Medical expert of the article
New publications
Reflux gastritis: biliary, superficial, chronic, erosive, atrophic, antral gastritis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
This is one of the forms of inflammation of the gastric mucosa, caused by a change in the flow of duodenal contents and its backflow into the stomach. The detergent components of the refluxate have a traumatic effect on the epithelium of the stomach, which ultimately leads to an inflammatory process, most often in the antral part of the stomach.
Epidemiology
The epidemiology of reflux gastritis is determined by the frequency of surgical interventions on the digestive organs, the use of pharmacological drugs, the prevalence of alcoholism and other risk factors for the development of duodenogastric reflux.
For example, duodenogastric reflux is a consequence of suturing a duodenal ulcer in 52.6% of cases, and cholecystectomy in 15.5%.
There is data that from a quarter of the population to 40% suffer from symptoms similar to duodenogastric reflux, but only about 5-7% of them seek help with such complaints. More than 50% of those who seek help have antroduodenal dysmotility, which is one of the causes of reflux gastritis.
The vast majority of episodes of chronic gastritis (about 80%) are associated with Helicobacter pylori infection, up to 15% are cases of autoimmune atrophic inflammation of the stomach, and only about 5% are due to special types of pathology, including reflux gastritis.
 [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
[ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
Causes reflux gastritis
This pathological condition is provoked by a disorder of the muscular function of the sphincter, which blocks the return of duodenal contents back to the stomach in a healthy person. Significant risk factors for the development of this condition are gastric resection, gastroenterostomy, cholecystectomy, pyloroplasty and other interventions on the digestive organs that lead to a pathological disorder of the coordination of motor skills and evacuation of contents in the digestive tract, chronic inflammation of the duodenum, its dyskinesia and hypertension, bacterial invasion Helicobacter pylori, gastroposis (prolapse of the stomach). Reflux gastritis may develop as a result of taking non-hormonal anti-inflammatory drugs. This is facilitated by treatment with some other drugs, for example, antibiotics or analgesics, iron- and potassium-containing drugs, and alcohol abuse. A rather important role in the mechanism of pathology development is given to the state of the nervous system - irritable, easily excitable people are considered more susceptible to this disease.
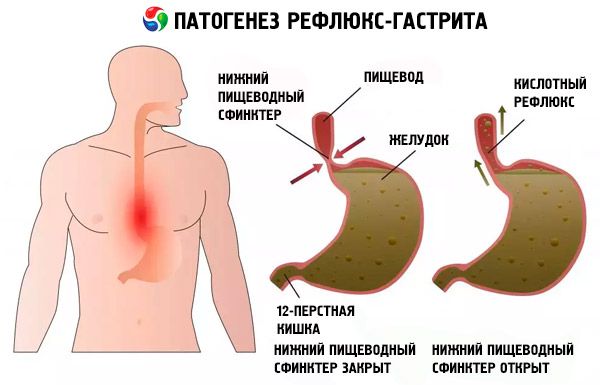
Pathogenesis
The pathogenesis of reflux in modern medicine is considered as follows:
- sphincter insufficiency, allowing the contents of the duodenum to freely bypass the antral and cardiac sphincters and return to the stomach and esophagus;
- antroduodenal discoordination – lack of regulation of the direction of movement of the food bolus in the duodenum;
- surgical removal of the stomach or part of it, which disrupts the natural barrier to the backflow of refluxate.
The contents that get back into the stomach contain substances that are aggressive to it – bile, its acids and salts, enzymes synthesized by the pancreas, lysolecithin, intestinal juice. It activates the secretion of gastrin (the number of cells producing this digestive hormone increases in the antrum), and in the presence of hydrochloric acid, it forces the dissolution of the fatty components of the cell walls of the gastric mucosa with a dense avalanche of hydrogen ions moving in the opposite direction.
Constant damage to the gastric epithelium by the contents of the duodenum causes dystrophy and necrobiotic transformation of its cells. In this case, only the epithelial surface of the stomach is affected, and the process is focal. This form of the inflammatory process is classified as chemical-toxic-induced gastritis (type C).
There is, however, a position that allows one to doubt the significance of duodenogastric reflux in the mechanism of development of inflammatory disease of the gastric mucosa. In fact, the epithelium of the stomach is very resistant to the action of bile and other components of the refluxate. Even prolonged exposure to duodenogastric reflux causes minor damage to its structure. Some clinicians consider the backflow of contents from the duodenum to be a protective reaction to the overproduction of hydrochloric acid or regulating the secretory activity of the gastric glands, i.e. substitution - in case of its insufficiency. The role of duodenogastric reflux is still in the process of controversy and study.
