Medical expert of the article
New publications
Transmural myocardial infarction
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
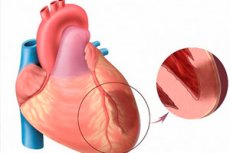
When speaking about acute myocardial infarction, we mean one of the most threatening forms of cardiac ischemia. It is about ischemic necrosis of a certain area of myocardium, which occurs as a result of an imbalance between the need for oxygen in the heart muscle and the actual level of its transport by blood vessels. Transmural myocardial infarction, in turn, is considered a particularly severe pathology, when necrotic foci damage the entire thickness of the ventricular wall, starting from the endocardium and up to the epicardium. Pathology is always acute and large-focal, culminating in the development of postinfarction cardiosclerosis. Symptomatology is pronounced brightly, compared with the picture of a typical infarction (exception - infarction of the posterior heart wall, often proceeding covertly). Prognosis directly depends on the timeliness of emergency medical care. [1]
Epidemiology
Cardiovascular diseases are considered the most common cause of death for patients in many economically developed regions of the world. For example, in European countries, more than four million people die annually from cardiac pathologies. It is noted that more than half of fatal cases are directly related to such risk factors as high blood pressure, obesity, smoking, low physical activity.
Myocardial infarction, as a complicated variant of the course of coronary heart disease, is currently the leading cause of disability in adults, with mortality rates of 11%.
Transmural infarction more often affects men belonging to the age category of 40-60 years. Women suffer this type of infarction 1.5-2 times less often.
In recent years, the incidence of transmural pathology in young patients 20-35 years of age has increased.
Transmural myocardial infarction is among the most severe and life-threatening conditions, hospital mortality often reaches 10-20%. The most frequent unfavorable outcome is observed in patients with concomitant diabetes mellitus, hypertension, as well as in recurrent infarct attacks.
Causes of the transmural myocardial infarction.
In the vast majority of patients, the development of transmural infarction is associated with occlusion of the main trunk or branch of the coronary arterial vessel. During this disorder, the myocardium experiences a lack of blood supply, hypoxia increases, which worsens with increasing load on the heart muscle. Myocardial functionality decreases, tissue in a certain part of it undergoes necrosis.
Direct narrowing of the coronary lumen occurs for reasons such as these:
- Chronic vascular pathology - atherosclerosis, accompanied by deposition of cholesterol elements (plaques) on the vessel walls - is the most frequent factor in the occurrence of myocardial infarctions. It is found in 95% of cases of lethal outcome from transmural infarction. A common sign of atherosclerosis is considered to be an increase in blood lipid levels. The risk of infarct complications increases dramatically when the vascular lumen is blocked by 75% or more.
- The formation and movement of blood clots within blood vessels - vascular thrombosis - is a less common but another possible cause of blood flow blockage in the coronary circulation. Thrombi can enter the coronary network from the left ventricle (where they are formed due to atrial fibrillations and valve pathology) or through an unclosed foramen ovale.
Special risk groups include people who have an aggravated hereditary predisposition (heart and vascular pathologies in the family line), as well as heavy smokers and people over 50-55 years of age. S[2]
Negative contributions to the formation of atherosclerosis are:
- Improper diet;
- Metabolic disorders, obesity;
- Insufficient physical activity, hypodynamia;
- Diagnosed arterial hypertension;
- Diabetes of any type;
- Systemic pathologies (primarily vasculitis).
Risk factors
The heart always reacts acutely to any circulatory failure and hypoxia. When the lumen of a coronary arterial vessel is blocked and it is impossible to provide alternative blood flow, cardiac myocytes - myocardial cells - begin to die in the affected area within half an hour.
Disturbed blood circulation as a result of atherosclerotic processes of the coronary network in 98% of cases becomes the "culprit" of transmural myocardial infarction.
Atherosclerosis can affect one or more coronary arteries. The narrowing of the affected vessel is different - by the degree of blood flow blockage, by the length of the narrowed segment. If a person's blood pressure rises, the endothelial layer is damaged, the atherosclerotic plaque becomes saturated with blood, which subsequently clots and forms a thrombus, aggravating the situation with a free vascular lumen.
