Medical expert of the article
New publications
Myofascial pain syndrome: face, cervical, thoracic, lumbar spine
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Anyone who has ever encountered small lumps in the muscles that cause unbearable pain when pressed, of course, knows what myofascial syndrome is and would not advise anyone to encounter something similar in their life. Although the diagnosis may have sounded completely different. For example, myofasciitis, myogelosis or myofibrositis, pelvic floor muscle syndrome or muscular rheumatism, etc., etc.
True, the above-mentioned names, applied to the same pathology, do not quite correctly reflect the essence of the problem. After all, tension and pain in the muscles with myofascial pain syndrome are associated not with structural changes in the muscles, but with their dysfunction. Therefore, it would be more correct to call this pathological condition painful muscular-fascial dysfunction.
 [ 1 ]
[ 1 ]
Epidemiology
Statistical studies of chronic pain in the human body give us a clear picture of the prevalence of muscle pain, which is also characteristic of myofascial syndrome. According to various sources, from 7.5 to 45% of the population suffers from chronic pain of various localizations on the planet.
About 64-65% of patients complain of muscle pain in the back, neck, arms and legs, which are considered the most common after headaches. But two thirds of this number are patients with myofascial syndrome.
Muscle pain is most common in old age, but older people complain of muscle pain less often; pain and limited mobility in the joints come to the forefront.
In addition, it is believed that women are somewhat more susceptible to pain than men (especially at a young and mature age), so they often come to doctors with this problem and note a higher intensity of pain compared to men. Moreover, labor pains and discomfort during menstruation are not taken into account.
Causes myofascial syndrome
Despite the fact that the pain is felt in the muscles, the pathology is actually neurological in nature. After all, the cause of muscle spasm is a signal coming from the central nervous system.
When the body is healthy, the muscles receive a correct chain of signals that promote regular contraction and relaxation of muscle fibers. However, some health pathologies can interfere with the normal passage of the signal, and the muscles can remain in one position for a long time.
A prolonged relaxed state of muscles prevents them from performing their motor function, but muscle spasms can cause severe pain syndrome, which is called myofascial (MFPS).
The following diseases can cause the development of myofascial syndrome:
- Osteochondrosis of the spine. The localization of pain depends on the location of the spine section where degenerative-dystrophic changes are observed. Thus, cervical osteochondrosis provokes pain syndrome in the neck, back of the head, collarbones, shoulder girdle, arms. But pathological changes in the spinal column in the sternum and lumbar region cause pain similar to renal colic, attacks of angina pectoris or painful manifestations of the acute stage of pancreatitis.
- Dystrophic or inflammatory changes in the joints with localization of muscle pain in the same area as the damaged joint.
- Diseases of organs located inside the chest or abdominal cavity: heart, kidneys, liver, ovaries, etc. In this case, there is a reflex mechanism to protect the affected organ, due to which the muscles nearby are in a tense state. Plus, the pain associated with the underlying pathology forces a person to take a forced position in which it becomes a little easier. This again causes overstrain of certain muscle groups.
- Congenital and life-long skeletal defects. The difference in the length of the left and right legs is more than 1 cm, scoliosis, flat feet, asymmetry of the pelvic bones and other pathologies of the musculoskeletal system can cause severe tension in individual muscles, especially when walking.
- Various inflammatory diseases with edema syndrome, resulting in compression of nearby nerves, which worsens the conduction of nerve impulses.
- Intoxication of the body caused by a long course of taking certain groups of drugs (cardiac glycosides and antiarrhythmic agents, calcium antagonists and β-blockers used to treat cardiovascular pathologies, anesthetics such as lidocaine and novocaine).
- Pathologies of the neuromuscular system (myopathy, myotonia, etc.).
- Rheumatic pathologies characterized by systemic inflammation of connective tissue (fascia): lupus erythematosus, erythematous dermatitis, rheumatoid arthritis, polyarthritis, etc.