Symptoms reflux gastritis
The symptom complex of this form of inflammation of the gastric epithelium is often not commensurate with the degree of its damage established during the examination. Often, the obvious presence of this form of gastritis diagnosed for another reason can have an asymptomatic course.
However, with pronounced symptoms, the first signs that you should pay attention to are pain in the epigastrium or the appearance of a feeling of heaviness during or immediately after eating, the appearance of belching air, as well as the food eaten (regurgitation), heartburn, nausea, flatulence, the appearance of a repulsive bitter taste in the mouth, vomiting bile. Later, frequent constipation or diarrhea, a yellowish coating on the tongue, loss of appetite and weight loss may join in. Over time, dry skin, cracks in the corners of the lips (angular cheilitis), weakness and rapid fatigue are observed - this is how anemia and vitamin deficiency manifest themselves.
Pain syndrome in reflux gastritis is not a characteristic symptom, but some patients complain of intense burning pain localized in the upper abdomen. It usually appears periodically, is characterized by paroxysms and is often a consequence of physical exertion or emotional outbursts and stressful situations.
The symptoms described above may be accompanied by a cough, which is usually considered the prerogative of colds, but in practice it is often caused by gastroesophageal reflux. Cough with reflux gastritis is usually debilitating, it is not accompanied by a runny nose and sore throat. It is usually accompanied by other dyspeptic disorders, general weakness and malaise.
Acute reflux gastritis is not a very correct definition, since acute means inflammation of the gastric epithelium due to the impact of single intense irritants. Reflux gastritis develops due to constant irritation of the gastric mucosa by regular reflux of intestinal contents. In most cases, it is characterized by an asymptomatic course and is often discovered by chance. Therefore, when talking about reflux gastritis, we mean a chronic disease. If the endoscopist's conclusion refers to the acute stage of this disease, then, most likely, an exacerbation of reflux gastritis is implied.
Acute reflux gastritis developed, according to some authors, as a secondary condition in patients after operations on the digestive organs. In postoperative patients, with the development of reflux gastritis, infection with Helicobacter, polypous hyperplasia and peptic ulcers were often detected.
Chronic reflux gastritis occurs in waves, with long latent periods. Expressed (described above) symptoms correspond to the stage of exacerbation of this disease.
Moderate reflux gastritis may be asymptomatic or have mild symptoms, and may have only one symptom, such as heartburn, flatulence, or other dyspeptic symptoms. They may be persistent and debilitating. Moderate or severe reflux gastritis is a conclusion made after gastroscopy and says more about the degree of damage to the gastric mucosa. According to practicing gastroenterologists, the severity of symptoms in this form of the disease does not always correspond to the severity of damage to the gastric epithelium.
Forms
Bile is the most studied ingredient of refluxate. Its acids play the main role in the pathogenesis of this disease. Bile acids, which are surface-active substances, have the ability to dissolve the main lipid components of the cell membranes of the gastric mucosa, causing its damage. Pathologies of the biliary system in combination with antroduodenal dysmotility and insufficiency of the sphincter apparatus lead to regular reflux of intestinal contents saturated with bile acids into the stomach. Constant bile burns cause biliary reflux gastritis. There are no specific symptoms that allow one to distinguish it from other types of this pathology by clinical manifestations; most often, bile reflux manifests itself as belching and heartburn.
Morphological transformations of the gastric mucosa due to biliary reflux are increased proliferation of mucous cells on the surface of the stomach and, accordingly, epithelial proliferation, edema against the background of a moderate inflammatory process. The epithelial surface acquires a basophilic structure saturated with nucleic acids, with a practical absence of mucus. Epithelial cells undergo dystrophic changes (vacuolar degeneration, karyopyknosis), leading to the onset of necrobiosis and the formation of erosions, since the gastric glands located there stop producing protective mucus. This process can eventually develop into erosive reflux gastritis, which is manifested by bleeding from erosions and the presence of brownish and bloody streaks in vomit and feces.
Damage to the gastric mucosa caused by the reflux of duodenal contents is often provoked by inflammatory pathology and hypertension in the duodenum (reflux gastritis-duodenitis). Pathological changes can only be diagnosed using duodenogastroscopy, as well as biopsy analysis of the gastroduodenal mucosa. This type of gastritis does not have specific symptoms.
Catarrhal reflux gastritis (simple) – usually in this case we are talking about acute gastritis and superficial damage to the epithelium. With this type of disease, the mucous membrane swells, there is a possibility of spreading to its entire surface and dystrophic changes begin in it. Symptoms are usually pronounced, but without specificity.
