Medical expert of the article
New publications
Scrotum
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The scrotum is a protrusion of the anterior abdominal wall that has two separate chambers for the male sex glands. The scrotum is located below and behind the root of the penis. Inside the scrotum and in each of its chambers is a male sex gland.
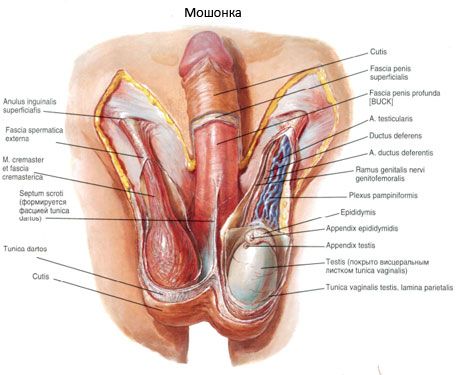
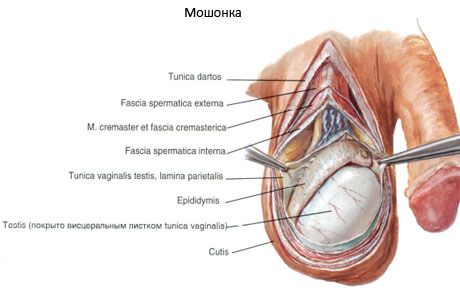
The scrotum has 7 layers (membranes), which are also called the testicular membranes:
- skin (cutis);
- fleshy shell (tunica dartos);
- external spermatic fascia (fascia spermatica externa);
- fascia of the muscle that lifts the testicle (fascia cremasterica);
- muscle that lifts the testicle (m.cremaster);
- internal spermatic fascia (fascia spermatica interna);
- the vaginal membrane of the testicle (tunica vaginalis testis), in which two layers (two plates) are distinguished: the parietal plate (lamina parietalis) and the inner plate (lamina visceralis).
The skin of the scrotum is thin, easily folds, is darker in color than in other parts of the body, and is covered with numerous hairs. Under the skin is the dartos (tunica dartos), formed from the subcutaneous connective tissue of the inguinal region and perineum and replacing the subcutaneous fat. The dartos contains bundles of smooth muscle cells and elastic fibers. There are no fat cells in it. The dartos forms the septum of the scrotum (septum scroti), separating the right testicle from the left. On the surface of the scrotum, the line of attachment of the septum corresponds to the scrotal suture (raphe scroti), which has a sagittal direction. Deeper lies the external spermatic fascia, which is a derivative of the superficial fascia of the abdomen. Under it is the fascia of the muscle that lifts the testicle, formed from the proper fascia of the external oblique muscle of the abdomen and partly from the fibrous fibers of its aponeurosis. Then there is the muscle that lifts the testicle (m.cremaster), consisting of muscle bundles that branch off from the transverse and internal oblique muscles of the abdomen. Inside the muscle is the internal spermatic fascia - a derivative of the transverse fascia of the abdomen. The internal spermatic fascia grows together with the parietal (parietal) plate of the vaginal membrane of the testicle, which at the posterior edge of the testicle passes into its visceral (visceral) plate covering the testicle and the epididymis. Between the visceral and parietal plates there is a slit-like closed cavity - a derivative of the peritoneal cavity.
Vessels and nerves of the scrotum
The anterior scrotal branches (branches of the external genital artery) and the posterior scrotal branches (branches of the perineal artery) branch out in the walls of the scrotum. A branch of the inferior epigastric artery approaches the muscle that lifts the testicle.
The anterior scrotal veins drain into the femoral vein, and the posterior scrotal veins are tributaries of the internal genital veins. The lymphatic vessels of the scrotum drain into the superficial inguinal lymph nodes.
The scrotum is innervated by the anterior scrotal nerves - branches of the genitofemoral nerve and the posterior scrotal nerves - from the genital nerve. The involuntary (smooth) muscles are innervated from the inferior hypogastric plexuses.
Descent of the testicle and formation of its membranes
The membranes of the male reproductive gland are formed during the descent of the testicle, in which the guiding ligament of the testicle (gubernaculum testis - BNA) plays an important role. The ligament is laid in the early stages of development retroperitoneally and extends from the caudal end of the rudiment of the testicle to the anterior abdominal wall, where the scrotum subsequently begins to form. Somewhat later, in the 3rd month of intrauterine development, a protrusion of the peritoneum appears in place of the future deep inguinal ring, forming its vaginal process (processus vaginalis peritonei). As the body of the embryo grows in length, the testicle occupies an increasingly lower position, moves retroperitoneally into the pelvic cavity, and then near the vaginal process of the peritoneum, where, being enveloped in a serous cover (the lower part of the vaginal process), it occupies its final position. Together with the vaginal process, other layers of the anterior abdominal wall protrude outward, forming the receptacle of the male reproductive gland - the scrotum.


 [
[