Medical expert of the article
New publications
Sinus bradycardia: causes, symptoms, treatment
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Although the normal heart rate for most people fluctuates between 60 and 90 beats per minute, a persistent decrease is often observed, which is defined in cardiology as sinus bradycardia (ICD-10 code - R00.1).
What is it? It's an abnormality where your heart beats more slowly, meaning less than 60 times per minute. Why sinus? Because the heart rhythm is controlled by the sinoatrial node, which produces the electrical impulses that initiate each heartbeat.
Epidemiology
Differentiating between physiological and symptomatic sinus bradycardia is difficult, so statistics regarding their prevalence are unknown.
Although, as practice shows, only the pathological (symptomatic) type of decreased heart rate requires treatment, especially in the elderly, since the frequency of this symptom increases with age - as the corresponding diseases develop.
Causes sinus bradycardia
A symptom that manifests itself as a decrease in the heart rate does not necessarily indicate a disease. For example, when a person sleeps, the heart rate is lower than when awake. Therefore, a distinction is made between physiological and symptomatic (pathological) sinus bradycardia. And in most cases, doctors can identify its causes.
Thus, a decrease in heart rate during hypothermia (hypothermia of the body, accompanied by a slowdown in all metabolic processes) is not considered a pathology, as is unnoticed sinus bradycardia in elderly men and women - the result of changes in the heart caused by aging.
Sinus bradycardia in athletes is physiological, with a high, frequent, wandering tone; almost half of them simultaneously have sinus bradycardia and left ventricular hypertrophy, since the heart rate decreases with an increase in its volume and internal pressure due to increased physical exertion. For more information, see – Sports Heart
Physiologically, sinus bradycardia during pregnancy also occurs, occurring in the first half due to frequent vomiting characteristic of early toxicosis, and in later stages - when the uterus begins to exert mechanical pressure on the inferior vena cava. But due to anemia, pregnant women may experience sinus tachycardia.
Meanwhile, a persistent slowing of the heart rate can be a symptom of a variety of pathological conditions and diseases: congestive and hypertrophic cardiomyopathy; infectious myocarditis and endocarditis; post-infarction condition; hypothyroidism (deficiency of thyroid hormones); deficiency of potassium and/or magnesium in the blood (leading to electrolyte imbalance); arterial hypotension and vegetative-vascular dystonia; problems with the adrenal glands or pituitary gland; increased intracranial pressure; inflammation localized in the brain (for example, Lyme disease) and neoplasms.
The key causes of sinus bradycardia are disturbances in the cardiac conduction system, in which the sinus or sinoatrial node (nodus sinuatrialis) of the right atrium, the main pacemaker, plays a major role. And the combination of pathological abnormalities in its operation, leading to a decrease in heart rate, is called weak sinus syndrome.
However, the conduction defect in sinus bradycardia is also associated with disorders of the atrioventricular node - atrioventricular block (AV block), the clinical significance of which exceeds the weakness of the sinoatrial node. And problems with the conduction of impulses below the AV node are caused by Lenegret syndrome - idiopathic fibrosis and calcification of the conduction system.
Risk factors
Risk factors for persistent decrease in heart rate include: infectious and autoimmune diseases that cause complications for the heart; bleeding and hypoxia of any etiology; autonomic hyperreflexia; old age; prolonged bed rest; anorexia and "starvation diets"; exposure to toxic substances (poisoning), as well as smoking, alcohol abuse, and stress.
An important iatrogenic factor is the long-term use of antiarrhythmic drugs that block β-adrenergic receptors or calcium channels (Amiodarone, Verapamil, Propranolol, etc.); cardiac glycosides (digitalis group); tricyclic antidepressants and neuroleptics of the phenothiazine group, sedatives (including Valocordin and its analogues).
And risk factors for weakening the pacemaker and the development of bradycardia: myocardial ischemia, infarction (with scars in the area of the right atrium or interventricular septum), focal and diffuse degenerative changes in the myocardium with damage to the myocytes of the sinus node (sclerosis, calcification).