A blood clot is more likely to form:
- In the area of the atherosclerotic plaque lesion;
- In the area of endothelial damage;
- At the site of the narrowing of the arterial vessel.
Increasing myocardial necrosis can have different sizes, and transmural necrosis often provokes rupture of the muscle layer. Factors such as anemia, infectious-inflammatory processes, fever, endocrine and metabolic diseases (including thyroid pathologies) worsen myocardial ischemia. [3]
The most significant risk factors for the development of transmural myocardial infarction are considered to be:
- Blood lipid imbalance;
- Long-term or heavy smoking;
- Diabetes;
- Increased blood pressure;
- Any degree of obesity;
- Psychosocial aspects (frequent stress, depression, etc.);
- Hypodynamia, lack of exercise;
- Improper nutrition (consumption of large amounts of animal fats and trans fats on the background of low consumption of plant foods);
- Alcohol abuse.
"Small", relatively rare risk factors are considered to be:
- Gout;
- Folic acid deficiency;
- Psoriasis.
Significantly worsen the course of myocardial infarction such factors as:
- Of being male;
- Thrombolysis;
- Acute coronary artery disease;
- Smoking;
- Hereditary aggravation for coronary heart disease;
- Left ventricular failure;
- Cardiogenic shock;
- Ventricular rhythm disturbances;
- Atrioventricular block;
- A second heart attack;
- Old age.
Pathogenesis
The process of infarction development proceeds with the formation of permanent changes in the myocardium and myocyte death.
A typical manifestation of myocardial infarction is the electrocardiographic detection of abnormal Q-beats exceeding the norm in duration and amplitude, as well as a slight increase in the amplitude of R-beats in thoracic leads. The ratio of Q and R-tooth amplitudes determines the depth of debridement. That is, the deeper Q and lower R, the more pronounced the degree of necrosis. Transmural necrosis is accompanied by disappearance of R-notches and fixation of the QS complex.
Before the development of coronary thrombosis, the endothelial layer of the atherosclerotic plaque is affected, which is accompanied by an increase in the level of thrombogenic blood factors (thromboxane A2, etc.). This is pushed by hemodynamic failures, abrupt changes in vascular tone, fluctuations in catecholamine indices.
Damage of atherosclerotic plaque with its central necrosis and extramural thrombosis, as well as with a small stenosis, often ends either with the development of transmural infarction or sudden coronary death syndrome. Fresh atherosclerotic masses containing large amounts of atherogenic lipoproteins are especially prone to rupture.
The onset of myocardial damage most often occurs in the pre-morning hours, which is explained by the presence of circadian changes in coronary vascular tone and changes in catecholamine levels.
The development of transmural infarction at a young age may be due to congenital defects of coronary vessels, embolism due to infective endocarditis, cardiac myxomas, aortic stenosis, erythremia, etc. In these cases, there is an acute imbalance between the need of the heart muscle in oxygen and its supply through the circulatory system. Transmural necrosis is aggravated by hypercatecholemia.
Obviously, in most cases of acute transmural myocardial infarction, the cause is stenotic atherosclerosis of coronary vessels, thrombosis and prolonged occlusive spasm.
Symptoms of the transmural myocardial infarction.
The clinical picture in transmural infarction goes through several stages, which are symptomatically different from each other.
The first of the stages is prodromal, or preinfarction, which lasts about one week and is associated with stress or physical overload. The symptomatology of this period is characterized by the appearance or aggravation of angina attacks, which become more frequent and severe: unstable angina develops. The general well-being also changes. Patients begin to experience unmotivated weakness, fatigue, mood loss, anxiety, sleep is disturbed. Painkillers, which previously helped in the elimination of pain, now do not show effectiveness.
Then, if no help is rendered, the next - acute - stage of pathology occurs. Its duration is measured from the moment of ischemia of the heart muscle to the first signs of its necrosis (usual duration - from half an hour to a couple of hours). This stage starts with a burst of cardiac pain radiating to the upper extremity, neck, shoulder or forearm, jaw, scapula. The pain may be either continuous (lingering) or wavy. There are signs of stimulation of the autonomic nervous system:
- Sudden weakness, feeling short of breath;
- An acute sense of fear of death;
- "drenching" sweat;
- Difficulty breathing even at rest;
- Nausea (possibly to the point of vomiting).