Superficial inflammation localized in the pyloric part of the stomach, combined with muscular insufficiency of the sphincter between the stomach and the duodenum, leads to the fact that the food lump, abundantly flavored with hydrochloric acid, can uncontrollably penetrate into the intestine, burning its bulb and causing an inflammatory process in it, called bulbitis. The same sphincter insufficiency does not prevent the backflow of contents into the stomach. Such unimpeded passage of not fully processed food in one (correct) direction and its backflow ultimately ends with a diagnosis of reflux gastritis-bulbitis.
As already mentioned, the most frequent damage to the epithelium during the reflux of duodenal contents occurs in the antral part of the stomach (antral reflux gastritis). It is also called distal reflux gastritis, since this part of the stomach includes the antral part, the pyloric canal and the pyloric sphincter. This zone suffers the most from the reflux of refluxate and is the first to be affected. Focal reflux gastritis develops. If the disease is not diagnosed in time and treatment is not started, atrophic changes subsequently increase. Sometimes mixed reflux gastritis is observed, in which areas of inflamed, but still "working" surface of the epithelium are combined with zones of atrophy of the gastric glands - foci of hyperemic surface alternate with grayish areas of atrophy.
At the beginning of its development, non-atrophic reflux gastritis, focal and superficial, and even proceeding without pronounced symptoms, does not look like a very serious disease. The progressive process of proliferation and dysplastic changes lead to the fact that atrophic reflux gastritis develops in the future. The main distinguishing characteristic of this type of disease is the atrophy of zymogen and parietal cells in the deep layers of the gastric epithelium and their displacement by so-called pseudopyloric cells, which are unable to produce digestive hormones and sulfuric acid. Atrophic transformations of the gastric mucosa, in particular, colonic metaplasia, pose a risk of malignancy.
The same can be said about hyperplastic reflux gastritis, which is characterized by the proliferation of the gastric mucosa and the appearance of cystic, folded or polypous formations.
Erythematous reflux gastritis – this formulation indicates that gastroscopic examination has revealed redness of the mucous membrane. This is not a diagnosis, but rather a statement of fact that suggests the existence of gastritis or other gastric pathology. Additional studies are needed for a final diagnosis.
Complications and consequences
In fact, the types of any form of chronic inflammatory process in the stomach are stages or phases of a single course of the disease and reflect morphological changes in the process of its development. In conditions of regular damage to the epithelial surface of the stomach, the process of its restoration is disrupted. The renewed epithelium in chronic gastritis differs from the healthy one and ceases to perform natural functions. The development of the pathological process is a demonstration of dysregeneration of the gastric mucosa.
Negative changes occurring with the gastric mucosa are aggravated by untimely diagnosis and prolonged absence of treatment. The most unpleasant consequence of ignoring this pathology may be the development of a malignant neoplasm. The stages of development of atrophic and hyperplastic transformations of the epithelium are considered especially dangerous in this sense.
Diagnostics reflux gastritis
The assumption of the presence of reflux gastritis is made on the basis of the patient's complaints, his thorough examination and questioning, during which the cause of the disease is revealed. Particular attention is paid to people who have undergone operations on the digestive organs. Instrumental diagnostics allows confirming or refuting the presumptive diagnosis. According to the results of fibrogastroduodenoscopy, a focal inflammatory process is detected (usually in the antrum), often - edema of the epithelium, the shade of the stomach contents is yellowish. The inflammatory process in reflux gastritis is usually insignificant. The sphincter between the pyloric part of the stomach and the duodenum is dilated.
Currently, gastritis (duodenitis, esophagitis) is a histological diagnosis, so an accurate conclusion is given based on microscopy of biopsy specimens taken during fibrogastroduodenoscopy. When studying them, hyperplastic changes in the mucous membrane, plethora in the absence of significant inflammation, irreversible changes in cells and their death, and occasionally intestinal-type metaplasia are detected.
With the help of antroduodenal manometry or gastrography, the contractile activity and coordination of muscle contractions of different parts of the gastroduodenal zone are studied, pH-metry or a histamine (gastrin) test allows one to assess the level of acidity, contrast X-ray or daily pH-metry using Gastroscan-24 – the presence of duodenal reflux.
An ultrasound examination of the digestive organs is prescribed to identify concomitant pathologies and tests: blood, urine, feces.
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
Treatment reflux gastritis
The treatment process for this disease is aimed at achieving the following goals: restoring normal motor function of the digestive system organs and compensating for the destructive effect of refluxate on the gastric epithelium. Therapy for reflux gastritis includes medications from different pharmacological groups: stimulants of the digestive tract motility (prokinetics), inhibitors of acid production (antacids), derivatives of ursodeoxycholic acid (hepatoprotectors), cytoprotectors, enterosorbents, and proton pump inhibitors.
