Medical expert of the article
New publications
Right ventricular myocardial infarction
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A focus of necrosis of muscle tissue in the thickness of the wall of the right ventricle of the heart - its myocardium - is defined as a right ventricular myocardial infarction.
Acute myocardial infarction involving only the right ventricle is much less common than left ventricular myocardial infarction because the walls of the right ventricle are thinner and its pressure is lower. [1]
Epidemiology
Right coronary artery occlusion is rare, so infarction involving only right ventricular myocardium accounts for about 4% of cases. In 30% of clinical cases, focal myocardial necrosis of the right ventricle is observed in patients with inferior posterior transmural myocardial infarction of the left ventricle, and in 10-50% of cases it is combined with myocardial dysfunction of the inferior wall of the left ventricle.
The relatively small rate of right ventricular myocardial infarction can be explained by several factors: lower right ventricular oxygen demand due to lower muscle mass and workload; increased blood flow during diastole and systole; more extensive right ventricular collateralization, predominantly from the left coronary side; and diffusion of oxygen from intracameral blood through the thin wall of the PV into the physis veins. [2], [3]
Causes of the right ventricular myocardial infarction
The main cause of right ventricular myocardial infarction is acute coronary insufficiency resulting from the cessation of blood supply to the tissue of the right ventricular wall due to atherosclerotic occlusion of the proximal segment of the feeding vessel - the dominant right coronary artery, which branches from the right aortic sinus (above the right aortic valve leaflet), or the left anterior descending artery (left anterior interventricular artery).
Complete occlusion of the lumen of the right coronary artery from its origin to the middle of the pointed outer edge of the right ventricle by thrombosis or embolism can cause myocardial infarction not only of the right ventricle but also of the inferior wall of the left ventricle, often combined necrosis of the heart muscle in both ventricles. This is explained by the fact that the right coronary artery of the heart - in addition to supplying blood to the right ventricle - supplies blood to 25-30% of the left ventricle.
More information:
Risk factors
Factors that increase the risk of right ventricular myocardial infarction include:
- Angina pectoris (stable and unstable);
- Ischemic heart disease;
- High blood pressure (arterial hypertension);
- Elevated blood cholesterol levels (hyperlipidemia) leading to atherosclerosis of the heart vessels;
- Hypodynamia (lack of physical activity);
- Overweight and smoking.
Pathogenesis
The mechanism of myocardial cell (cardiomyocyte) alteration is due to the cessation of their blood supply, i.e., oxygen supply, which is necessary for intracellular metabolism.
As a result, necrotic death of cardiac myocytes occurs in the zone of ischemia - due to lack of oxygen and basic nutrients - with formation of granulation tissue by myofibroblasts and scar tissue by myocardial fibroblasts with accumulation of fibrillar collagen on the damaged area of myocardium.
Symptoms of the right ventricular myocardial infarction
In myocardial infarction of the right ventricle, the first signs are manifested by intense chest pain (radiating to the shoulder and scapula), dyspnea, peripheral edema and cold sweat.
See:
Also for infarction of this localization are characterized by such symptoms as
- Decrease in blood pressure in the form of uncontrollable hypotension;
- Swelling of the jugular vein due to increased inspiratory blood pressure in the right atrium and reverse blood flow (regurgitation) through the tricuspid aortic valve - Kussmaul's symptom.
The intensity of symptoms and the condition of patients depends on the stage of the infarction: acute (first two hours from the onset of the infarction), acute (first ten days), subacute (from the tenth day to two months) or scarring (which begins at the end of the second month from the onset of the infarction and lasts up to six months).
Depending on the depth of myocardial damage, types of right ventricular infarction are distinguished:
- Subepicardial (with a focus of necrosis in the outer layer, under the epicardium);
- Subendocardial (with damage to the inner layer - under the endocardium lining the inside of the heart);
- Intramural (with localization of the necrosis zone in the thickness of the ventricular wall),
- Transmural (with myocardial damage to the entire thickness of the myocardium).
Complications and consequences
Complications of right ventricular myocardial infarction range from severe arterial hypotension and ventricular fibrillation to cardiogenic shock. And sequelae include:
- Postinfarction cardiosclerosis;
- Myocardial akinesia;
- Damage to the interventricular septum leading to septal rupture;
- Right ventricular aneurysm;
- Dysfunction or rupture of the papillary muscles in the ventricular wall;
- Right-sided heart failure with dyspnea and edema;
- Development of atrioventricular block iI-III degree.
