Medical expert of the article
New publications
Thoracoscopy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Thoracoscopy is a procedure used by a doctor to examine the space inside the chest (outside the lungs). Thoracoscopy is prescribed for strictly specific indications, in particular for the treatment of spontaneous pneumothorax. The procedure is effective both in diagnostic and therapeutic terms. It is minimally traumatic and is very rarely accompanied by intraoperative or postoperative complications.
The main "plus" of thoracoscopy is that there is no need to make large damaging tissue incisions. Thoracoscopy is performed through punctures in the chest wall, using special endoscopy instruments. Today, many thoracic interventions can be performed with the help of thoracoscopy. The procedure is relevant if it is necessary to diagnose or treat pulmonary and cardiovascular pathologies, diseases of mediastinal organs and esophagus, thorax and pleura.
Indications for the procedure
Thoracoscopy is often the operation of choice for many pathological conditions, because it is not characterized by intense postoperative pain, complications are rare, there is no need for the patient to stay in the intensive care unit. Thoracoscopy may be prescribed for the following pathologies:
- Air accumulation in the pleural cavity (Spontaneous pneumothorax );
- Inflammation of the pleura;
- Chest injuries (closed, open);
- Bullous pulmonary emphysema (formation of air cysts in the lungs caused by the destruction of alveoli);
- Generalized form of myasthenia (perform thoracoscopic thymectomy);
- Hyperhidrosis of the palms (perform thorascopic sympathectomy);
- Diffuse lung lesions (granulomatosis, alveolitis );
- Benign and malignant neoplasms in the lungs;
- Breast cancer (perform parasternal lymphadenectomy);
- Tumor processes and esophageal diverticula.
Thoracoscopy with the use of a fiber-optic camera should be mentioned separately. This method has high visualization capabilities. If necessary, during the procedure it is possible to remove fluid accumulated in the pleural cavity or lungs, as well as to take biological material for further histological analysis.
Thoracoscopy, used for diagnostic purposes, in 99.9% of cases allows the correct diagnosis of the disease. However, the intervention is prescribed only when other diagnostic methods cannot be used for any reason, or they do not have sufficient efficiency and informativeness. There are several reasons for this:
- The need for general anesthesia;
- High cost and traumatic as a diagnostic procedure;
- Theoretical, but still a possibility of infection.
Given these nuances, specialists try not to use thoracoscopy for prophylactic purposes: the operation is prescribed only for strict indications, in particular:
- To determine the stage of the cancer; [1]
- To clarify all points in patients with pleurisy of unclear origin, and to take biological material or remove fluid.
Thoracoscopy is appointed if in a particular situation it becomes the only possible or the most informative way to make the correct diagnosis and determine the subsequent treatment tactics.
Spontaneous pneumothorax is a frequent indication for hospitalization of patients with lung diseases requiring emergency medical intervention in special thoracic surgical or surgical clinics. [2]
Thoracoscopy for pneumothorax is appropriate:
- In case of ineffectiveness of transthoracic drainage (lung leakage with progressive or preserved pneumothorax);
- For recurrent spontaneous pneumothorax;
- When pneumothorax develops in patients who have a history of pneumothorax on the other side;
- In the absence of resolution of pneumothorax in individuals with increased somatic risks for thoracotomy.
According to statistics, the most common causes of spontaneous pneumothorax are tumor processes in the lungs, tuberculosis, pulmonary sarcoidosis.
Thoracoscopy in tuberculosis - in particular, in tuberculosis-associated exudative pleurisy or empyema - helps to visually assess the nature of the lesion, perform targeted biopsy of the pleura for morphological verification of pathology, and perform local sanation of the pleural cavity. The surgeon opens individual swollen areas, removes exudate and fibrin, washes the cavity with antiseptic and antitubercular drug solutions, treats the pleura with laser or ultrasound, performs a partial pleuroectomy, drains the pleural cavity.
Preparation
Despite the fact that thoracoscopy refers to minimally invasive interventions, it is still a difficult surgical operation, and it is necessary to prepare for it accordingly. At the preliminary stage, the patient undergoes the necessary tests and electrocardiography.
The patient should tell doctors in advance if he has any chronic pathologies (including heart disease), a tendency to allergies. It is important to warn the doctor if there is a systematic intake of medications (often some drugs that require regular intake are temporarily canceled to avoid the development of complications).
It is especially important to report taking blood-thinning medications.
If the doctor has authorized leaving the morning intake of any medication needed for ongoing treatment, it is best to swallow the tablets without drinking liquid. The use of the smallest possible sip of water is allowed.
Thoracoscopy is performed on an empty stomach: the patient should not eat or drink any food or beverages approximately 12 hours before the operation. That is, if the procedure is scheduled for the first half of the day, only a light dinner is allowed the night before.
You should also avoid drinking (even water) and smoking before the intervention.
It is mandatory to take a shower to cleanse the skin of impurities, which will reduce the chances of getting an infection during the intervention.