Primer (active ingredient – itopride hydrochloride) is a modern prokinetic of selective action, enhancing propulsive peristalsis of all organs of the digestive tract and preventing the development of duodenogastric reflux. The action of this drug is due to the stimulation of the release of endogenous acetylcholine and an increase in the time of its activity, which is achieved by inhibiting the activity of the enzyme acetylcholinesterase. This tones the muscles, including the sphincter muscles, leads to an increase in the duration of contractions of the smooth muscle tissue of the stomach and intestines, accelerates the movement of the contents of these organs in the right direction.
The active substance is absorbed (approximately 90%) in the intestine, the highest plasma concentration is recorded after ¾ hour from the moment of taking Primer. Absorption does not depend on food intake. The metabolism of this drug is carried out in the liver with the help of flavonoid monooxygenase without the participation of cytochrome P450, which makes it possible to avoid negative interactions when combining it with other drugs, the metabolism of which is carried out by enzymes of the CYP450 system. Primer has virtually no toxic effect on the liver, does not accumulate and does not pass through the blood-brain barrier. Inactive metabolites of the active ingredient are excreted in the urine, for complete excretion of one dose, ½ a day is enough.
The recommended single dose is 50 mg, taken every eight hours. The maximum permissible dose is 800 mg per day. The duration of treatment is from two to three weeks.
Not prescribed to pregnant and lactating women, aged 0-11 years, persons with bleeding, perforation, obstruction of the digestive organs, sensitization, elevated prolactin levels.
Hydrotalcite is a medicine used for increased acid production. The active ingredient of the same name is aluminum magnesium hydroxide carbonate hydrate - it neutralizes excess hydrochloric acid in the gastric juice, normalizes acidity and protects the epithelium of the stomach from the damaging effects of hydrochloric and bile acids. It has a layered mesh structure with a specific effect. The outer layer of the tablet containing the active ingredient comes into contact with the acid. As soon as the acidity decreases, the release of aluminum and magnesium stops until the next moment of its increase, when the next layer of the active substance enters into the reaction. This allows for a long time, compared to other antacids, to maintain the acidity of the gastric juice close to normal. In addition, hydrotalcite has sorbent properties, absorbing bile acids and lysolecithin. It is taken orally. It is dosed at 0.5-1 g with an interval of at least an hour after meals and at night, three to four times a day, for children over six years of age - 0.25-0.5 g. It interacts with some antibiotics and other drugs, so if combined administration is necessary, it is necessary to maintain a time interval of at least an hour. Contraindicated at the age of 0-5 years, in case of exacerbation of renal pathologies, sensitization to components, pregnant and lactating women.
Combination therapy with acid inhibitors is more effective than monotherapy with either drug.
For example, simultaneous administration with Rabeprazole. This drug with the same active substance inhibits acid production by reducing the enzymatic activity of hydrogen-potassium adenosine triphosphatase on the surface of parietal cells. The effect of the application depends on the dose and reduces both the basic and stimulated secretion of hydrochloric acid. It has slightly alkaline properties, is quickly absorbed and accumulates in the parietal cells. The effect of the drug is somewhat potentiated by daily intake of one tablet, a stable effect occurs on the fourth day of administration, after the end of therapy, acid formation is normalized after two to three days. It is metabolized using the cytochrome 450 system, which should be taken into account when prescribing drugs with a similar metabolism, does not interact with hydrotalcite. It has many side effects, with long-term treatment, the condition of patients must be monitored. Contraindicated in children, pregnant and lactating women, sensitized individuals. Prescribed in dosages from 10 to 20 mg, per day - once. The duration of treatment is from one to two months.
The use of therapeutic agents in the treatment regimen for reflux gastritis, the active component of which is bear bile (ursodeoxycholic acid), is based on its cytoprotective effect. It converts toxic bile acids into a hydrophilic form, the aggressiveness of the refluxate decreases. The clinical condition of the patient improves, endoscopic examination shows a decrease in the lesions of the epithelial surface of the stomach. The effectiveness of ursodeoxycholic acid derivatives in both reflux gastritis and Helicobacter-positive gastritis has been experimentally proven, which is important since the damaging effect on the mucosa with a combination of duodenogastric reflux and infection with this bacterium increases synergistically. These drugs also give a positive effect in the treatment of patients with operated digestive organs (stomach, gallbladder).
The drug Ursosan (synonyms Ursofalk, Ursachol, Holacid) has such properties. When taken orally, the active ingredient is well absorbed by the tissues of the digestive organs, combines with the sulfur-containing amino acid taurine and aminoacetic acid. Ursodeoxycholic acid accumulates in bile, the level of accumulation depends on the condition of the liver. The metabolism of the active ingredient of the drug occurs in the intestines and liver, it is excreted mainly with feces, a small part - with bile. Contraindicated in inflammatory processes in the biliary organs, chronic liver and kidney dysfunction, at the age of up to five years and in the first three months of pregnancy (in the remaining six - for vital indications). Not prescribed to nursing women. Patients of childbearing age must be reliably protected. The drug may cause side effects, most often from the digestive system, and affect the properties of other drugs, in particular, antacids, which contain aluminum and magnesium.
