Medical expert of the article
New publications
Atherosclerosis of the heart vessels
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
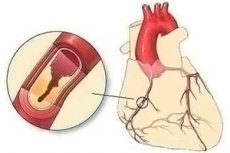
Atherosclerosis can affect arteries of various localizations, and coronary atherosclerosis - atherosclerosis of the vessels of the heart that supply oxygen to the heart muscle cells (myocardium) - is a long-lasting and constantly progressive disease of the cardiovascular system with multiple clinical manifestations.
Epidemiology
The coronary (or venous) arteries, along with the abdominal (abdominal) aorta, occupy the first place in terms of the frequency of atherosclerosis, ahead of the descending thoracic aorta and internal carotid arteries.
According to statistics, in persons with a latent form of this pathology, the prevalence of cardiovascular disease is more than 25%, which is twice as high as in its absence.
And, according to WHO, 50-60% of deaths in patients with cardiovascular disease are etiologically related to atherosclerotic lesions of the walls of the arteries of the heart. [1]
Causes of the atherosclerosis of the heart vessels
Atherosclerosis most often affects the proximal regions of the left and right epicardial arteries of the heart, which branch off the aorta and are located on the outer surface of the heart, providing coronary blood flow.
The main causes of atherosclerotic lesions are due to disorders of lipid metabolism, which lead to increased levels of LDL (low-density lipoprotein) cholesterol in the blood - hypercholesterolemia.
In this case, there is an accumulation of "bad" cholesterol in the inner lining of vascular walls (tunica intima) and subendothelial tissue in the form of atheromatous or atherosclerotic plaques. [2]
Read more in the publications:
Risk factors
The risk of coronary atherosclerosis is increased at age 45+; if blood relatives have the disease; dyslipidemia and diabetes mellitus; systemic arterial hypertension and obesity (which can lead to type 2 diabetes and arterial hypertension).
Other risk factors include smoking, sedentary lifestyle and eating foods high in saturated fat. [3]
Pathogenesis
The pathogenesis of atherosclerotic lesion of vascular walls, stages of atherosclerotic plaque formation, changes in arterial walls and the mechanism of inflammatory reaction of endothelial cells (with macrophage activation) are discussed in detail in the materials:
Symptoms of the atherosclerosis of the heart vessels
Cardiac atherosclerosis is a chronic progressive disease with a long asymptomatic phase during which atherosclerotic plaques form on the vascular walls. At this stage, defined as subclinical atherosclerosis, there are no symptoms. And the first signs appear when specific cardiac problems arise. [4]
The spectrum of symptoms corresponds to conditions such as:
- Heart attack (manifested by shortness of breath, cold sweats, chest pain, shoulder or arm pain);
- Stable angina pectoris - with heart rhythm disturbance, excessive fatigue, discomfort and a feeling of pressure in the chest during exercise, left-sided chest pains (which may radiate to nearby areas);
- Unstable angina with more frequent pain, periods of arrhythmia, shortness of breath and dizziness.
Minimal, mild or severe degrees of coronary artery atherosclerosis are defined depending on the size of atherosclerotic plaques, intima thickness of the vessel walls and the level of obstruction.
The right coronary artery (arteria coronaria dextra), which supplies blood to the right ventricle, right atrium, part of the cardiac septum, sinus atrial and atrioventricular nodes (which regulate heart rhythm), comes out of the right aortic sinus.Atherosclerosis of the right coronary artery, when its lumen is reduced, can manifest as heart attacks with palpitations and difficulty breathing.
The left main coronary artery (arteria coronaria sinistra), which supplies blood to the left ventricle and left atrium, is more susceptible to atherosclerosis due to anatomical features and local hemodynamic forces (the right coronary flow is known to be more uniform during the cardiac cycle). Most often, atherosclerosis of the left coronary artery means a lesion of one of its branches, in particular, the left anterior descending artery (anterior interventricular branch of the left coronary artery), which supplies blood to the anterior part of the left side of the heart.
