva, G. T. Sukhikh, V. N. Serov, V. E. Radzinsky. - 2nd ed., revised. and additional - Moscow: GEOTAR-Media, 2022.