Left ventricular failure develops, characterized by dyspnea and decreased pulse pressure, followed by cardiac asthma or pulmonary edema. Cardiogenic shock is a possible complication. Arrhythmias are present in the vast majority of patients.
First signs
The first "bells" of transmural infarction most often appear a few hours or even days before the development of an attack. People who are attentive to their health may well pay attention to them and seek medical help in a timely manner.
The most likely signs of impending pathology:
- Occurrence of chest pain at times or immediately after physical activity, strong emotional states and experiences;
- More frequent occurrence of angina attacks (if there were any before);
- A feeling of an unstable heart, a strong heartbeat, and dizziness;
- Lack of effect from Nitroglycerin (chest pains are not controlled, although the drug helped before).
It is important to understand the seriousness of the situation: among all recorded cases of transmural infarction, at least 20% of them are fatal within the first 60 minutes of the attack. And the fault of the medics here, as a rule, is not. Lethal outcome occurs due to delay on the part of the patient or his loved ones, who are not in a hurry to contact doctors and do not call "emergency help" in a timely manner. It should be remembered that if there is a person with an increased risk of heart attack in the family, all close people should clearly know the algorithm of their actions at the time of development of a cardiac attack.
Transmural myocardial infarction can be suspected by a rather strong and persistent pain syndrome. Painful manifestations - squeezing, pecky - they are felt in the chest, are able to "recoil" in the upper extremity (more often the left), the shoulder or neck area, the side of the body or the shoulder blade. Additional signs to which attention should be paid:
- The sensation of not having enough air to breathe;
- A sense of dread, a premonition of his own death;
- Increased sweating;
- Skin pallor.
One of the distinguishing features of myocardial infarction from the usual angina attack: the pain syndrome does not self-eliminate at rest, does not disappear after resorption of Nitroglycerin, lasts more than 15-20 minutes. [4]
Stages
According to morphological signs, the course of myocardial infarction has three stages (they are rarely indicated in the diagnosis line, since it is more appropriate to prescribe the duration of pathology in days):
- Ischemia stage (a little earlier it was called acute focal ischemic myocardial dystrophy stage) - lasts up to 6-12 hours.
- Necrosis stage - lasts up to 1-2 weeks.
- Organization stage - lasts up to 4 weeks or more.
Forms
Depending on the localization of the pathological focus, distinguish such types of transmural infarction:
- Anterior wall lesion (anterior, anterosuperior, anterolateral, anteroseptal transmural infarction;
- Lesion of the posterior (lower) wall (inferior, inferolateral, inferior posterior, diaphragmatic infarction);
- Apical-lateral, upper-lateral, basal-lateral lesions;
- Posterior, lateral, posterior-basal, posterolateral, posterior-septal lesions;
- Massive right ventricular infarction.
According to the spread of the pathologic necrotic process, there are other types of infarct foci besides transmural:
- Intramural;
- Subepicardial;
- Subendocardial.
Most patients are diagnosed with transmural and subendocardial lesions.
Depending on the extent of the damage, distinguished:
- Micronecrosis (aka focal necrosis);
- Shallow necrosis;
- Large-focal necrosis (in turn, subdivided into small, medium and extensive variant).
Transmural infarction of the anterior myocardial wall is more often associated with occlusion of the main trunk of the left coronary artery, or its branch - the anterior descending artery. Pathology is often accompanied by ventricular extrasystole or tachycardia, supraventricular arrhythmia. Conduction disturbances are usually stable, because they are associated with necrosis of the structures of the conductive system.
Transmural infarction of the inferior myocardial wall affects the areas adjacent to the diaphragm - the diaphragmatic section of the posterior wall. Sometimes such an infarction is called posterior diaphragmatic, diaphragmatic, or inferior. Such a lesion often proceeds by abdominal type, so the problem is often confused with diseases such as acute appendicitis or pancreatitis.