Multiple atherosclerotic lesions of vessels - peripheral and carotid arteries - are defined as multifocal atherosclerosis. Its prevalence in patients with coronary artery atherosclerosis is estimated at 60%. [5]
As the coronary arteries continue to narrow, blood flow to the heart decreases and symptoms may become more severe or frequent. That is, stenotic coronary artery atherosclerosis develops with varying degrees of persistent narrowing of the vessel lumen caused by obstructive atherosclerotic plaques. [6]
Complications and consequences
Complications and life-threatening consequences of the progression of coronary atherosclerosis are:
- Insufficient coronary circulation and the development of IBS (Coronary heart disease and atherosclerosis of heart vessels have a causal relationship, as IBS is usually provoked by vasoconstriction, while their stenosis is caused by coronary atherosclerosis);
- Acute coronary syndrome (development of which occurs due to destruction of atherosclerotic plaque with acute coronary artery thrombosis);
- Myocardial infarction with ST-segment elevation.
Diagnostics of the atherosclerosis of the heart vessels
The gold standard for detecting coronary artery atherosclerosis is coronarography (coronary angiography) with contrast enhancement. But, because such coronarography visualizes only the blood-filled space of the vessel, it is difficult to detect other angiographic signs of coronary artery atherosclerosis, such aspresence of atherosclerotic plaques in the vessel wall, determine their number, assess their volume and composition (including the presence of calcification) - can only be detected by cT angiography (on multidetector CT scanners) or vascular MRI - magnetic resonance angiography.
Also instrumental diagnostics include electrocardiography (ECG), echocardiography (Echocardiography), chest x-ray, and intravascular ultrasound.
For laboratory tests, blood tests are taken: for total cholesterol, LDL, HDL-C, LDL-C, HDL-C, apolipoprotein B (Apo B), triglycerides; for C-reactive protein and for serum homocysteine levels.
A differential diagnosis with diabetic microangiopathy and coronary occlusion in systemic scleroderma is made. [7]
Treatment of the atherosclerosis of the heart vessels
Can atherosclerosis of the heart vessels be cured? Today it is believed that coronary atherosclerosis cannot be cured, because with the help of currently available means, the progressive process of atherosclerotic plaque formation cannot be completely reversed.
But treatment can help manage symptoms and reduce the likelihood of complications and consequences. For example, drug therapy for angina pectoris includes nitrates (Nitroglycerin), cardiac glycosides (Digoxin, Corglycone), calcium channel blockers (Nifedipine), and Propranolol hydrochloride (Anapriline) and other β-blockers. In addition, patients with symptoms of angina pectoris may be prescribed sedatives to reduce the production of endogenous catecholamines to avoid serious complications.
Today, the most available medications for atherosclerosis of the heart vessels include drugs to reduce atherogenic lipoprotein levels, primarily statins (Provastatin, Lovastatin, Simvastatin, Atorvastatin).
Reduces cholesterol absorption in the intestine Cholestyramine (Colestyramine) and some other pharmacologic agents for treatment of elevated cholesterol.
Bezafibrate (Bezamidine) and other pills for high cholesterol are also used.
Newer agents include the FDA-approved lipid-modifying drugs Alirocumab (Praluent) and Evolocumab (Repatha) of the PCSK9 inhibitor group, which provide reductions in low-density lipoprotein (LDL) cholesterol.
Treatment may include lifestyle changes such as regular exercise and quitting smoking. For more information, see. - atherosclerosis - Treatment
What vitamins to take in atherosclerosis of the heart vessels? Specialists recommend B vitamins, especially vitamin B3 (nicotinamide) and B15 (calcium pangamate).
For life-threatening stenosis of heart vessels, resort to coronary artery stenting.
Details about how the diet is needed for atherosclerosis of the heart vessels, as well as the approximate menu for atherosclerosis of the heart vessels, in publications:
And what foods are recommended for atherosclerosis of the heart vessels, read in the material - useful foods to strengthen the heart and blood vessels [8]
Prevention
To prevent coronary atherosclerosis, you should eliminate smoking; eat a healthy diet low in saturated fat, cholesterol and salt; lose excess pounds and maintain a normal body weight, as well as move more and exercise regularly. [9]
Forecast
It should be borne in mind that when atherosclerotic plaque clogs an artery, disrupting blood flow and causing blood clots, the prognosis for the outcome of the disease cannot be favorable, as atherosclerosis of the heart vessels can lead to cardiovascular disease with life-threatening consequences.