Risk factors
Risk factors for the development of MFBS are:
- bad posture,
- Uncomfortable clothing and accessories that contribute to the compression of nerves and muscle tissue,
- excess weight,
- sedentary lifestyle,
- "sedentary" work, prolonged stay in a static position at the computer,
- nervous tension, susceptibility to stress, sensitivity,
- consistently heavy physical labor,
- professional sports (especially while taking drugs that stimulate muscle growth),
- infectious diseases,
- tumor processes,
- dystrophic processes associated with the aging of the body,
- soft tissue injuries,
- hypothermia, frequent exposure to drafts (especially physical labor in adverse weather conditions),
- forced long-term restriction of motor activity as a consequence of injuries or operations.
Pathogenesis
Our body is a complex mechanism, the motor activity of which is provided by the musculoskeletal system, which includes bones, tendons, muscles, fascia (connective tissue surrounding the muscle). Movements of the arms, legs, body, facial expressions, breathing, talking - all this is possible only thanks to muscles.
Any movement is based on the ability of muscles to contract. And these are not chaotic contractions, but systematized with the help of the central nervous system. The impulse for the muscles to work comes from the brain.
If everything is in order in the body, the neuromuscular system works without failures. But under the influence of the above factors, the transmission of nerve impulses can be disrupted, either complete relaxation of the muscles (paralysis) or overstrain (long-term spasm) of the muscles occurs, accompanied by severe pain. It is against the background of excessive muscle tension that myofascial syndrome is observed.
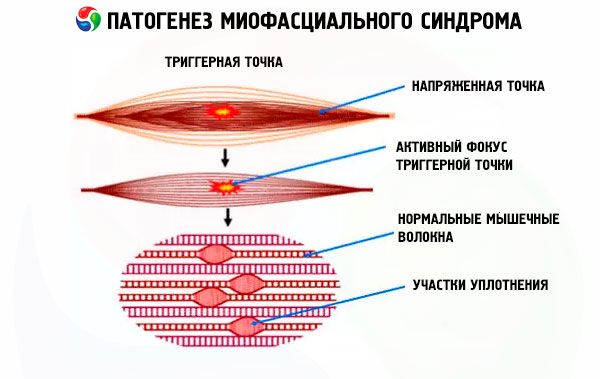
In the thickness of the muscle exposed to the negative influence of provoking factors, a small seal is formed near the motor nerve, which is characterized by increased tone even when the other parts of the muscle are relaxed. There can be one or more such seals, formed in the area of one muscle or in a certain part of the body. These seals are called trigger points, which in myofascial syndrome are associated with pain.
The mechanism of formation of such compactions of muscle tissue has not been thoroughly studied. However, scientists have clearly determined that compactions are nothing more than spasmodic tissue, structural changes in which (such as inflammatory processes or proliferation of connective tissue) can appear only at a certain stage of pathology, not being the true causes of muscle spasms and pain.
 [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ]
[ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ]
Features of trigger points in myofascial syndrome
The appearance of dense nodules of muscle tissue is a distinctive feature of myogelosis, which is characterized by the development of myofascial syndrome. Nodules, or trigger points, are unlikely to be seen during an external examination, but they are perfectly recognizable during palpation, noticeably standing out against the background of the rest of the muscle tissue, even if it is in a tense state.
Some nodules are located closer to the skin, while others are located in the deep layers of muscles (such trigger points can only be felt when the muscle is relaxed).
In addition, trigger points in myofascial syndrome can be both active, accompanied by severe pain both when pressed and at rest, and passive (latent). Latent points are characterized by pain sensations of lesser intensity, appearing only when pressing on the nodule or with strong muscle tension.
As strange as it may sound, despite the pronounced pain, active trigger points are not always easy to detect. The thing is that they are characterized by reflected pain, radiating to different parts of the body along the muscle in which the point is located, which is the source of pain. Diffuse pain does not allow you to determine the exact location of the trigger point, so sometimes you have to palpate the entire muscle.