Acute transmural myocardial infarction of the left ventricle occurs in the vast majority of transmural lesions. The focus of necrosis may be localized in the anterior, posterior or inferior wall, apex, interventricular septum, or involve several zones simultaneously. The right ventricle is relatively rarely affected, and the atria even less frequently.
Transmural anterolateral myocardial infarction is one of the forms of left ventricular damage, in which the electrocardiogram shows increased Q-tooth in leads I, aVL, V4-6, as well as ST-segment displacement upward from isolation and negative coronary T-tooth. The anterior aspect of the lateral wall of the left ventricle is affected due to occlusion of the diagonal arteries or branches of the left circumflex artery.
Transmural inferolateral myocardial infarction is a consequence of occlusion of the anterior descending artery or envelope arterial trunk.
Transmural myocardial infarction of the lateral wall results from occlusion of the diagonal artery or the posterolateral branch of the left circumflex artery.
Transmural anterior septal myocardial infarction is characterized by the location of the necrotic focus in the right part of the anterior wall of the left ventricle and in the anterior part of the interventricular septum, which is also the left ventricular right wall. As a result of the lesion, excitation vectors depart to the back and to the left, so characteristic electrocardiographic changes are noted only in the right thoracic leads.
Large-focal transmural myocardial infarction, otherwise known as extensive or MI with pathologic QS, is the most dangerous type of pathology, which has very serious and life-threatening consequences for the patient. Extensive transmural myocardial infarction leaves practically no chance for patients.
Complications and consequences
Complications in transmural infarction are, unfortunately, not uncommon. Their development can dramatically change the prognosis of the disease. Among the most common adverse effects are cardiogenic shock, severe rhythm disturbances and acute heart failure.
The vast majority of delayed outcomes are due to the formation of a connective tissue zone in the area of dead cardiac tissue. The prognosis can be relatively improved by cardiac surgery: the operation may consist of aortocoronary bypass, percutaneous coronary angiography, etc.
Connective tissue replacement of the affected area prevents full myocardial contraction. Conduction disorders occur, cardiac output changes. Heart failure is formed, the organs begin to experience serious hypoxia.
It takes time and intensive rehabilitation measures for the heart to adapt to the new working conditions to the maximum extent possible. Treatment should be continuous, physical activity should be increased gradually, under the careful supervision of a medical specialist.
Some of the most common delayed complications include:
- Cardiac aneurysm (structural change and bulging of the heart wall in the form of a sac, which leads to decreased blood ejection and increasing heart failure);
- Thromboembolism (may occur due to physical inactivity or failure to follow medical advice);
- Chronic failure of cardiac function (occurs as a result of impaired left ventricular contractile activity, manifested by leg edema, dyspnea, etc.).
The risks of complications after transmural infarction are present throughout the patient's life. Especially often patients develop a recurrent attack or relapse. The only way to avoid its development is to regularly visit a cardiologist and exactly follow all his recommendations.
Transmural myocardial infarction is a very severe pathology, which, when complications join, leaves almost no chance for the patient. Among the most common consequences:
- Violations of rhythmic cardiac activity (atrial fibrillation, extrasystolic arrhythmias, paroxysmal tachycardia). Often the patient dies when ventricular fibrillation occurs with further transformation into fibrillation.
- Increasing heart failure with left ventricular dysfunction and, as a consequence, pulmonary edema, cardiogenic shock, a sharp drop in blood pressure, blocked renal filtration and - lethal outcome.
- Pulmonary-arterial thromboembolism, which results in lung inflammation, pulmonary infarction and - death.
- Cardiac tamponade due to rupture of the myocardium and rupture of blood into the pericardial cavity. In most of these cases, the patient dies.
- Acute coronary aneurysm (bulging scar area) followed by increasing heart failure.
- Thromboendocarditis (fibrin deposition in the cardiac cavity with its further detachment and stroke, mesenteric thrombosis, etc.).
- Postinfarction syndrome, which includes the development of pericarditis, arthritis, pleurisy, etc.
As practice shows, the largest proportion of patients who underwent transmural myocardial infarction die in the early (less than 2 months) postinfarction stage. The presence of acute left ventricular failure significantly aggravates the prognosis. [5]
Diagnostics of the transmural myocardial infarction.
