New publications
Preparations
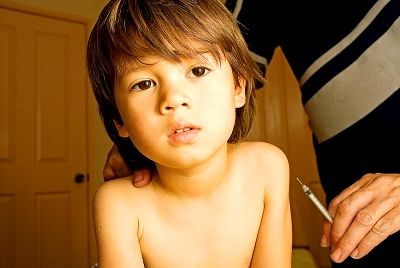
Pertussis vaccination

Pertussis in children of the first months of life is particularly difficult - with attacks of apnea, pneumonia, atelectasis (25%), seizures (3%), encephalopathy (1%). The pertussis vaccination performed in children in the coverage of more than 95% in Russia led to a decrease in the incidence from 19.06 per 100 000 population and 91.46 per 100 000 children under 14 in 1998 to 3.24 and 18.86 in 2005 and 5.66 at 34.86 in 2007, respectively.
However, pertussis in older children, adolescents, although often not diagnosed, constitutes an essential part of the incidence. In 2006, out of 7681 cases of pertussis in children aged 0-14 years (35.83: 100 000), 1170 cases were registered in children under 1 year old (79.8: 100 000), 878 at the age of 1-2 g ( 30,42: 100,000), 1,881 at 3-6 years (36,64: 100,000), and 2,742 at 7-14 years (72,8: 100,000), i.e. 1/3 of all registered cases fall on schoolchildren.
Incidence of whooping cough in a number of countries per 100 000 population
|
England - 0.5 |
Spain - 0.7 |
Austria 1.8 |
|
Iceland - 3.6 |
Malta - 3.7 |
Ireland -4.5 |
|
Italy - 6,1 |
Germany 10.1 |
Sweden - 22.3 |
|
Holland-32.7 |
Norway -57.1 |
Switzerland -124 |
|
USA - 2.7 |
Canada - 30.0 |
Australia - 22-58 |
In 1998 - 2002 years. In a number of countries, its maximum was for children under 1 year (Denmark 253.1 per 100 000, Switzerland - 1039.9, Norway - 172.5, Iceland - 155.3). The highest growth occurs in the age group over 14 years, the average age of pertussis cases in Europe has increased from 7 years in 1998 to 11 years in 2002 due to a decrease in the proportion of people aged 5-9 years (from 36% in 1998 up to 23% in 2002) with an increase in the proportion of people older than 14 years (from 16% to 35%). In the USA in 2005, 30% of all cases of whooping cough are registered in a group of people 21 years and older.
The true incidence of whooping cough is much higher than that recorded: a significant proportion of diseases of children and adolescents accompanied by a prolonged (more than 2 weeks) cough are due to whooping cough. Ill both partially vaccinated and properly vaccinated children, and it is obvious that immunity begins to weaken from the age of 5 years. According to new estimates, 600,000 adults suffer from pertussis every year - with a cough of 2-4 months and repeated calls to the doctor.
Long-coughing patients provide active circulation of the pathogen, pertussis causes 90-100% of susceptible persons who were in close family contact with the patient, the relative role of adolescents and adults has increased as sources of infection. For children, especially the first year of life; adolescents, according to the literature, are most often infected in school (39%), from friends (39%), family members (9%), and adults - from colleagues (42%), family (32%), friends ( 14%).
The current scheme of vaccine prevention of pertussis (3-fold vaccination and 1 revaccination) creates a high level of immunity, which decreases to school age. This is what prompted many countries to conduct the second revaccination in 5-11 years (Belgium, France, Germany, Spain, Portugal, USA, Japan, etc.), and Austria, Finland and Switzerland - also the 3rd revaccination in 11- 15 years. In England, only one revaccination is carried out - but at 3 years, in New Zealand - at 4 years, and in Denmark - at 5 years.
For booster vaccine in all countries, except Brazil, an acellular pertussis vaccine is used. It is obvious that in Russia it is necessary to introduce the 2nd revaccination.