When pressing on an active point, doctors often encounter the so-called "jump effect", when the patient jumps up from the spot due to severe pain. Sometimes the pain is so strong that the person may lose consciousness.
However, there is some benefit from these points. They prevent excessive stretching of an already injured muscle and limit its contractile function until the effects of the negative factors are eliminated.
For more numerous latent points, such intense pain is not typical. However, passive points under the influence of unfavorable factors tend to become active with symptoms typical for this group of triggers.
Symptoms myofascial syndrome
The first signs of myofascial syndrome of any localization are pains of varying intensity, increasing with tension of the affected muscle or pressure on the trigger point. Where to expect pain depends on the location of the trigger points, as well as the size of the affected muscle. After all, the pain will not always be localized, reflected pains can be felt along the entire length of this muscle.
Myofascial pain syndrome (MPS) can be divided into several types depending on the localization of the muscle with motor dysfunction. At the same time, localized and reflected pains, depending on the type of MPS, can be accompanied by other unpleasant symptoms.
Head and face
Myofascial pain syndrome in the facial area is a pathology with a fairly wide range of symptoms. In addition to dull, diffuse pain, it is characterized by multiple symptoms that force patients to seek help from various doctors: ENT, neurologist, dentist.
Patients may complain of difficulty opening the mouth, clicking in the temporomandibular joint, rapid muscle fatigue when chewing food, pain when swallowing. The pain sensations themselves may spread to the gums, teeth, pharynx, palate, and ears.
Less often, when diagnosing myofascial syndrome, patients complain of symptoms such as more frequent blinking, nervous tics in different parts of the face, congestion in one or both ears, occasionally accompanied by noise or ringing in them.
Sometimes, increased sensitivity of teeth is also noted. This is the problem that myofascial syndrome is known for in dentistry. However, the rest of the symptoms indicate not only the neurological nature of the pathology, but also that the main cause is still hidden in muscle dysfunction.
In this pathology, trigger points can be found in the area of the masticatory muscles, the pterygoid processes of the sphenoid bone on both sides of the nose, in the area of the temporomandibular joint, and also in the upper part of the trapezius muscle (radiating pain in the temporal region).
Neck and shoulders
Cervical myofascial syndrome also begins with pain, which can be localized in the neck or back of the head, or spread to the head, face, and forearms. At the next stage, vegetative-vascular disorders join them: dizziness, visual and hearing impairment, ringing in the ears, fainting. A "causeless" runny nose and increased salivation may also appear.
Although in most cases trigger points for cervical myofascial syndrome are located primarily along the cervical spine and upper shoulder girdle, isolated foci of tension can also be found in the area of:
- scalene muscles,
- oblique and splenial muscles of the head (burning pain in the back of the head and eyes, autonomic disorders),
- middle section of the sternocleidomastoid muscle (pain on one side of the face, accompanied by lacrimation, increased salivation, rhinitis),
- in the area of the shoulder blades or collarbone,
- upper parts of the trapezius muscle (throbbing pain in the temples),
- pectoral and subclavian muscles.
About half of patients with this pathology suffer from various sleep disorders, psycho-emotional disorders, and report decreased performance. About 30% developed panic attacks.
Rib cage
The occurrence of severe chest pain is most often associated with heart disease, and in particular with myocardial infarction. However, diagnostic studies do not always confirm this. The cause of chest pain may be the formation of seals in the muscles of the anterior chest, and then we are talking about a certain type of myofascial syndrome of the thoracic region called anterior chest wall syndrome. It is characterized by dull aching pain, most often on the left side of the sternum, intensifying when turning the body, lifting weights, spreading the arms to the sides, coughing.
Despite the fact that with such localization of trigger points the symptoms are mainly limited to chest pain, the appearance of painful foci may be a consequence of some diseases of the chest organs or even the back, which in itself is a reason to undergo an examination at a medical institution.
Another type of thoracic myofacial syndrome is the syndrome of the small pectoral muscle with localization of trigger points in its thickness. It is characterized by pain in the subclavian region, which can radiate to the shoulder or left arm. The pain is often accompanied by the appearance of goosebumps and temporary loss of sensitivity of the limb.