Diagnostics of the right ventricular myocardial infarction
The typical triad seen on physical examination is hypotension accompanied by jugular vein ballooning and clear lungs. Preserved left ventricular (LV) function confirms the diagnosis. [4]. A murmur of tricuspid regurgitation, Kussmaul's symptom (increased central venous pressure on inspiration as manifested by jugular vein distension), and paradoxical pulse are signs of significant hemodynamic effects due to right ventricular ischemia. [5]. In some cases, these symptoms are absent on admission and do not occur until diuretics or nitrates are prescribed.
The publication - myocardial infarction: diagnosis is devoted to diagnosis
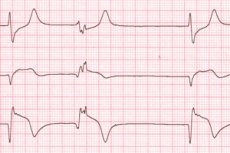
First of all, instrumental diagnostics are performed: electrocardiography (ECG), echocardiography, [6] coronarography, ventricular scintigraphy, coronary angiography.
Since the standard 12-lead electrocardiogram is insufficient to assess right ventricular involvement, right precardiac leads are always used. ECG signs of right ventricular myocardial infarction include: ST-segment elevation (upward shift) in the inferior leads (as well as in the left precardiac leads V1-V3); upward broad T waveform; and dilated Q waveforms. [8]
See also:
Blood tests are required for cardiac enzyme levels (troponins); creatine phosphokinase, aspartate aminotransferase, and lactate dehydrogenase isoenzymes; white blood cell count; and erythrocyte sedimentation rate (ESR).
Differential diagnosis with other acute cardiac and cardiovascular conditions with similar symptoms is necessary: cardiac tamponade, acute coronary syndrome, pulmonary embolism, constrictive pericarditis.
Who to contact?
Treatment of the right ventricular myocardial infarction
Treatment of right ventricular myocardial infarction is performed using:
- Reperfusion thrombolysis (antiplatelet or thrombolytic therapy) - to destroy the thrombus and restore blood supply to the myocardium;
- Intravenous infusion load - intravenous infusion of saline solution (40 ml per minute) with hemodynamic monitoring - to adjust right ventricular preload and optimize cardiac output;
- Control and maintenance of heart rate and rhythm, and atropine (0.5-1 mg w/v) is used in case of symptomatic decrease in HR;
- Inotropic support of myocardial contractility - by intravenous administration of cardiotonic agents, in particular Dobutamine (2-5 mcg per kg of body weight per minute with dose increase every 10 minutes).
For reperfusion thrombolysis, drugs such as Aspirin and Heparin and other drugs of the thrombolytic group are used intravenously: Streptokinase (Streptase), Tenecteplase, Alteplase.
One week after the onset of infarction, tablet inhibitors of platelet aggregation: Clopidogrel (Plavix) or Ticlopidine (Ticlid) may be prescribed.
Administration of Nitroglycerin in right ventricular myocardial infarction. By relaxing the smooth muscle fibers of vascular walls, Nitroglycerin causes their expansion, and also reduces blood pressure. It is used to relieve acute spasms of coronary vessels in angina pectoris. In right ventricular infarction - with a sharp decrease in BP - this drug can cause fainting, so its use is contraindicated. In addition, with impaired myocardial contraction and right ventricular insufficiency, nitrates can lead to worsening of the condition.
Read also - myocardial infarction: treatment
Prevention
In order to avoid myocardial infarction of any localization it is necessary to take measures to prevent cardiovascular pathologies, among which in the first place - atherosclerosis and coronary heart disease, which are the key cause of myocardial damage.
And for this you need to give up bad habits, maintain physical activity, get rid of excess weight and limit the consumption of foods high in "bad" cholesterol.
Forecast
Only timely and proper treatment gives a favorable prognosis for patients who have suffered a right ventricular myocardial infarction. And it should be remembered that it worsens in the presence of complications. See - myocardial infarction: prognosis and rehabilitation
If patients did not have right ventricular failure, hospital 30-day mortality was 4.4% with thrombolytic therapy and 3.2% with PCI. This figure increases to 13% with thrombolysis and 8.3% with PCI in patients with right ventricular failure. In patients with cardiogenic shock, mortality increases to 100% with thrombolysis and 44% with PCI. [9]