In the second revaccination up to the age of 6 years, it is possible to use the acellular vaccine AaDS, but at a younger age, a reduced dose of diphtheria toxoid should be administered. Such vaccines (AaKdS) are created, but not registered in Russia: Bostrix (GlaxoSmithKline) for the age of 11-18 years and Ldasel (sanofi pasteur). They are administered and at a time from the previous dose of ADS (ADS-M) to 5 years.
Pertussis vaccines registered in Russia
| Anatoxin | Content, preservative |
| DTP - whole cell pertussis-diphtheria-tetanus vaccine - Micro Gene, Russia | In 1 dose (0.5 ml)> 30 MIU diphtheria,> 60 MI of tetanus toxoid, pertussis vaccine > 4 MZE. Aluminum hydroxide. Preservative of mercury |
| Infanrix (AaDS) - diphtheria-tetanus three-component acellular pertussis vaccine, GlaxoSmithKline, England | In 1 dose> 30 ME diphtheria,> 40 ME tetanus, 25 μg pertussis and filamentous hemagglutinin, 8 μg pertactin. Aluminum hydroxide 0.5 mg. Preservatives are 2-phenoxyethanol, formaldehyde up to 0.1 mg |
| Pentaxim (AaCDS + IPV + HIB) - diphtheria-tetanus-acellular pertussis-poliomyelitis and Hib vaccine, sanofi pasteur, France | In 1 dose> 30 ME diphtheria,> 40 ME tetanus, 25 mcg pertussis toxoid, 25 mcg PHA, 10 mcg Hib polysaccharide, D antigen poliovirus: 1st (40 units), 2nd (8 units), and 3 types 32 units). Aluminum hydroxide 0.3 mg. Preservatives are 2-phenoxyethanol (2.5 μl). Formaldehyde (12.5 μg). |
| Tetraczyme (AaCD + IPV) - diphtheria-tetanus-acellular pertussis poliomyelitis vaccine, sanofi pasteur, France (filed for registration) | |
| Infanrix-Penta (AaCDS + IPV + GeV) - diphtheria-tetanus-acellular pertussis-poliomyelitis and Hib vaccine, GlaxoSmithKline, Belgium (filed for registration) | |
| Infantriks-hexa (AaCDS + Hib + IPV + HepB) - diphtheria-tetanus-acellular pertussis-poliomyelitis, Hib and hepatitis B vaccine, GlaxoSmithKline, Belgium (filed for registration) | |
Vaccination against pertussis
Vaccination against whooping cough allows you to prevent more than 35 million cases of the disease and more than 600 thousand deaths annually in the world. However, the goal set by WHO in Europe - to reduce the incidence of whooping cough by 2010 to a level of less than 1 per 100 000 population - is unlikely to be achieved without the introduction of 2nd revaccination. It is also important to maintain a high level of coverage of young children, its decline led to an increase in the incidence in Russia in the 90s. In England, the reduction in coverage from 77% in 1974 to 30% in 1978 led to a pertussis outbreak with 102,500 cases. In Japan, in 1979, fourteen years after the end of the vaccinations (due to attacks on the whole-cell vaccine), 13,105 cases were reported with 41 deaths.
Postexposure prophylaxis of pertussis
For emergency prophylaxis of pertussis in unvaccinated children, a normal human immunoglobulin can be used - twice with an interval of 24 hours in a single dose of 3 ml at the earliest possible time after contact with the patient. More effective chemoprophylaxis with macrolide at age doses for 14 days (azithromycin - 5 days); 16-member macrolides should be used in neonates (Wilprafen Solutab, Macropen, Spiramycin), since 14- and 15-membered can cause them pyloric stenosis.
The vaccination against pertussis is not carried out by contact non-vaccinated children, in part vaccinated children continue to be vaccinated according to the calendar. If the child received a third dose of DTP for more than 6 months. Back, it is expedient to conduct a revaccination.