If you have removable dentures, they must be removed. The same applies to contact lenses, hearing aids, jewelry, etc.
A basic series of preoperative investigations includes procedures such as:
- General clinical blood tests and urine;
- Determination of blood type and Rh factor;
- Blood biochemistry (determination of glucose, total and direct bilirubin, protein, creatinine, ALT and AST, alkaline phosphatase, etc.);
- Blood tests for RW, HIV, hepatitis B and C;
- Coagulogram;
- Electrocardiogram with transcripts;
- X-rays (Fluorography ).
All of these tests are mandatory before thoracoscopy. Other procedures may also be prescribed on an individual basis, according to the indications. Sometimes there is a need for consultations with physicians of subspecialties.
All necessary laboratory tests should be taken no more than 7-10 days prior to the anticipated thoracoscopy.
Technique of the thoracoscopies
Thoracoscopy is performed using general anesthesia, if necessary, the affected lung is "switched off" from the ventilation process. The patient's position on the operating table is lying on the healthy side.
After anesthesia is administered, the patient falls asleep. The surgeon uses a scalpel to make small incisions (2 cm on average), through which he then introduces a trocar, followed by a thoracoscope and additional instruments through its sleeve. There may be two or three incisions, the exact location of the incisions is chosen depending on the location of the pathologic zone in the thoracic cavity.
Using a thoracoscope, the specialist assesses the condition of the pleural cavity, performs the necessary manipulations (removes material for biopsy, drainage, etc.).
At the end of the intervention, a drain is placed in one of the incisions to drain accumulations of pleural fluid and maintain adequate intrapleural pressure.
In general, there are several variants of thoracoscopy. The most well-known is the Friedel method, which can be performed with both general and local anesthesia. [3] Through the incision, a special needle with a falling mandrel is introduced into the pleura, which facilitates the correct choice of the direction of the thoracoscopy channel. After that, a trocar with a short bronchoscopic tube is introduced through the incision, through which an aspirator with a soft tip for suctioning purulent or exudative secretions is passed inside the cavity. [4] Together with surgical instruments, an optical device for visualization and imaging of the pleura is introduced inside the cavity.
If thoracoscopy with biopsy is performed, the biomaterial is taken at the final stage of the operation. This requires special forceps connected to an optical device or a biopsy needle. Under telescopic observation, the forceps are brought to the area of the proposed biomaterial collection, open the brushes and bite off the necessary amount of tissue. A coagulator is used to stop bleeding.
Thoracoscopy of the pleural cavity is completed by applying deep U-shaped skin and muscle sutures to the incision site, except for the incision in which a silicone drainage connected to an aspiration apparatus is placed to remove residual fluid, air, and blood.
Diagnostic thoracoscopy usually lasts no more than 40 minutes, but therapeutic surgery can last several hours (on average 1.5-2.5 hours).
After the procedure, the patient is monitored to detect any complications in time.
Lung thoracoscopy is performed by a thoracic surgeon using intubation or general anesthesia, which is decided, depending on the status, age, other individual characteristics of the patient. Only general anesthesia is indicated for children, adolescents, or mentally unstable individuals. In some cases of therapeutic thoracoscopy, intraoperative disconnection of one lung is possible.
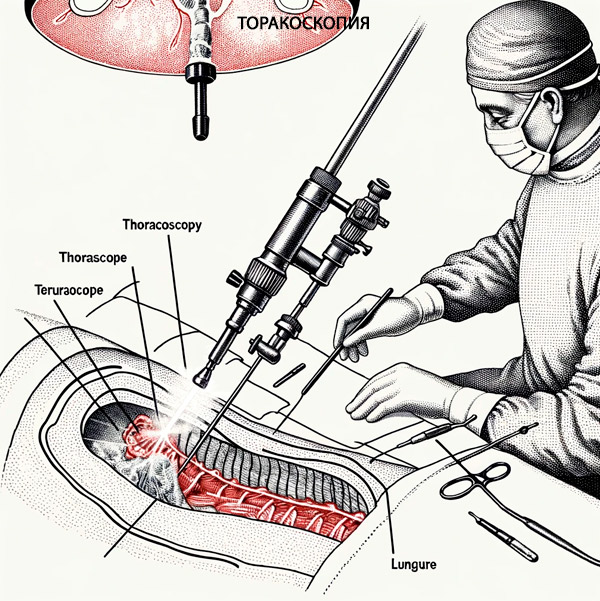
Patients with severe forms of pleurisy several days before endoscopy are performed pleural punctures, which allows to reduce the stressful effect of complete emptying of the pleural cavity of fluid during thoracoscopy, as well as to prevent sharp displacement of the mediastinum at the time of thoracoscope insertion. The device is a metal tube up to 10 mm in diameter with two optical channels. Through one channel light is delivered into the cavity under investigation, and through the second channel the image is transmitted to the camera screen and monitor. [5]
Thoracoscopy of the mediastinum is most often performed in the fourth intercostal space, slightly anterior to the mid axillary line. There are relatively few muscles and intercostal vessels in this area, minimizing the likelihood of injury. Meanwhile, the pleural space is clearly visible here. If there are coarse schwarts and drained fluid, thoracocentesis is performed in the area of extreme proximity of the cavity to the chest wall. Multiaxial fluoroscopy should be performed prior to surgery to determine the most appropriate point for thoracentesis. [6]
Contraindications to the procedure
The thoracoscopy operation itself does not pose a threat to the patient's life, so the indicated contraindications are always relative and are determined primarily by the condition of the body and its ability to tolerate general anesthesia. The procedure can be canceled if its qualitative performance can be questioned due to decompensation conditions, primarily on the part of the cardiovascular and respiratory system.