Ursosan is taken once a day, at night. Dosage and duration of the course are individual. The standard dose is calculated as follows: per kilogram of body weight - 10 mg of the drug. Treatment can last up to 12 months.
Treatment measures to eliminate duodenogastric reflux and regenerate the gastric mucosa include dopamine receptor antagonists, preferably Domperidone, as the safest drug in this group, which does not overcome the protective barrier between the blood and brain tissue and does not lead to motor dysfunction. It tones the muscles of the pyloric sphincter, stimulates gastric motility, accelerating the evacuation of the food bolus from it, normalizes the coordination of muscle contractions of the stomach and duodenum. The drug can be prescribed to pregnant and lactating women for vital indications. It is not prescribed to persons sensitized to it, in case of bleeding, perforation, obstruction of the digestive tract, elevated prolactin levels. It can cause a number of side effects and negatively interact with some drugs. It is available in the form of a solution, suspension, suppositories and tablets.
Dosage for adults: one or two tablets (for severe symptoms) three or four times a day before meals. Rectal suppositories from two to four units (60 mg each).
Dosage for children:
- solution (1%) - at the rate of one drop per kilogram of weight three to four times a day;
- oral suspension – 0.25 ml per kilogram of weight three times a day;
- ½ tablet twice daily for body weight from 20 to 30 kg;
- more than 30 kg – one tablet twice a day;
- for the age group 0-2 years, suppositories 10 mg - from two to four units;
- for the age group of two years and older, suppositories 30 mg - from two to four units.
The treatment regimen may include antibacterial drugs (if Helicobacter infection is detected), enzymatic agents and probiotics, depending on the symptoms and condition of the patient.
In chronic, especially untimely diagnosed protracted course of reflux gastritis, avitaminosis develops. Vitamins are not absorbed in diseased digestive organs, especially B vitamins, which participate in hematopoiesis. Their deficiency leads to anemia, manifested by fatigue, dizziness, nervous system and mental disorders. Deficiency of retinol (vitamin A) slows down regeneration processes, ascorbic acid - lowers the immune barrier. With increased acidity, vitamin E can be useful, which helps to reduce its level. All this is taken into account when prescribing a treatment regimen, the doctor can prescribe a course of individual vitamins or vitamin-mineral complexes, which must be taken according to the doctor's recommendations and the instructions attached to them.
Physiotherapy is also included in the therapeutic scheme, standard procedures are electrophoresis or phonophoresis with drugs. They are carried out to relieve pain and inflammation.
Amplipulse therapy restores muscle motility and has a beneficial effect on the gastric epithelium and secretory function.
Acupuncture activates the functions of the digestive organs by acting on them through active points on the human body.
UHF therapy (electromagnetic decimeter waves), UHF therapy (ultra-high frequency) – improve blood circulation, stimulate healing and eliminate swelling and pain.
It should be taken into account that physical therapy is contraindicated in case of erosive and ulcerative lesions and the presence of tumors.
Alternative treatment
Traditional medicine is very rich in recommendations for healing gastrointestinal diseases. However, you should not replace drug treatment with traditional methods. They can help in complex treatment and recovery of the body, but always after consultation with the attending physician.
Thus, folk treatment of heartburn, which is one of the main symptoms of reflux gastritis, consists of the following simple procedures:
- chew a small piece of calamus root and swallow, you can wash it down with water;
- take a teaspoon of calamus root powder and swallow it;
- drink a tablespoon in the morning and evening before meals of freshly squeezed celery root juice;
- Grind the roots, leaves and seeds of angelica, brew one pinch of powder with boiling water, drink like tea after five minutes.
Flaxseed helps well, a decoction of which coats the gastric mucosa and protects it from the damaging effects of refluxate. The recipe for making an infusion from it is usually published on the packaging box. For reflux gastritis, another method of preparation is recommended: pour a tablespoon of seeds with ½ a glass of cool water and leave until the seeds swell and mucus appears, then strain and drink before meals.
You can prepare a herbal mixture for the infusion: two tablespoons of flax seeds, the same amount of chamomile, one tablespoon each of calamus root powder, licorice, lemon balm leaves and plantain. Place two tablespoons of the herbal raw materials in an enamel bowl and pour in boiling water (400 ml). Simmer in a water bath for a quarter of an hour, let it brew for two hours, strain and bring the infusion to 400 ml with boiled water. Take ½ cup four times a day before meals.