Diagnostic measures should be carried out as soon as possible. At the same time, the completeness of diagnosis should not be neglected, because many diseases, not only cardiac pathologies, can be accompanied by a similar clinical picture.
The primary procedure is electrocardiography, which indicates coronary occlusion. It is important to pay attention to the symptomatology - in particular, a pronounced chest pain syndrome lasting 20 minutes or more, which does not respond to the administration of Nitroglycerin.
Other things to look out for:
- Pathologic signs preceding the seizure;
- "recoil" of pain in the neck, jaw, upper extremity.
Pain sensations in transmural infarction are more often intense, at the same time there may be breathing difficulties, disorders of consciousness, syncope. Transmural lesion has no specific signs. Irregularity of heart rate, brady or tachycardia, moist hoarseness are possible.
Instrumental diagnosis, first of all, should be represented by electrocardiography: this is the main research method, which reveals a deep and dilated Q-tooth, reduced R amplitude, ST-segment elevation above the isoline. After some time, the formation of a negative T-tooth, ST-segment decrease is noted.
Coronarography can be used as an additional method. This is a particularly accurate method that allows not only to detect coronary vessel occlusion by a thrombus or atherosclerotic plaque, but also to assess the functional capacity of the ventricles, detect aneurysms and dissections.
Laboratory tests are also mandatory - first of all, the MB fraction of CPK (creatine phosphokinase-MB) - myocardial fraction of total creatine phosphokinase (specific indicator of myocardial infarction development) - is determined. Additionally, cardiac troponins (quantitative study), as well as myoglobin level are determined.
To date, other new indicators have been developed, which, however, are not yet widely used. These are fatty acid binding protein, myosin light chains, glycogen phosphorylase BB.
At the pre-hospital level, diagnostic immunochromatographic testing (rapid tests) is actively used, helping to quickly determine the biomarkers troponin, myoglobin, creatine kinase-MB. The result of a rapid test can be evaluated in as little as ten minutes. [6]
Acute transmural myocardial infarction ECG
The classical electrocardiographic picture in infarction is represented by the appearance of pathologic Q-tooths, the duration and amplitude of which are higher than normal values. In addition, there is a weak increase in the amplitude of R-beats in thoracic leads.
Pathological Q-tooths provoked by cardiac muscle necrosis are visualized 2-24 hours after the start of clinical manifestations. Approximately 6-12 hours after the onset, ST-segment elevation subsides, and Q-tooths, on the contrary, become more intense.
The formation of pathologic Q-notches is explained by the loss of the ability of dead structures to electrical excitation. Postnecrotic thinning of the anterior left ventricular wall also reduces its potential, as a result, there is an advantage of depolarization vectors of the right ventricle and left ventricular posterior wall. This entails an initial negative deviation of the ventricular complex and the formation of pathologic Q-tooths.
Decreased depolarization potential of dead cardiac tissue also contributes to a decrease in the amplitude of R-beats. The extent and spread of the infarction is assessed by the number of leads with abnormal Q-tooths and decreased R-tooth amplitude.
The depth of necrosis is judged by the relationship between the amplitudes of Q and R beats. Deeper Q and lower R indicate a pronounced degree of necrosis. Since transmural myocardial infarction directly involves the entire thickness of the heart wall, R-tooths disappear. Only a negative shape of the plaque, called QS-complex, is recorded. [7]
|
Electrocardiographic signs of transmural myocardial infarction |
|
The electrocardiogram (usually in thoracic leads) shows abnormal Q-notches and QS complexes. The same changes may be present in endocarditis with myocardial involvement, purulent and aseptic myocarditis, cardiomyopathy, progressive muscular dystrophy and so on. It is important to perform a qualitative differential diagnosis. |
Differential diagnosis
Transmural myocardial infarction is often differentiated with other causes of pain syndrome behind the sternum. This may be a dissecting thoracic aortic aneurysm, pulmonary embolism, acute pericarditis (mainly of viral etiology), intense radicular syndrome. During diagnosis, the specialist necessarily pays attention to the presence of risk factors for atherosclerosis, the peculiarities of the pain syndrome and its duration, the reaction of the patient's body to the use of analgesics and vasodilators, blood pressure values. The results of objective examination, electrocardiogram, echocardiogram, laboratory tests are evaluated. [8]
- Dissecting aortic aneurysm is characterized by the appearance of pain more often between the shoulder blades. The pain shows resistance to nitrates, and there is a history of arterial hypertension. There are no obvious electrocardiographic changes in this case, the indices of cardiac markers are normal. There is intense leukocytosis and LF shift to the left. To clarify the diagnosis, echocardiography, aortography with contrast, computed tomography are additionally prescribed.
