Medical expert of the article
New publications
Supratentorial foci of gliosis
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
When the process of glial cell proliferation occurs in the supratentorial region of the brain, i.e. The upper parts of the brain located above the cerebellar tentorium (tentorium cerebelli), the membrane separating the cerebellum from the occipital lobes of the brain, supratentorial foci of gliosis are formed.
Epidemiology
The exact number of cases of focal gliosis of the supratentorial region of the brain has not been calculated, and it is unknown. But after strokes, foci of reactive astrocytic gliosis are found in 67-98% of patients; in Alzheimer's disease - in 29-100% of patients, and in Parkinson's disease - in 30-55% of patients.
Clinical statistics indicate that in nearly 26% of epilepsy cases, the main neuropathologic abnormality is diffuse astrocytic gliosis, which does not develop due to neuronal damage.
Causes of the supratentorial foci of gliosis.
Gliosis refers to organic lesions of the brain and is considered a common reaction of glial cells (which make up about half of the total brain volume), in response to damage or death of nerve cells (neurons) surrounded by glia. [1] This lesion can result from:
- Of head trauma;
- Perinatal hypoxia or birth trauma in newborns;
- Hemorrhagic stroke, when supratentorial foci of gliosis of vascular genesis occur during cerebral circulatory disorders;
- Ischemic stroke with supratentorial foci of gliosis of residual genesis, i.e., associated with hypoxia and ischemia of white matter neurons;
- Cerebellar stroke;
- Of Korsakoff's syndrome;
- Immune-mediated damage to CNS myelinated axons in multiple sclerosis;
- Inflammation of the walls of blood vessels (vasculitis);
- Alzheimer's disease;
- Parkinson's disease;
- Charcot's neurodegenerative disease amyotrophic lateral sclerosis;
- Genetic Huntington's disease;
- Prion diseases, specifically creutzfeldt-Jakob disease;
- AIDS, which can lead to hIV dementia;
- Of a tuberculous brain lesion.
Pathological changes in the white matter of the brain in the elderly with replacement of neurons by glia cells are recognized as a manifestation of small vessel atherosclerosis and are associated with age-related vascular risk factors.
Also supratentorial foci of gliosis on the background of vascular microangiopathy - lesions of the walls of small blood vessels with impaired blood circulation in the brain tissue - are possible in cases of systemic lesions of connective tissue, infections and malignant neoplasms of the brain.
Risk factors
In addition, risk factors for gliosis foci in the brain are associated with chronic high blood pressure; hyperlipidemia and hypoglycemia; prolonged cerebral blood circulation disorders (leading to hypoxia of brain tissue); with prolonged neonatal asphyxia (leading to hypoxia of brain tissue); with a range of hereditary pathologies and genetic diseases; with epilepsy; with brain infections (encephalitis, meningitis of viral origin); with metabolic syndrome and alcoholism. [2]
Pathogenesis
Considering the pathogenesis of gliosis as a universal reaction to local brain damage or a general pathological process in the CNS, neurophysiologists note the uncertainty of the mechanism of this reaction.
However, it is known for sure that glial cells of the brain - unlike nerve cells - are able to multiply by division regardless of the age of a person. Glia cells not only maintain the stable position of neurons, but also provide their trophic support and regulate the extracellular fluid surrounding neurons and their synapses.
The stimulatory role of inflammatory cytokines - IL-1 (interleukin-1), IL-6 (interleukin-6) and TNF-α (tumor necrosis factor alpha) in the activation and proliferation of glial cells: astrocytes, microglia and oligodendrocytes was revealed.
For example, in response to brain damage, astrocytes (stellate glia cells) release chemical mediators of inflammation that attract eosinophils and some trophic blood factors; this increases the expression of glial fibrillary acidic protein (GFAP) with glia hypertrophy and astrocyte proliferation. This results in the formation of a glial scar that fills the neural tissue defect. At the same time, stellate cells inhibit regrowth of the damaged axon.