Contraindications and vaccinations against pertussis in children with chronic diseases
Strong reactions and complications, known hypersensitivity to any component of the vaccine or hypersensitivity to the previous dose of this vaccine are contraindications to the administration of the same pertussis vaccine. Progressive diseases of the central nervous system - a contraindication for DTP and vaccine Pentaxim, afebrile convulsions in the anamnesis - for DTP. For infanix vaccine, contraindication is encephalopathy, which developed within 7 days after the previous administration of this vaccine.
If a strong reaction or complication develops into a whole-cell pertussis vaccine, vaccinations can be continued with acellular vaccines or toxoids. If the child gave a strong reaction to the first injection of DTP, in the absence of an acellular vaccine, the vaccination against diphtheria and tetanus vaccination continues with ADS, which is administered once, not earlier than 3 months; after the 2nd dose of DTP, the course of vaccinations against diphtheria and tetanus is considered complete, in both cases the first revaccination is performed by ADS after 12 months. After the last inoculation. After the third DTP vaccination, revaccination is performed by ADS after 12-18 months.
Children with less severe CNS pathology should be vaccinated with acellular pertussis vaccines if there are concerns about the administration of DTP. Prematurity, stable allergic manifestations (localized skin, hidden or moderate bronchospasm, etc.) are not contraindications to vaccination, which can be performed against the background of appropriate therapy. Children with febrile convulsions, vaccination against whooping cough is carried out against the background of antipyretic.
Reactogenicity of pertussis vaccination
After vaccination against pertussis, fever may occur in the child (in predisposed children with febrile seizures), malaise, soreness, congestion and swelling at the injection site are not uncommon. The appointment of paracetamol 2-3 hours after vaccination and the next day prevents a sharp rise in temperature and convulsions.
Reactogenicity of Infanriks with respect to temperature, local soreness and redness, as well as irritability, drowsiness and decreased appetite is lower than that of whole-cell vaccines, which allows using it in children with disabilities in health status.
In rare cases, allergic reactions may develop ( Quincke's edema, urticaria, polymorphic rash), mainly to repeated doses of LDCA, more often in children who have similar reactions to previous doses; it is advisable for such children to prophylaxis antihistamines. However, the opinion about the "allergic" effect of DTP is not supported by studies conducted by different methods: vaccination did not increase neither the frequency of asthma nor eczema. Moreover, there is evidence of the protective effect of whole-cell pertussis vaccine on the incidence of asthma and, to a lesser extent, eczema.
A shrill cry (screech) for 1-3 or more hours after grafting was associated with an increase in intracranial pressure; Now the opinion prevails that this is the result of a pain reaction to the injection, it does not leave any consequences.
To excessively strong general reactions include hyperthermia (40 ° and above), for local reactions - dense infiltrates more than 8 cm in diameter, severe hyperemia of the skin with soft tissue edema at the injection site (sometimes the entire buttock with the transition to the hip and lower back). Such reactions have been rare in recent years.
Complications after pertussis vaccination
The data from the all-Russian registration disprove the opinion about the high incidence of complications in DTP: for the 6 years (1998-2003), only 85 reports of DTP side effects were submitted, of which only 60 have been confirmed. There were no lethal cases after DTP for the last 10 years.
Anaphylactic shock develops in a few minutes after inoculation, less oftenafter 3-4 hours. In children of the first year of life, the equivalent of anaphylactic shock is a kolaptoid state: a sharp pallor, lethargy, adynamia, a drop in blood pressure, less often cyanosis, cold sweats, loss of consciousness. Bronchial obstruction, croup after the introduction of DTP, is usually due to ARVI.
Afebra cramps with loss of consciousness, sometimes in the form of "pecks", absences, gaze stopping are observed with a frequency of 1: 30-40 thousand vaccinations and are often incorrectly designated as an encephalic reaction. This is usually the first manifestation of epilepsy, but it is difficult to deny its association with grafting as a trigger.
Encephalopathy (an encephalic reaction) is characterized not only by the presence of convulsions, but also by a disturbance of consciousness and / or behavior for more than 6 hours, as well as the appearance of slow waves on the EEG. It is observed much less often than isolated febrile seizures, its prognosis is favorable.