- Pericarditis requires a careful analysis of past infectious respiratory diseases. Note changes in pain on inhalation and exhalation or in different body positions, pericardial friction murmurs, and nondynamic cardiac markers.
- Recurrence of osteochondrosis and plexitis is accompanied by pain on the side of the sternum. The pain depends on the patient's posture and respiratory movements. Palpatory reveals the point of extreme pain sensation in the zone of nerve endings discharge.
- Pulmonary embolism is characterized by more profound pain than transmural infarction. Paroxysmal respiratory distress, collapse, and redness of the upper body are often present. The electrocardiographic picture has similarities with the infarct lesion of the myocardium of the lower location, but there are manifestations of acute overload of the cardiac compartments on the right side. During echocardiography, intense pulmonary hypertension is noted.
- The picture of acute abdomen is accompanied by signs of peritoneal irritation. Leukocytosis is strongly pronounced.
Transmural myocardial infarction is also differentiated with acute pancreatitis, hypertensive crisis.
Who to contact?
Treatment of the transmural myocardial infarction.
Therapeutic interventions should have the following sequential goals:
- Pain relief;
- Restoring blood supply to the heart muscle;
- Reducing the load on the myocardium and decreasing its oxygen demand;
- Limiting the size of the transmural focus;
- Preventing the development of complications.
Pain relief allows to improve the patient's well-being and normalize the nervous system. The fact is that excessive nervous activity provoked by severe pain contributes to increased heart rate, increased blood pressure and vascular resistance, which further aggravates myocardial load and increases the need for oxygen in the heart muscle.
Drugs that are used to eliminate pain syndrome are narcotic analgesics. They are administered intravenously.
To restore adequate blood supply to the myocardium, coronarography, thrombolysis (thrombolytic) therapy, aortocoronary bypass surgery are performed.
Coronarography is combined with stenting or balloon angioplasty to restore the patency of the artery with a stent or balloon and normalize blood flow.
Thrombolytic therapy also helps restore venous (coronary) blood flow. The procedure consists of intravenous injection of appropriate thrombolytic drugs.
Aortocoronary bypass is one of the surgical options for resuming and optimizing the coronary blood supply. During bypass surgery, the surgeon creates a bypassing vascular pathway that allows blood flow to the affected areas of the myocardium. This operation can be performed as an emergency or elective procedure, depending on the situation.
In order to reduce cardiac load and minimize hypoxia, such groups of drugs are prescribed:
- Organic nitrates - contribute to the elimination of pain, limit the spread of necrotic focus, reduce mortality from transmural infarction, stabilize blood pressure (initially administered intravenous drip, after a while transferred to the tablet form of drugs);
- β-adrenoblockers - potentiate the effect of nitrates, prevent the development of arrhythmias and increased blood pressure, reduce the severity of myocardial hypoxia, reduce the risk of physical complications (in particular, ventricular rupture).
If the patient develops complications, such as pulmonary edema, cardiogenic shock, cardiac conduction disturbances, the therapeutic regimen is adjusted individually. Physical and mental peace of mind must be ensured.
Each of the stages of therapy of patients with transmural infarction is carried out according to certain schemes and protocols. As auxiliary medications may be prescribed:
- Antiaggregant drugs - reduce platelet aggregation, inhibit the formation of blood clots. In most cases of transmural infarction, patients are prescribed dual antiplatelet therapy, which consists of taking two versions of antiaggregants simultaneously for a year.
- Angiotensin-converting enzyme inhibitor drugs - help stabilize blood pressure, prevent heart deformity.
- Anticholesterol drugs (statins) - used to improve lipid metabolism, lower levels of low-density lipoproteins and cholesterol - potential markers of atherosclerotic progression.