Herbal treatment of this disease is not complete without chamomile. It is present in almost all folk recipes in combination with other herbs and as a monophytopreparation. Even Greenfield tea with chamomile, according to reviews, helps with gastritis.
However, chamomile (by itself) is recommended for gastritis with low acidity, as it stimulates the production of gastric juice. However, in combination with yarrow and St. John's wort, chamomile is recommended for use in the form of herbal tea from approximately equal parts of all these herbs. It is drunk in the morning and evening, adding light flower honey.
Traditional healers offer the following recipe for chamomile syrup: fresh flowers are placed in layers in a glass or enamel bowl, sprinkled with layers of sugar. The layers should be pressed thoroughly until the juice is released. Dilute a teaspoon of the strained syrup in ½ glass of water and drink three times a day. Do the same with dandelion flowers, only before drinking, dilute a tablespoon of the strained syrup in ½ glass of water.
For pain and bilious vomiting, infusions of fumitory are recommended: two tablespoons of the herb are brewed with 500 ml of boiling water, and infused under a lid for about an hour. Take at intervals of two hours until the symptoms disappear, then it is recommended to switch to tea made from yarrow, St. John's wort and chamomile. However, in addition to its choleretic properties, fumitory has the ability to increase the secretion of gastric juice.
Traditional medicine recipes have been used for a long time, when treatment was purely symptomatic, and no one knew about stomach acidity. The benefits of decoctions and infusions were determined empirically. Reflux gastritis is most often accompanied by increased acidity, although with a long course and atrophic changes in the gastric epithelium, acidity decreases with any form of gastritis. Therefore, before treating with folk remedies, it is a good idea to analyze your diagnosis, consult a doctor and take into account all aspects of your condition. Many recipes contain mixtures of herbs that enhance, and often neutralize each other's effects. The answer to the question: which herbs are prohibited for reflux gastritis - is ambiguous and depends on several components, in particular, on acid formation. For example, chamomile, fumitory, plantain, calendula, dandelion are recommended for gastritis with low acidity. However, they are also present in herbal mixtures recommended for high acidity. Their anti-inflammatory and antimicrobial properties, as well as vitamins, micro- and macroelements, essential oils, flavonoids and other useful things are also useful here. Peppermint has the ability to reduce acid formation, fireweed is used for any secretion, marsh cudweed activates gastric motility. Infusions of medicinal herbs have a milder effect than medications, their active components are quickly excreted and do not have a cumulative capacity. In short, they are universal.
Homeopathy, prescribed individually at a consultation with a practicing homeopath, can lead to a stable remission even in advanced cases, but for this you need to be patient, change your habits and food preferences. Classical homeopathy uses one drug for treatment, and only an experienced doctor can choose it correctly. After all, more than twenty drugs are used for reflux, including Baptisia, Bryonia, Chamomilla or the same medicinal chamomile, not bypassed by homeopaths. Many drugs are prescribed when certain symptoms predominate, for example, Conium is prescribed to patients with excessive acid formation, with a predominance of symptoms of heartburn, sour belching, frequent nausea, Kali bichromicum - with a feeling of heaviness in the upper abdomen, with decreased appetite and flatulence, Argentum nitricum - relieves severe stomach pain, Robinia - burning pain, severe heartburn, regurgitation, sour belching.
If it is not possible to visit a homeopath, you can, together with your doctor, choose complex preparations offered in a homeopathic pharmacy or a Heel brand preparation.
For example, Gastricumel-Heel, intended for the treatment of various dyspeptic disorders and inflammatory processes in the stomach. The complex remedy includes: Argentum nitricum, Arsenicum album, Pulsatilla, Nux vomica, Carbo vegetabilis, Antimonium crudum, the most popular remedies for digestive disorders and gastrointestinal tract. This drug can be used both independently, especially in the initial stages of the disease, and in combination with medications. A Gastricumel tablet is placed under the tongue 30 minutes before a meal or an hour after and dissolved until it dissolves. To relieve an acute attack, you can dissolve a tablet every quarter of an hour, but make sure not to take more than 12 pieces per day. Treatment is continued for two or three weeks. Repeated use is possible if prescribed by the attending physician. The drug can be taken from the age of three, expectant and nursing mothers - only under medical supervision. The development of allergic reactions cannot be ruled out.
In case of severe acute inflammation of the gastric mucosa, it can be combined with Traumeel C to speed up the recovery process. Traumeel is able to quickly stop the inflammatory process, swelling, pain, and hyperemia through the activation of its own immunity.