Back
Myofacial syndrome in the back muscles develops against the background of the appearance of painful nodules in the muscle running along the thoracic spine, in the latissimus dorsi, in the rhomboid and infraspinatus muscles. The location of the pain in this case is the area between or under the shoulder blades, as well as above the shoulders.
In this case, the pain is acute and occurs suddenly, especially when the muscles are overexerted or overcooled.
Myofascial syndrome of the lumbar spine is characterized by pain in the lower back, which can spread to the groin or sciatic nerve. Pain in the lower back can be caused by disc herniations, osteomyelitis, diseases of the digestive system, and even cancer that has metastasized to this area. But most often it comes down to muscle strain during heavy physical exertion (for example, lifting weights) or to displacement of the vertebrae in the lumbar spine.
If measures to treat underlying diseases are not taken in time, trigger points form in the lumbar region, which provoke excruciating pain syndrome.
Pelvic area and thigh
The symptoms of myofascial pelvic syndrome are more reminiscent of the symptoms of intestinal or genitourinary pathologies. Sometimes complaints boil down to the fact that the patient begins to feel as if there is a foreign body in his intestines. Painful sensations arise when walking or when a person does not change his sitting position for a long time. Localization of unpleasant sensations is mainly in the lumbar region or lower abdomen.
Many patients report increased urination. Women may also report discomfort in the area of the internal genitals and anus.
All these symptoms make people turn to a gynecologist, urologist, andrologist, who make the appropriate diagnoses: cystitis, prostatitis, urethritis, adnexitis, etc. Long-term examinations and treatment according to the above diagnoses remain unsuccessful until doctors manage to find out the true cause of discomfort and pain in the pelvic area.
But everything turns out to be much simpler, and pain in the pelvic area is provoked by a spasm of the muscles that hold organs such as the bladder, rectum, uterus, and in women, etc., located in the small pelvis. Depending on which muscle is affected (m.piriformis, m.levator ani, m.obturatorius int or superficial muscles), pain can be localized in different parts of the pelvis and radiate to the thigh.
Thus, with piriformis syndrome, pain in the buttocks and back of the thigh is accompanied by discomfort when walking and having sex, pain during defecation and unpleasant aching pain in the rectum and perineum that occurs with the slightest tension in the perineal muscles.
Internal obturator muscle and anal muscle syndrome, sometimes called urethral myofascial syndrome, is characterized by pain in the vagina, anus, or urethra, frequent painful urination, difficulty passing stool, and lower abdominal discomfort, especially when sitting.

Myofascial syndrome in children
Severe muscle pain in childhood seems to be something out of the ordinary, however, this problem is much more urgent than it may seem at first glance. Yes, chronic pathologies in children with myofascial syndrome are unlikely to be detected. But in this case, the emphasis is not on them, but on birth injuries to the spine and, in particular, its cervical region.
Slightly less than a third of newborn children have spinal cord injuries associated with the period of the child's birth, i.e. the passage of the fetus through the birth canal. More than 85% of such children receive various injuries to the cervical spine. About 70% of infants with various spinal injuries are diagnosed with myofascial syndrome.
In older children and adolescents, myofascial pain most often occurs either as a result of muscle hypothermia with subsequent spasm and formation of trigger points, or as a result of poor posture (scoliosis and other similar pathologies). Muscle pain is often provoked by the mobility typical of children and insufficient care for their health. As a result, we have a pain syndrome associated with injuries to the neck, spine and hip joint or muscle hypothermia, when a child, after active games with increased sweating, is in a draft or in an insufficiently heated room for some time.
Cervical myofacial syndrome in children most often manifests itself as headaches, pain in the eye area, dizziness, loss of balance. Injuries to the shoulder girdle and spine manifest themselves as pain in the back and upper limbs, and injuries to the hip and knee joints - pain under the knee, in the shin area, in the anterior and outer thigh, in the groin.