Pathogenesis
As cardiologists note, the pathogenesis of sinus bradycardia in parasympathetic hypertonus consists of overexcitation of the vagus nerve and its branches that innervate the sinoatrial node area.
And its dysfunction can be caused by several factors. Firstly, the heart rate decreases when the full blood supply to the sinus is disrupted and the trophism of the cells that form it deteriorates. Secondly, the pacemaker's automatism is partially "switched off" and it works at a lower speed. As a result, the interval between sinus depolarizations of cardiomyocytes (pacemaker neurons) increases, and this can lead to conditions defined as sinus bradycardia with sinus arrhythmia or sinus bradyarrhythmia with supraventricular tachycardia. Such conditions are called Frederick's syndrome.
When the sinus node is weak, impulses begin to be generated by the bundle of His, but they occur earlier than expected and alternately contract the muscle fibers of the ventricles of the heart - bypassing its atria. In such situations, sinus bradycardia and extrasystole can be diagnosed.
The transmission of the impulse itself may be disrupted, as it cannot freely pass from the sinus cells to the myocardium of the atria, or from the atria to the ventricles, due to second- and third-degree AV block.
Also, impulses can be delayed between the atrioventricular node and the atrioventricular bundle (His bundle). Then it would be more correct to define atrioventricular bradycardia. Read more - Conduction system of the heart. Partial disruption of impulse passage with a decrease in heart rate and an increase in pressure in the right ventricle indicates that this is an incomplete block of the right bundle of His and sinus bradycardia, which can occur with narrowing and prolapse of the mitral valve, ischemia and congenital heart defects, acute infarction, and are also a side effect of digitalis preparations (cardiac glycosides).
In case of heart defects associated with disturbance of interventricular hemodynamics, during the period of ventricular contraction, the pressure in them increases, slowing the heart rate, and sinus bradycardia with systolic overload is observed.
Explaining the influence of thyroid hormones on the heart rhythm, specialists emphasize that with insufficient synthesis of triiodothyronine and thyroxine in patients with hypothyroidism, not only is water-salt metabolism disrupted, but also the excitability of chromatin intra-tissue receptors of the sympathoadrenal system decreases. As a result, cells capture much fewer calcium ions, and this leads to a decrease in heart rate, cardiac output, and systolic blood pressure.
Symptoms sinus bradycardia
As noted above, sinus bradycardia in ICD-10 is assigned a place in class XVIII - among symptoms, signs and deviations from the norm. And the first signs of sinus bradycardia are a decrease in heart rate to 58-55 beats per minute, which may not be felt at all, and this is mild sinus bradycardia.
But as the heart rate decreases, sinus bradycardia can cause certain symptoms associated with disturbances in the functioning of the heart and general hemodynamics. Their intensity and range depend on the degree of decrease in the number of heart contractions per minute: 55-40 is moderate sinus bradycardia, less than 40 is severe sinus bradycardia.
Thus, among the non-specific symptoms accompanying sinus bradycardia of any etiology are: rapid fatigue, a feeling of general weakness, dizziness (even fainting), cold sweat, mild nausea, difficulty breathing and a feeling of discomfort in the chest area.
Severe sinus bradycardia – with a decrease in heart rate to 30 beats/min. and lower – is classified as an urgent terminal condition (in particular, with a significant decrease in the volume of circulating blood due to injuries and in cases of severe intoxication, cardiogenic shock, hypothyroid coma, etc.). It is manifested by cyanosis and cold extremities, severe dizziness, constriction of the pupils, convulsions, a drop in blood pressure, loss of consciousness and respiratory arrest.
Sinus bradycardia in children and adolescents
In younger children, the heart beats faster than in adults because the main physiological processes that ensure homeostasis of the child's body (body temperature and blood pressure, heart rate, etc.) are controlled by the sympathetic division of the autonomic nervous system (ANS).