Surgical contraindications to thoracoscopy include:
- Complete fusion (obliteration) of the pleural cavity, which prevents the use of an endoscopic device, and increases the risks of organ damage and bleeding;
- Coagulopathy (blood clotting disorder).
Most thoracic surgeons consider signs of damage to the heart, main vasculature, large bronchi and trachea, and unstable hemodynamics as contraindications.
Thoracoscopy is not performed in case of myocardial infarction, cerebral stroke, severe impairment of cerebral circulation and some other concomitant diseases, which is determined on an individual basis.
Complications after the procedure
Thoracoscopy is a relatively safe intervention, which is always prioritized over cavity surgeries. The development of adverse effects after thoracoscopy is rare, although they cannot be completely ruled out.
Immediately during the operation, mechanical trauma to the lung or nearby organs is possible, sometimes vessels are damaged, bleeding occurs, although this already belongs to the category of surgical complications. At the postoperative stage there is a risk of infectious processes, edema, hemothorax, pneumothorax.
Patients after thoracoscopy may complain of cough, chest pain. In most cases, these are normal symptoms that go away within 2-3 days if bed rest and all medical recommendations are followed.
Complications can occur both during thoracoscopy and in the postoperative period. [7]
Damage to the lung, bleeding is possible if the instruments are inserted roughly and incorrectly. To correct the problem, the injured area is sutured. If the vascular injury is small, ligation or cauterization is used. If a large vessel is injured, thoracoscopy is interrupted and an emergency thoracotomy is performed.
Due to a sharp drop in blood pressure, cardiac dysfunction, lung collapse during chest puncture, shock may develop, which requires urgent resuscitation measures.
Violation of heart rhythm can be provoked by careless manipulations during intervention, irritation of the myocardium. Often it is not possible to identify the cause of arrhythmia.
Some patients report dyspnea after thoracoscopy. Oxygen therapy is used to eliminate this phenomenon.
Insufficient treatment of instruments, violation of sterility during thoracoscopy can lead to the entry of infection into the wound. Purulent inflammation manifests itself with pain in the area of the postoperative wound, fever, fever, general weakness.
If the lung tissue is not adequately sutured, a pneumothorax may develop, and damage to the serous membrane or infection can lead to pleurisy.
It is worth noting that the described complications after thoracoscopy are extremely rare.
Care after the procedure
After the thoracoscopy, the patient wakes up in the recovery room. If a drainage tube has been inserted, it will be connected to the drainage device.
The patient is left in the ward for a few hours or overnight, then transferred to an inpatient unit.
Smoking during the postoperative phase is prohibited.
Often the doctor recommends that you start moving as early as possible, get up periodically, walk as much as possible. This will prevent the development of lung inflammation and thrombosis. Also recommended are breathing exercises and special exercises to improve the state of the respiratory system.
The drainage tube is removed after the discharge has stopped. After removal, the doctor applies a dressing, which may be removed after 48 hours at the earliest.
Showering is allowed 2 days after drainage removal. If there is no discharge, it is not necessary to apply a dressing after a shower: it is enough to blot the incision sites with a dry clean towel.
Bathing after a thoracoscopy is not recommended until your doctor authorizes it.
A well-balanced diet high in protein, vegetables, fruits and whole grains is recommended. It is important to drink enough water (unless otherwise recommended by your doctor).
You should not plan to travel by airplane, you should consult your doctor beforehand.
It is not recommended to lift weights of more than 3-4 kg for a month after thoracoscopy.
Before discharge, the specialist will examine the condition of the surgical incisions, give the necessary recommendations on wound care. The stitches are removed on about 7 days.
The length of hospital stay depends on many factors - in particular, on the type and extent of the thoracoscopy intervention performed, on the initial diagnosis, and on the general condition of the patient.
It is imperative that you inform your doctor:
- If the shortness of breath has developed and worsened;
- If your chest, neck, face are swollen;
- If there's a sudden change in his voice, tachycardia;
- If the temperature rises above 38°C, there is discharge from the wounds (especially with an unpleasant odor, thick consistency).
In most cases, thoracoscopy is not accompanied by complications, recovery is relatively easy if the patient complies with all medical recommendations.