Complications and consequences
Muscle pain, despite all the unpleasant sensations, does not seem to be a dangerous condition to many patients. The opinion that by getting rid of its cause, you can solve all the problems in one fell swoop is gaining more and more popularity, and people prefer not to complete the treatment or not to resort to it at all.
Sometimes this approach to the problem, especially at the beginning of the disease, gives good results. No cause – no pain. But in advanced cases, when there is already a pronounced myofascial syndrome with its characteristic point compaction of muscles and fibrous changes occurring in them, its consequences can hardly be called safe.
Complications of myofascial syndrome can be considered not only structural changes in muscles, contributing to the chronicity of the process. The very fact that muscle tension over a long period of time leads to the accumulation of lactic acid in them, which prevents normal metabolism in the body's tissues and causes their oxygen starvation, cannot but be alarming.
Severe cases of myofascial syndrome with the gradual formation of several trigger points can eventually lead not only to psychoemotional deviations associated with sleep disorders and constant pain, or impaired ability to work. There are frequent cases of compression of nerves and blood vessels by the affected muscles, which increases the pain syndrome and leads to circulatory disorders with the consequences that follow from this situation.
Diagnostics myofascial syndrome
Complaints of muscle pain can be associated with various reasons. And only by understanding the cause can you prescribe the appropriate treatment for the situation. And since myofascial pain syndrome is a symptom of many serious diseases, diagnosing these diseases is a matter of honor for a doctor.
Diagnostics begins, as usual, with examining the patient and collecting anamnesis. Perhaps, by the time the pain appeared, the patient himself already knew about the presence of some diseases, which he can tell the doctor about. Having information about chronic pathologies in the patient's body, the doctor can preliminarily determine the possible cause of the pain and start from it in further studies.
When examining a patient, the doctor pays special attention to palpation of the sore spot. To determine trigger points, the muscle in the area of localization of pain is stretched lengthwise and palpated. A cord-like strand is felt under the fingers. Trigger points or seals should be looked for exactly along this "cord". Pressing on the muscle nodule during palpation causes severe pain, from which patients jump up or scream. This indicates that the trigger point has been found correctly.
In searching for cords and trigger points, the physician may probe deeply into the muscle by moving the fingertips across the fibers or by rolling the muscle between the fingers. During palpation and communication with the patient, pay attention to the following:
- Is there a connection between the onset of pain and physical exertion or muscle hypothermia?
- Is there atrophy or other changes in the muscles, indicating, for example, the inflammatory nature of the pathology?
- Are there any nodular lumps in the muscles or is there just general muscle tension?
- Is the pain localized or does it radiate to other places?
- Does pressure or puncturing of muscle nodules contribute to referred pain?
- Is there a jumping symptom?
- Does massage or heat reduce the intensity of pain?
- Do symptoms go away after muscle block?
Among other things, the doctor pays attention to how the patient tolerates pain, how he or she feels about his or her condition, whether there are sleep disturbances, and whether there are signs of depression.
To exclude the inflammation factor, blood and urine tests are performed. They will also help prescribe safe treatment. Urine analysis will make it possible to differentiate myofascial pain in the lower back and renal colic.
Doctors resort to instrumental diagnostics in cases where there is a suspicion of cardiac pathologies, in which there are pains similar to myofascial ones. The doctor may prescribe electro- or echocardiography, corono- or histography, ECG monitoring during the day according to Holter and other methods.
As already mentioned, pain in myofascial syndrome can be of two types: localized and reflected. It is the presence of the latter that causes difficulties in diagnosing the pathology.
Indicative in this regard is the right-sided myofascial syndrome with pain under the shoulder blade. Severe pain syndrome in this area can occur for various reasons. This can be pinched nerve roots, an attack of acute pancreatitis or cholecystitis, cholelithiasis or biliary dyskinesia, renal colic, pyelonephritis, malignant processes in the liver, pancreas, kidney on the right side.
 [ 24 ]
[ 24 ]
What do need to examine?