Resident brain phagocytes, microglia, which are also activated by inflammatory cytokines and growth factors, differentiate into macrophages and can cause immune reactions in demyelinating and neurodegenerative diseases, also react to damage to neurons and their axons.
In addition, the process of gliosis in strokes can begin due to damage to the capillaries of the brain and temporary disruption of the integrity of the blood-brain barrier. [3]
Symptoms of the supratentorial foci of gliosis.
Specialists distinguish: focal or single supratentorial foci of gliosis (in the form of a fairly large-sized overgrowth of glia in one place); few foci (no more than two or three), as well as multiple supratentorial foci of gliosis (more than three) and diffuse or multifocal supratentorial foci.
So, the general symptoms as well as the first signs of supratentorial gliosis foci depend on whether they are single or multiple, but are largely determined by their specific localization. In some cases, such foci do not manifest neurologically in any way.
Supratentorial structures are the cerebral hemispheres with the basal ganglia and thalamus; the occipital lobes (controlling vision and oculomotor functions); the parietal lobes (enabling perception and interpretation of physical sensations); the frontal lobe (which is responsible for logic, intelligence, individual thinking and speech development); and the temporal lobes (responsible for short-term memory and speech).
Thus, the clinical picture of focal neuronal replacement by glial cells may include headaches and dizziness; abrupt BP fluctuations; motor dysfunctions (changes in gait, ataxia, paresis, difficulty in maintaining body balance, seizures); sensory disturbances; problems with vision, hearing or speech; decreased attention, memory and cognitive functions, as well as behavioral disorders, which are already symptoms of dementia.
In most cases of supratentorial gliosis foci of vascular origin, there is symptomatology characteristic of dyscirculatory encephalopathy. [4]
Complications and consequences
The main negative consequences of focal gliosis of the supratentorial region are impairment of brain functions, which can manifest as symptoms of cognitive impairment, dementia, gait disturbances, hallucinations, depression, etc.
Complications of focal gliosis increase the risk of complete disability of the patient.
Diagnostics of the supratentorial foci of gliosis.
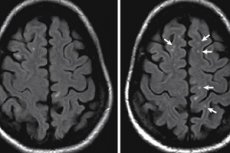
Only instrumental diagnostics - using magnetic resonance imaging (MRI) of the brain. Can detect a supratentorial focus of gliosis.
Visualized MR picture of single supratentorial foci of gliosis shows them in the form of intensely pronounced light areas of different configuration, which can be localized in different zones of brain structures belonging to the supratentorial ones. [5]
Differential diagnosis
Differential diagnosis is made with astrocytoma, craniopharyngioma, hemangioblastoma, ependymoma, and encephalomalacia.
Treatment of the supratentorial foci of gliosis.
It should be borne in mind that treatment is aimed not at the foci of gliosis in the brain matter (which can not be eliminated), but to ensure normal blood supply to the brain, improving the trophic nerve cells and the metabolic processes occurring in them, as well as to increase their resistance to hypoxia and oxidative stress.
The drugs Kavinton (Vinpocetine) and Cinnarizine contribute to normalization of cerebral blood supply. And the metabolism of nerve cells in the brain is stimulated by the use of nootropics: cerebrolysin, Piracetam, fezam (Piracetam + Cinnarizine), cereton (Cerepro), Ceraxon, calcium gopantenate.
Lipoic acid preparations may be prescribed as an antioxidant.
Prevention
General prevention includes the well-known principles of a healthy lifestyle. But, given the diseases in which gliosis foci appear in the supratentorial region of the brain, it is necessary to take prophylactic measures to prevent these pathologies - starting with atherosclerosis and strokes.
There are also recommendations for preventing Alzheimer's disease.
Forecast
The localization and distribution of supratentorial foci of gliosis, as well as their etiology and intensity of symptomatology directly affects the prognosis of the entire complex of emerging disorders of the CNS, affecting the quality of life of patients.