- Anticoagulants - prevent blood clots from forming.
Drug therapy is necessarily complemented by general restorative measures - in particular, it requires careful observance of rest and bed rest, dietary changes (therapeutic table № 10 AND), gradual expansion of physical activity.
For the first 24 hours after an attack, the patient should be kept in bed for the first 24 hours. Questions about the gradual resumption of motor activity are discussed with the attending physician individually. It is recommended to practice breathing exercises to prevent pulmonary stasis.
The food ration is limited, reducing the caloric content to 1200-1500 kcal. Exclude animal fats and salt. The menu is expanded by vegetable food, potassium-containing products, cereals, seafood. The amount of fluid intake is also limited (up to 1-1.5 liters per day).
Important: the patient should completely stop smoking (both active and passive) and alcohol consumption.
After a transmural infarction, a person is shown a mandatory dispensary with a cardiologist. At first, observation is carried out weekly, then - twice a month (the first six months after the attack). After six months, it is enough to visit the cardiologist monthly. The doctor conducts an examination, performs control electrocardiography, stress tests. [9]
Surgical treatment
Surgical treatment for transmural infarction can be open (with access through a chest incision) and percutaneous (involves probing through an arterial vessel). The second technique is increasingly used due to its effectiveness, low-trauma and minimal complications.
Common types of percutaneous surgeries:
- Venous stenting is the placement of a special dilating element in the area of narrowing of the vessel. The stent is a cylindrical mesh made of special plastic or metal. It is delivered by means of a probe to the necessary vascular area, where it is expanded and left. The only significant possible complication of this treatment may be retrombosis.
- Balloon vascular plasty is a procedure similar to stenting, but instead of a mesh cylinder, the probe delivers a special balloon frame that inflates upon reaching the desired vascular area and dilates the vessel, thereby restoring normal blood flow.
- Laser excimer vascular plasty - involves the use of a fiber-optic probe, which, when brought to the affected segment of the coronary artery, conducts laser radiation. The rays, in turn, affect the clot and destroy it, thanks to which blood circulation is restored.
The practice of open heart surgery is reasonable for patients with complete arterial occlusion, when stenting is not possible, or in the presence of concomitant coronary pathologies (e.g., heart defects). In such a situation, bypass surgery is performed, bypassing vascular pathways are laid (with autoimplants or synthetic materials). The operation is performed with cardiac arrest and the use of AIC ("artificial circulation"), or on a working organ.
The following types of bypasses are known:
- Mammarocoronary - the internal thoracic arterial vessel, which is less prone to atherosclerotic changes and does not have valves like a vein, is used as a shunt.
- Aortocoronary - the patient's own vein is used as a shunt, which is sewn to the coronary artery and aorta.
Any heart surgery is a potentially dangerous procedure. The operation usually lasts several hours. For the first two days, the patient stays in the intensive care ward under constant supervision of specialists. In the absence of complications, he is transferred to a regular ward. The peculiarities of the rehabilitation period are determined individually.
Prevention
Preventive measures to prevent the development of transmural infarction are aimed at reducing the negative impact of potential harmful factors on the human body. Especially important is the prevention of a repeated attack in sick people. In addition to medication support, they should follow a number of medical recommendations, including changes in nutrition, correction of physical activity and lifestyle.
Thus, prevention can be primary (for people who have never had a transmural or other infarction before) and secondary (to prevent recurrence of myocardial infarction).
If a person is in the risk group for the development of cardiovascular pathology, then the following recommendations are prepared for him:
- Increase physical activity.
Hypodynamia can provoke many cardiovascular problems. Support of cardiac tone is especially necessary for people over 35-40 years of age. You can simply and effectively strengthen the heart by daily walking, jogging, swimming and cycling.
- Completely give up bad habits.
Smoking and drinking alcohol is harmful to anyone, regardless of their initial state of health. And for people with cardiovascular pathologies, alcohol and cigarettes are categorically contraindicated. And this is not just words, but a proven fact.
- Eat quality and proper nutrition.