What tests are needed?
Differential diagnosis
The task of differential diagnostics is to detect or exclude the relationship between pathologies that are possible causes of pain in a certain area and myofascial pain. It is very important to find out the true cause of such pain in order to simultaneously treat both the cause and the effect. Only in this way will the treatment give the expected results.
After the patient has been examined by a local therapist, he or she may be referred for consultation to a neurologist, cardiologist, gastroenterologist, or traumatologist. The final diagnosis is made based on the results of the examination by these specialists. At the same time, effective treatment is prescribed for the pain syndrome itself and pathologies detected during diagnostics that can provoke muscle pain.
Who to contact?
Treatment myofascial syndrome
Myofascial syndrome is often caused by a peculiar duet: the cause of muscle pain (usually some health pathology) and the provoking factor (emotional stress, hypothermia, etc.). You have to fight both, which means the approach to treating myofascial pain syndrome should be comprehensive.
Sometimes it is possible to correct the situation without taking medications. This is possible if the cause of muscle pain is poor posture, heavy physical labor, sports, working at a computer, etc. The doctor gives such a patient recommendations regarding the work regime, posture correction, strengthening the back muscles, etc.
If the cause of MFBS is a serious illness, in parallel with pain relief, complex therapy for the existing health pathology is carried out.
Pain relief is achieved through drug therapy and alternative treatment methods. The following types of drugs are used as drug treatment:
- for pain relief: medications with anti-inflammatory and analgesic effects, such as Diclofenac, Nimesil, Ibuprofen, Voltaren Emulgel, etc., both in oral and topical forms,
- to relieve muscle tension and pain: drugs from the group of centrally acting muscle relaxants (Belofen, Tizanidine, Mydocalm, Sirdalud, Flexin),
- to stabilize the psycho-emotional state of patients: nootropic and gamkergic drugs (Picamilon, Pyriditol, Noofen, etc. 1-2 tablets 3 times a day), sedatives and vegetotropic drugs, antidepressants,
- general tonics and products for improving muscle tissue trophism: vitamins and vitamin-mineral complexes with an emphasis on preparations containing B vitamins and magnesium,
- to perform a blockade: most often, budget anesthetics "Novocaine" or "Lidocaine".
In addition to drug therapy for myofascial syndrome, various alternative methods and physiotherapy are used. The latter is especially relevant for myofascial syndrome of the face. In this case, electrical stimulation and thermomagnetic therapy, as well as cryoanalgesia, give good results.
Massage plays a major role in the treatment of myofascial pain, which can relieve muscle tension and improve blood circulation in the affected area, allowing medications to reach the site of action without hindrance. Manual therapy methods are especially indicative in this regard, as they act as a diagnostic and therapeutic procedure. It is only important that it is performed by a professional who knows his business.
Reflexology methods such as point massage and acupuncture also help relieve muscle hypertonicity and associated pain. Injecting medications into a muscle nodule to reduce its activity (pharmacopuncture) and stretching the affected muscle for the same purpose (osteopathy) also give good results in MFBS.
When the acute pain subsides, you can resort to cupping massage, doing it once every three days (about 6-8 procedures). After the massage, a warming rub or ointments that relieve pain and inflammation (for example, butadion or indomethacin) are applied to the affected area, the skin is covered with special compress paper and fabric.
In some medical institutions, patients may be offered a course of treatment with leeches. And if myofascial pain is associated with physical exertion, incorrect posture, muscle strain due to prolonged static position, and also if changes in the diseased muscle negatively affect other muscle groups, subjecting them to excessive loads, a set of exercises for various muscle groups may be prescribed, effective for myofascial syndrome of this type.
In advanced cases, when myofascial pain cannot be relieved by any of the listed methods, doctors may resort to surgical treatment, which involves releasing the nerve root from compression by the tense muscle (microvascular decompression).
Folk remedies
When talking about folk treatment of myofascial syndrome, it is important to understand that it only helps to temporarily relieve painful symptoms: spasms and muscle pain, but does not solve the problem radically. Without the use of muscle relaxants and various methods of physical impact on trigger points, it is impossible to achieve a lasting result.
