Medical expert of the article
New publications
Egg
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The testicle (testis; Greek: orchis, s.didymis) is a paired male sex gland. The testicles are located in the scrotum, covered by a common skin and fleshy membrane of the scrotum, the remaining membranes are formed as a result of the protrusion of the layers of the anterior abdominal wall when the testicle descends from the retroperitoneal space into the scrotum. The testicles originate from undifferentiated mesenchymal rudiments located between the fold of the primary kidney and the root of the mesentery. The testicle is an oval body, flattened from the sides. The function of the testicles is the formation of male sex cells and hormones, therefore the testicles are simultaneously glands of external and internal secretion.
Functionally, the testicles are both an excretory and an endocrine organ. They serve as a target organ for pituitary hormones with a complex negative feedback mechanism.
The main hormone produced by the testicles (Leydig cells) is testosterone. The testicles also produce estrogens, mainly estradiol.
Testosterone has a pronounced anabolic activity, stimulates erythropoiesis. Testosterone has a number of inactive and active metabolites. Of the active metabolites, the most well-known are 5-a-dihydrotestosterone and androsterone. Testosterone metabolism occurs under the influence of 5 a-reductase enzymes. Androgen receptors are located in the nuclei of sex gland cells in muscles and other organs.
The inner surface of the convoluted tubules is lined with two types of cells, sustentocytes and spermatogonia, which are called primary germ cells. Spermatocytes mature in the seminiferous tubules.
The testicles, or testicles, are located in the perineum in a special receptacle - the scrotum, with the left testicle lower than the right. They are separated from each other by the scrotal septum and surrounded by membranes. The surface of each testicle is smooth and shiny. The length of the testicle is on average 4 cm, the width is 3 cm, the thickness is 2 cm. The weight of the testicle is 20-30 g. The testicle has a dense consistency, oval shape and is somewhat flattened from the sides. It has two surfaces: a more convex lateral surface (facies lateralis) and a medial surface (facies medialis), as well as two edges: the anterior edge (margo anterior) and the posterior edge (margo posterior), to which the epididymis is adjacent. The testicle has an upper end (extremitas superior) and a lower end (extremitas inferior). At the upper end of the testicle there is often a small appendage - the appendix testis, which is a rudiment of the cranial end of the paramesonephric duct.
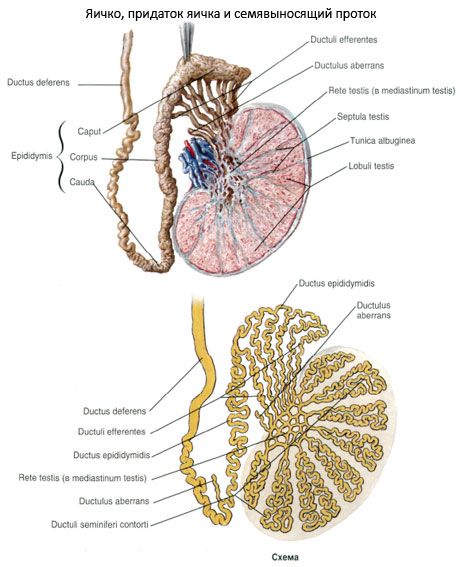
Structure of the testicle. The outside of the testicle is covered with a whitish fibrous membrane called the tunica albuginea. Under the membrane is the substance of the testicle - the testicular parenchyma (parenchyma testis). From the inner surface of the posterior edge of the tunica albuginea, a roller-shaped outgrowth of connective tissue penetrates into the parenchyma of the testicle - the mediastinum testis (mediastinum testis), from which thin connective tissue septa of the testicle (septula testis) fan out, dividing the parenchyma into lobules of the testicle (lobuli testis). The latter are cone-shaped and their apexes are directed toward the mediastinum testis, and their bases - toward the tunica albuginea. There are from 250 to 300 lobules in the testicle. In the parenchyma of each lobule there are two or three convoluted seminiferous tubules (tubuli seminiferi contorti) containing spermatogenic epithelium. Each of the tubules is about 70-80 cm long and 150-300 µm in diameter. Heading towards the mediastinum of the testicle, the convoluted seminiferous tubules in the area of the lobule apices merge with each other and form short straight seminiferous tubules (tubuli seminiferi recti). These tubules flow into the rete testis, which is located in the thickness of the mediastinum of the testicle. From the rete testis, 12-15 efferent testicular ducts (ductuli efferentes testis) begin, heading into its appendage, where they flow into the duct of the epididymis.