In newborns, sinus bradycardia is defined as a heart rate of less than 100 beats per minute (the norm is about 120-160) and accompanies asphyxia during childbirth. And persistent bradycardia with partial AV block is considered a sign of congenital systemic lupus erythematosus or hereditary long QT syndrome.
Also, sinus bradycardia in children can be a consequence of sick sinus syndrome, which develops after heart surgery, and with congenital hypertrophy of the right ventricle.
Sinus bradycardia detected by a cardiologist in a teenager may develop due to the same weakness of the sinus node, but in most cases it turns out to be a symptom of autonomic nervous system disorders characteristic of puberty (due to hormonal changes).
In some adolescents, this condition is accompanied by manifestations of predominantly sympathicotonia; in others, signs of vagotonia are noted, that is, when physiology is “controlled” mainly by the parasympathetic division of the ANS. This is genetically determined and is called parasympathetic hypertonus, which is manifested by increased sweating, arterial hypotension, and episodes of sinus bradycardia often occur.
If both parts of the autonomic nervous system are equally excited, then this is amphotonia, and in different situations bradycardia, sinus bradyarrhythmia and paroxysmal tachycardia (that is, paroxysmal) can alternate.
Forms
There is no single systematization of this heart rhythm disorder, and different sources define the following types of sinus bradycardia: physiological, symptomatic (pathological or relative), absolute, central, organic (intracardiac, i.e. due to primary organic heart disease), extracardiac (not associated with heart disease), degenerative, toxic, idiopathic (of unknown etiology).
Vertical sinus bradycardia is distinguished - physiological, associated with a change in the location of the electrical axis of the heart (EOS). In addition, an ECG may reveal a deviation of the EOS to the left (characteristic of left ventricular hypertrophy) or its shift to the right (with possible right ventricular hypertrophy). These changes may be asymptomatic, but may manifest themselves as nonspecific symptoms.
Complications and consequences
You already know how dangerous sharp sinus bradycardia is, but a less pronounced symptomatic, toxic or idiopathic decrease in the number of heart contractions can also have consequences and complications.
Among them: insufficient blood supply to individual structures of the heart with the development of pain syndrome (angina); functional cardiac disorders (heart failure); increased thrombus formation; development of stroke, heart attack, Morgagni-Adams-Stokes syndrome, etc.
Diagnostics sinus bradycardia
Diagnostics include measuring pulse, blood pressure, auscultation with a stethoscope, blood tests (biochemical, thyroid hormone and electrolyte levels, rheumatic complex).
The anamnesis should contain information about all illnesses the patient has had and medications taken.
Instrumental diagnostics play a key role using: 12-lead electrocardiography (as well as 24-hour Holter), echocardiography, and, if necessary, ultrasound or MRI of the chest.
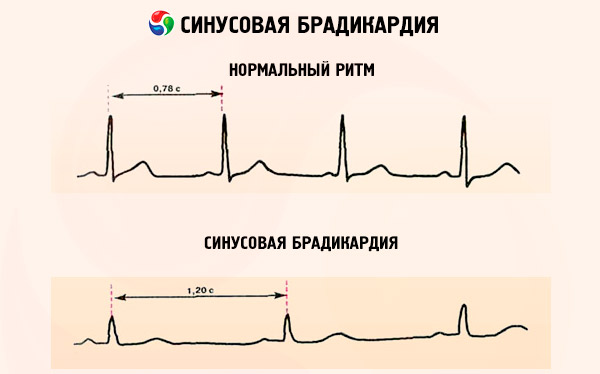
Sinus bradycardia on the ECG will be visible by a decrease in heart rate (the intervals between the R waves will be longer), by the presence of sinus rhythm (the P wave is always positive and is fixed in front of each ventricular complex - QRS); by a wider QRS complex.
Impulses originating within or below the His bundle on the ECG will create a wide QRS complex with a heart rate of 20 to 40 bpm.
What do need to examine?
Differential diagnosis
Differential diagnosis of cardiac rhythm abnormalities – including sinus arrhythmia, depolarization disorders, and early ventricular repolarization syndrome – is also performed on the basis of ECG, both normal and with physical activity.