But if drug therapy is not possible or in addition to it, the following recipes based on the positive effects of heat will help relieve pain:
- Paraffin wraps. Paraffin melted to a liquid state is applied to the site of pain. Another layer of paraffin is applied on top, after which the sore spot is covered with film and warmly wrapped for half an hour.
- 3 in 1 therapy:
- Dry heat. We apply coarsely ground salt heated to a hot state (so that the person can easily endure it) to the sore spot and cover it with a blanket. Remove it when it cools down.
- Iodine grid. After removing the salt, draw a grid on the skin with iodine.
- Medicinal patch. We glue a pepper patch over the iodine mesh. After the procedure, we send the patient to bed until the morning.
- Epsom salt (also known as magnesium sulfate or magnesia). It can be purchased at a pharmacy and used to relieve muscle spasms and pain by dissolving it in bath water. Warm water itself reduces pain, but magnesia also helps to relax tense muscles due to its magnesium content, a natural muscle relaxant. You will need 1 or 2 glasses of Epsom salt to take a bath. The procedure takes only 15 minutes.
But not only heat helps with myofascial pain. Massage with essential oils, which can be done at home, also has a therapeutic effect. A regular relaxing massage with mint, lemongrass and marjoram oils, taken in equal proportions, will help relieve muscle spasms. And essential oils of such plants as chamomile, basil, immortelle and lavender cope well with pain. It is better to use mixtures of different oils, adding them to a base oil (preferably coconut).
Herbal treatment for myofascial pain is carried out using horsetail, from which a healing ointment is made by mixing the crushed herb and butter in a ratio of 1:2, or an infusion of sweet clover flowers.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ]
Homeopathy
Since the main symptoms of myofascial syndrome are muscle spasms, leading to the appearance of trigger points, and the pain that accompanies them, the main focus of homeopathic treatment is precisely the removal of spasms and relief of myofascial pain.
The most popular antispasmodic in homeopathy is considered to be the drug "Spascuprel". It should be taken three times a day, 1 tablet, dissolving it in the mouth. To relieve pain during muscle spasm, you can take the drug 4 times within an hour until the pain subsides.
For muscle hardening and pain that goes away under the influence of heat, taking the homeopathic preparation “Rus toxicodendron” in 12 dilution will also be useful.
The drug "Brionia" in 12 dilution copes well with pain in the lower back, and for pain in the neck and between the shoulder blades, a homeopathic doctor can suggest "Chelidonium" drops.
The drugs "Brionia" and "Belladonna" are also effective for tension headaches, which also belong to the category of reflected myofascial pain.
Indicative for the relief of symptoms of myofascial pain syndrome is treatment with homeopathic subcutaneous or intramuscular Guna injections. For muscle pain, GUNA®-MUSCLE preparations are used for injections together with GUNA®-NECK, GUNA®-LUMBAR, GUNA®-HIP, etc.
More information of the treatment
Prevention
The effectiveness and duration of myofascial syndrome treatment depends not only on the severity of the process, but also on the patient's desire to get rid of the pain that torments him as soon as possible. Taking medications and physiotherapy, massage and manual practices will give a tangible and sustainable result if the patient adheres to the skills that are instilled in him during rehabilitation classes. These are new motor stereotypes, and the ability to control your body with control over the state of the muscular system, and the ability to strengthen the muscular corset, and correct posture.
And for those who do not want to face such an unpleasant disease, we advise you to take the following preventive measures:
- avoid muscle hypothermia and exposure of hot muscles to drafts,
- Limit physical activity, avoiding muscle strain,
- provide conditions for a good rest,
- when performing work that requires maintaining a static position for a long time, take short breaks with exercises for tired muscles,
- Treat illnesses in a timely manner, preventing them from becoming chronic.
By following these recommendations, you may never even know what myofascial syndrome with its excruciating pain is.