In case of dysfunction of the digestive organs, Gastricumel-Heel can be used in combination with Nux vomica-Homaccord drops, which eliminate the consequences of the undesirable impact of toxic substances on the gastric mucosa, tone its muscles and activate motility, not only of the stomach, but also of the entire digestive tract from top to bottom, eliminating the symptoms of dyspepsia.
Combination with Mucosa compositum is possible, especially in case of erosive and ulcerative lesions of the digestive tract mucosa, to enhance motility and normalize coordinated movements of organs, eliminate bleeding, and accelerate the regenerative process. If necessary, the combination is supplemented with Traumeel.
The dosage of the combined treatment is prescribed by the attending physician. If necessary, all these drugs can be combined with anti-Helicobacter therapy.
 [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ]
[ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ]
Surgical treatment
Surgical interventions for reflux gastritis are used extremely rarely. Emergency operations are performed in cases of bleeding that has opened due to erosive damage to the gastric epithelium. Indications for planned operations are tumor formations, non-healing ulcers and erosions, sphincter function disorders that do not respond to conservative treatment.
Diet for reflux gastritis
In the treatment plan for this disease, one of the main roles is given to dietary nutrition, without which achieving a positive result is simply impossible. Since treatment is most often outpatient, the patient independently organizes his own diet, based on medical recommendations. Organization of nutrition and the set of products used should help normalize intestinal motility and reduce acidity, not irritate the gastric mucosa and not provoke reflux. During an exacerbation, you can take table No. 1 as a basis with some adjustments, leaving the main principle - food should be cooked without frying and baking with a crispy crust, not fatty, not spicy, not hot and not cold, meals - fractional (≈ 5-6 meals per day, portions should be small). It is advisable to eat on schedule, food, if possible, should be freshly prepared. Do not rush during meals, you need to learn to chew food well. It is recommended to eat in the evening for the last time about two hours before going to bed.
The following are eliminated from the diet:
- drinks – containing alcohol, caffeine, mint, carbonated, kvass;
- any fried foods, smoked foods, pickles;
- cabbage soup, borscht, okroshka;
- products that cause fermentation and flatulence – beans, peas, cabbage, black bread and others;
- fatty foods (pastries, shortbread, puff pastries; dairy products, not low-fat even with a low fat content; fatty meats and poultry, fish, ice cream, chocolate);
- fresh bread;
- any canned goods and semi-finished products;
- hard-boiled eggs;
- decoctions - meat, fish, mushroom, rich vegetable;
- sour, unripe, fibrous fruits and berries; in the acute period, it is better not to eat vegetables and fruits without heat treatment at all;
- ketchups, hot sauces, mustard, horseradish, pepper, mayonnaise;
- salt – limited (no more than a teaspoon per day).
The easiest way is to make a menu for reflux gastritis for each day of the week, based on the list of permitted products, trying to ensure that the same dishes are repeated no more than twice. And stick to it, making some adjustments along the way. Basically, the patient's diet will include:
- well-cooked porridge (the “mash” option) made from buckwheat, oatmeal, rice, can be served with skim milk (occasionally, for variety, you can also use other cereals);
- pureed vegetable soups with the addition of cereals, minced meat is possible (but not in meat broth);
- boiled meat, minced or blended, steamed (stewed) cutlets, meatballs, soufflé from dietary parts - fillet parts of beef, turkey, chicken, rabbit;
- lean fish, steamed, boiled, stewed;
- puree of boiled, stewed or steamed vegetables; vegetable stews of well-steamed and chopped vegetables;
- non-sour low-fat cottage cheese and dishes made from it - lazy vareniki, casseroles; low-fat hard cheese (grated, later - sliced); fresh low-fat milk;
- eggs (no more than twice a week), soft-boiled, steamed omelettes, soufflés;
- stale wheat bread, crackers, biscuits;
- butter, vegetable oil, a small amount of sour cream (added to the dish);
- desserts in the form of jelly, soufflé, baked apples, marmalade, pastilles from the store (1-2 pieces a couple of times a week);
- compotes, jelly, herbal teas.
The daily diet can be composed as follows:
- in the morning it is best to eat porridge cooked in water or skim milk with a small piece of butter, you can add a soft-boiled egg or a meatball, wash it down with herbal tea (it is even better to drink the tea first and then eat);
- for a second breakfast, white bread toasts sprinkled with grated cheese and rosehip infusion are suitable;
- for lunch you can have pureed vegetable soup, boiled pasta with the addition of minced meat, or dried fruit compote;
- afternoon snack will consist of a baked apple, a glass of jelly and biscuits;
- for dinner you can have lazy dumplings, washed down with chamomile tea;
- An hour and a half before bed, drink ½ glass of milk with a biscuit or cracker.