Bradycardia or bradyarrhythmia can also occur due to problems with the transmission of electrical impulses by the ventricles, and intraventricular conduction disturbances are detected in patients with cardiac ischemia and the presence of heart valve pathologies caused by atherosclerosis, endocarditis or rheumatism.
More information in the material – Heart rhythm and conduction disorders.
Who to contact?
Treatment sinus bradycardia
According to experts from the European Society of Cardiology, for most people, treatment for sinus bradycardia is not required unless patients have symptoms that are clearly associated with a slow heartbeat that negatively affects overall hemodynamics.
What to treat and how to treat if symptoms are present? It depends on the etiology of the decreased heart rate and its accompanying manifestations. If sinus bradycardia is caused by hypothyroidism, then hormone replacement therapy (Levothyroxine) is indicated. Infectious myocarditis requires the use of antibiotics, in case of potassium and magnesium deficiency, tablets containing K and Mg are prescribed (Panangan, Kudesan, Kalinor, Potassium orotate, etc.).
Treatment is necessary for sinoatrial node dysfunction with severe clinical symptoms and severe atrioventricular block, and this is exclusively surgical treatment by implantation of a permanent pacemaker.
In other cases, to increase the heart rate, medications with a positive chronotropic effect can be prescribed, which is provided by drugs that block M-cholinergic receptors and agents that stimulate β-adrenoreceptors. These include: Atropine, Isadrine (Isoprenaline), Ipratropium bromide (other trade names - Itrop, Atrovent, Vagos, Normosecretol), Orciprenaline (Astmopent, Alupent, Alotek), Ephedrine, Epinephrine (Adrenaline), Norepinephrine.
Tablets (0.01 g) and injection solution Ipratropium bromide can only be prescribed by a doctor, who also determines the dose (standard - 0.5-1 tablet twice a day). The drug can disrupt urination, sweating, accommodation and bowel function; dries the mucous membrane in the mouth and reduces appetite. Contraindicated in prostate hypertrophy, glaucoma, intestinal stenosis, pregnancy (first trimester).
If there is no history of atherosclerosis, Orciprenaline can be used - 0.05% solution, tablets (20 mg). This drug is especially effective in cases of bradyarrhythmia, as well as in case of decreased heart rate after taking cardiac glycosides. The dose and duration of the course of treatment are determined by the attending physician.
Severe sinus bradycardia, which can lead to respiratory arrest, which may be followed by cardiac arrest, requires emergency care - with the administration of Atropine and cardiac stimulation.
Prevention
There are no specific measures to prevent any form of bradycardia. The easiest way is to prevent the influence of the iatrogenic factor, that is, to refuse medications that reduce the heart rate.
Otherwise, it remains to follow the standard recommendations of doctors: control cholesterol and blood pressure levels, reduce the amount of fat and salt consumed, have regular physical activity and quit smoking.
Forecast
The prognosis depends on many factors. In severe forms of sinus bradycardia (less than 40 bpm), the "slow" heart does not provide enough blood to meet the body's needs. This can cause negative consequences and be life-threatening.
The prognosis is good in patients with hypothyroidism, as treatment with thyroid hormones can relieve bradycardia and other symptoms.
At one time, the prognosis for people with third-degree AV block was poor, with 50% of patients dying within one year of diagnosis. However, the implantation of a permanent pacemaker has dramatically improved the situation.
Military service and sports
Sinus bradycardia and the army are incompatible if the pathology is accompanied by severe heart failure. In the case of asymptomatic mild or moderate bradycardia, the fate of conscripts is decided by a medical commission, which determines the possibility of being or not being "limitedly fit" for military service.
And the question of whether it is possible to play sports with sinus bradycardia should also be answered by a cardiologist - after examination and clarification of the causes of bradycardia. But moderate exercise without serious deterioration in health in the presence of this heart rhythm disorder is only welcome.


 [
[