Nutrition is the foundation of our overall health and vascular health. It is important to consume as little fried foods, animal fats, products with synthetic substitutes, trans fats, large amounts of salt as possible. It is recommended to expand the diet with vegetables, greens, fruits, nuts, berries, seafood.
- Avoid the negative effects of stress, seek more positive emotions.
It is desirable to avoid, if possible, excessive emotional stress and shocks. People prone to worry and anxiety, who often take situations "close to the heart", are recommended to take sedatives (after consultation with a doctor).
- Monitor blood pressure readings.
Often the processes leading to subsequent spasms and blockage of the vascular lumen are provoked by an increase in blood pressure. To avoid such complications, you should independently monitor blood pressure, take antihypertensive drugs prescribed by a doctor in a timely manner.
- Control blood sugar levels.
Patients with diabetes mellitus have problems with the condition of the vascular walls, which become more brittle and easily clogged due to the disease. To prevent the development of pathological intravascular processes, it is necessary to regularly consult an endocrinologist, undergo treatment and stay under systematic medical control (to monitor blood sugar values).
- See a cardiologist regularly.
People at risk of developing transmural infarction or other heart diseases should be systematically (1-2 times a year) examined by a general practitioner and a cardiologist. This recommendation is especially relevant to patients over 40-45 years of age.
Secondary prevention is to prevent the development of a repeated attack of transmural infarction, which can be fatal for the patient. Such preventive measures include:
- Notifying your doctor of any suspicious symptoms (even relatively harmless ones);
- Following the doctor's prescriptions and advice;
- Ensuring adequate physical activity, diet and lifestyle adjustments;
- Selection of a type of work activity that does not require excessive physical exertion and is not accompanied by psycho-emotional shocks.
Forecast
Pathologies of the cardiovascular apparatus are the most frequent factor of increased mortality. Transmural myocardial infarction is the most dangerous complication of ischemic heart disease, which cannot be "curbed" even despite the constant improvement of diagnostic and therapeutic methods.
Survival after an attack depends on many factors - first of all, on the speed of medical care, as well as on the quality of diagnosis, general health and age of the person. In addition, the prognosis depends on the period of hospitalization from the moment of attack onset, the extent of heart tissue damage, blood pressure values, etc.
Most often, experts estimate the survival rate at one year, followed by three, five and eight years. In most cases, if the patient does not have kidney pathologies and diabetes mellitus, a three-year survival rate is considered realistic.
The long-term prognosis is mainly determined by the quality and completeness of treatment. The highest risk of death is reported in the first 12 months after the attack. The main factors of patient death are:
- Infarct recurrence (most common);
- Chronic myocardial ischemia;
- Sudden cardiac death syndrome;
- Pulmonary embolism;
- Acute circulatory disorder in the brain (stroke).
Properly conducted rehabilitation measures play a crucial role in the quality of prognosis. The rehabilitation period should pursue the following objectives:
- Provide all conditions for the recovery of the organism, its adaptation to standard loads;
- Improve quality of life and performance;
- Reduce the risks of complications, including recurrences.
Quality rehabilitation interventions should be sequential and uninterrupted. They consist of the following stages:
- Inpatient period - begins from the moment of admission of the patient to the intensive care or intensive care unit, and further - to the cardiology or vascular department (clinic).
- Staying in a rehabilitation center or sanatorium - lasts up to 4 weeks after a heart attack.
- Outpatient period - involves outpatient follow-up by a cardiologist, rehabilitologist, LFK instructor (for a year).
Rehabilitation is then continued by the patient independently, at home.
The basis of successful rehabilitation is moderate and consistent physical activity, the scheme of which is developed by a doctor on an individual basis. After certain exercises, the patient's condition is monitored by a specialist and evaluated according to a number of criteria (the so-called "stress tests" are particularly relevant). [10]
In addition to physical activity, the rehabilitation program includes medication support, lifestyle correction (dietary changes, weight control, elimination of bad habits, monitoring of lipid metabolism). An integrated approach helps to prevent the development of complications and adapt the cardiovascular system to daily activities.
Transmural myocardial infarction is characterized by the most unfavorable prognosis, which is explained by the increased probability of mortality even at the pre-hospital stage. About 20% of patients die within the first four weeks after the attack.