 [ 47 ], [ 48 ], [ 49 ], [ 50 ], [ 51 ]
[ 47 ], [ 48 ], [ 49 ], [ 50 ], [ 51 ]
Recipes for reflux gastritis
Any dietary nutrition is based on cereals, the most suitable of which are buckwheat and oatmeal. They are rich in vitamins and minerals, are easily digestible, and promote rapid evacuation of intestinal contents. They can be eaten at least every day several times. Rice porridge is also quite digestible, you can make a slimy "smear" from it during an exacerbation by adding more water than necessary, however, the low fiber content is not very suitable for those patients who suffer from constipation. Other cereals can also be consumed, but less often, for example, once a week. Since reflux gastritis is usually accompanied by increased acid formation, you can have flaxseed porridge for breakfast. It is very easy to prepare: grind flax seeds in a coffee grinder, take three to five teaspoons of the resulting flour, pour boiling water, stirring until the consistency of fresh sour cream, add salt, cover with a lid and wait at least five minutes. Starting the day with this porridge, you will get the effect - two in one: nutrition and therapy.
Any porridge goes well with boiled minced meat (just mix), oatmeal - with berries and applesauce. In case of relapses of the disease - boiled or baked apples, when the condition improves - you can use raw - ripe and sweet (without skin).
Meat dishes are prepared from tender fillet parts, cleaned of skin and tendons. For example, you can make meatballs with buckwheat. Add an egg and raw, sorted and washed buckwheat to the minced meat, add salt, form meatballs. Put them in a single layer in a saucepan. Pour hot water almost to the top of the meatballs, add coarsely chopped onion, a tablespoon of sour cream, and salt to the water. Cover, put on the fire, simmer for about an hour on low heat or put in the oven for an hour (t=150°C).
- Fish cutlets: make mince from white fish of the cod family (hake, cod, white and blue), having removed its skin beforehand. Add an egg, onion and carrot chopped in a blender or on a fine grater, a little semolina (do not overdo it, the mince should be tender), salt. Let it stand for a while (20 minutes). You can cook cutlets in a steamer, or you can put them in a saucepan, add a little uncut onion, carrot, two tablespoons of vegetable oil, about two fingers of hot water on the bottom, salt the gravy and simmer in the oven or on the stove until done (≈30 minutes).
- Lazy vareniki: mix cottage cheese with egg and a little sugar, add flour so that the dough sticks together. Make small balls (3 cm in diameter) and cook them in boiling water. Serve with sour cream or butter.
Classic vareniki can be made from unleavened dough consisting of flour, water and salt (without eggs, as there are restrictions on this product). The filling can be cottage cheese, mashed potatoes, finely chopped peeled apples, and in summer – fresh berries.
- Jelly: make a rich compote from approved berries and/or fruits. Strain, dilute with instant gelatin or agar-agar in the proportion indicated on the package. Pour into bowls, cool - put in the refrigerator. Making jelly from store-bought bags with food coloring, flavor substitutes and preservatives is strictly not recommended.
- Stuffed beetroot: boil (bake) the beetroot, peel and remove the inside, shaping it into a cup, which is filled with a mixture, slightly sugared with the addition of 10g of melted butter, consisting of boiled rice, finely chopped peeled apples, finely chopped dried apricots (prunes, raisins - to taste and tolerance). Beetroot cups are poured with sour cream and baked in the oven. Can be served with sour cream.
More information of the treatment
Prevention
Prevention of inflammation of the gastric mucosa caused by duodenogastric reflux consists, first of all, in preventing the backflow of the contents of the duodenum. Not a very original idea, but first of all, you need to follow the rules of a healthy lifestyle, eat rationally, try to increase your stress resistance, do not get irritated and do not get nervous over trifles.
If, due to anatomical or other reasons, reflux periodically makes itself known, it is worth following simple rules. Firstly, get examined, because the earlier the treatment is started, the more effective it is. Secondly, you should adhere to the norms of dietary nutrition and give up bad habits.
Before eating, some nutritionists recommend drinking a glass of water to reduce the acidity of gastric juice. Avoid straining the abdominal muscles immediately after eating (do not bend over or lift heavy objects). Do not lie down to rest. It is much better to walk in this case. Do not wear tight underwear and clothing (pants, belts, skirts). The preferred sleeping position is semi-sitting (on a high pillow).
Forecast
This disease, as a rule, does not prevent a person from working and leading an active lifestyle, except for periods of exacerbation. However, in the case of a reasonable approach to the problem (timely diagnosis, treatment, appropriate lifestyle), the prognosis is quite favorable.
Long-term ignoring of symptoms, delaying seeking medical help, and failure to follow doctor's recommendations regarding diet usually results in complications, surgical interventions, and a serious deterioration in quality of life.