Encephalitis in the post-vaccination period is extremely rare (1: 250-500 thousand doses of vaccine), usually it is a case of a disease in the first few days after vaccination, taking place with hyperthermia, vomiting, convulsions, loss of consciousness, hyperkinesia, development of automatisms, paresis, other focal symptoms, usually with gross residual effects. Now these cases are deciphered as having no connection with the vaccination of the CNS disease (infectious meningoencephalitis, hereditary leukodystrophy, etc.), the initial manifestations of which coincided with it in time. Of the 4 reports on encephalitis after DTP in 1997-2002, there were 3 cases of viral encephalitis, 1 case of pneumonia with edema of the brain.
Preparations for vaccination against pertussis
Whole-cell vaccines containing all components of the microbial cell are recommended by WHO as the main means of preventing pertussis. In a number of developed countries acellular (acellular) vaccines are used, which are deprived of the lipopolysaccharides of the bacterial membrane causing the reactions. All vaccines are stored at 2-8 °, after freezing it is not applicable. Buba-Kok.
Acellular pertussis-diphtheria-tetanus vaccine Infarriks (AaCD) is well known to pediatricians, since the registration (2004) in Russia, more than 1 million doses of vaccine have been used. The vaccines of the Infanriks family are registered in 95 countries, total 221 million doses were used. It contains three 3 antigens of B. Pertussis: pertussis toxin, filamentous hemagglutinin and pertactin; its high immunogenicity and low reactogenicity makes it possible to increase immunization coverage by vaccinating children with contraindications to whole-cell DTP.
In 2008, the Pentaxim vaccine was registered in Russia, it contains, in addition to diphtheria and tetanus toxoid, increased IPV, Hib and 2 components of acellular pertussis vaccine. Pentaxim is registered in 71 countries of the world and is included in the calendar of 15 countries of Europe and a number of countries on other continents. The immunogenicity of this vaccine corresponds to that given by the separate administration of vaccines, it remains at a good level and at the age of 5 years. For example, in Sweden, in counties where only the Pentaxim vaccine was used (according to the scheme 3-5-12 months), its effectiveness against pertussis was 91% after 2 doses and 99% after 3 doses.
All vaccines are injected deep into the external muscle of the thigh at a dose of 0.5 ml according to the Calendar - at the age of 3, 4 "6 and 18 months.
Immunity after vaccination against pertussis
A full course of vaccination against whooping cough with whole-cell vaccine provides protection, especially from severe pertussis to 80% of vaccinated, from diphtheria and tetanus - more than 95% of vaccinated. The protective effectiveness of the Infranix vaccine is comparable, the presence of pertactin in it is important for maintaining a high degree of immunity to whooping cough. Immunity to whooping cough with all vaccines is reduced after 5-7 years, which justifies the second revaccination.
In the literature, the question of comparative immunogenicity of acellular vaccines with different number of components was discussed. In one study comparing studies performed before 2001, it was shown that 1-2-component vaccines had an efficacy of 67-70%, and those containing 3 or more components 80-84% with efficacy of whole-cell vaccines 37-92% . These findings were criticized, since the experimental 2-component vaccine was included in the comparison, which was later withdrawn from production. Several of the 2-component vaccines analyzed by the authors were subsequently licensed in countries such as Sweden, Japan, and France and have been successfully applied since. In response, the authors recognized that the lower immunogenicity of the 2-component vaccines is indeed related to the inclusion of data on the experimental vaccine and that, when it is excluded, there is no difference in immunogenicity, depending on the number of components.
The point in this discussion was recently published by Vidor E. And Plotkin SA. Data on 2-component vaccines, obtained by 75 groups of researchers in 36 projects in different countries in 1987-2006, showed their high efficiency, including in comparison with whole-cell vaccines. It should be noted that comparisons of the effectiveness of vaccines, including those with a different number of components, by national immunization regulators are considered illegal if these vaccines have been tested and registered for use in the country. At the same time, the main trend in improving the effectiveness of pertussis vaccines is the development of drugs with 3-5 components.