The convoluted seminiferous tubules are lined with spermatogenic epithelium and supporting cells (Sertoli cells) located on the basement membrane. Cells of the spermatogenic epithelium, which are at different stages of spermatogenesis, form several rows. Among them, stem cells, spermatogonia, spermatocytes, spermatids and spermatozoa are distinguished. Spermatozoa are produced only in the walls of the convoluted seminiferous tubules of the testicle. All other tubules and ducts of the testicle are pathways for the removal of spermatozoa.
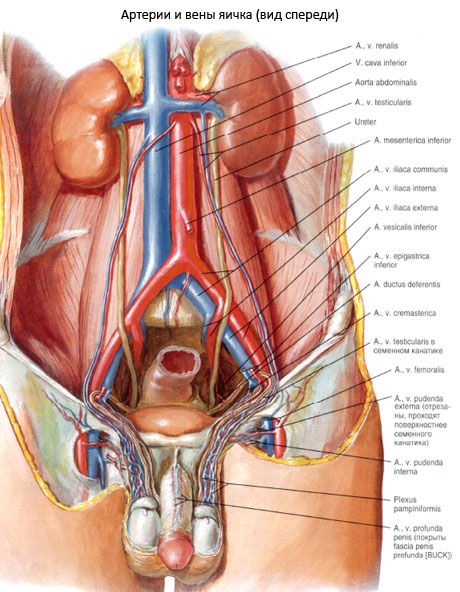
Vessels and nerves of the testicle and its epididymis. The testicle and epididymis are supplied with blood from the testicular artery (a branch of the abdominal aorta) and partly from the artery of the vas deferens (a branch of the internal iliac artery), which anastomoses with the testicular artery. Venous blood from the testicle and epididymis flows through the testicular veins, which form a pampiniform venous plexus as part of the spermatic cord. The veins of this plexus flow into the inferior vena cava on the right and into the left renal vein on the left. The lymphatic vessels of the testicle and epididymis flow into the lumbar lymph nodes.
The testicle and its appendage receive sympathetic and parasympathetic innervation from the ovarian plexus. The plexus also contains sensory nerve fibers.
Supporting cells (Sertoli cells) have a pyramidal shape, well-developed organelles (especially the non-granular endoplasmic reticulum and the Golgi complex). These cells reach the lumen of the convoluted seminiferous tubule with their apex. Supporting cells are the microenvironment for the spermatogenic epithelium, provide their trophism, and also isolate the developing germ cells from toxic substances, various antigens, and prevent the development of immune reactions. Sertoli cells can function as phagocytes. Supporting cells synthesize androgen-dependent protein, which transfers male sex hormones to spermatogenic cells.
Outside the basement membrane of the convoluted seminiferous tubule there is a thin layer of loose (fibrous) connective tissue containing smooth myocytes (contractile cells with actin). The straight seminiferous tubules are lined with prismatic epithelium, and the tubules of the rete testis are lined with cuboidal epithelium. The epithelium lining the efferent tubules is represented by tall ciliated and secretory cells. In addition, there is another type of cell in the testicle - interstitial endocrinocytes (Leydig cells). They are located in the loose fibrous connective tissue between the convoluted seminiferous tubules, around the blood capillaries. Leydig cells are large, round or polygonal, rich in glycoprotein inclusions, and have a pronounced endoplasmic reticulum.
What tests are needed?

