Medical expert of the article
New publications
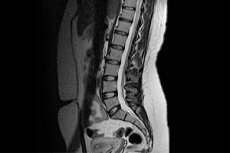
MRI of the lumbar spine
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Back pain, impaired mobility and sensitivity of the body in the lumbar region, difficulties with changing posture, bending and unbending the torso - all these are symptoms that disrupt the usual course of life, creating problems at home and at work, limiting a person's activities. It is clear that a person cannot endure such torment for a long time, so he turns to a doctor to find out the cause of the ailment and get qualified help. But how can doctors see those problems that are hidden inside the spine and often do not have specific external manifestations? Of course, with the help of X-rays, CT or MRI of the lumbar spine - methods that allow you to see the situation from the inside and make an accurate diagnosis.
Which method to choose?
As we can see, doctors have not one, but three options to accurately diagnose spinal diseases without damaging the skin and soft tissues. Modern medicine allows for such painless and effective diagnostic procedures. But are they all equally effective and safe?
X-ray examination is one of the oldest non-invasive methods of diagnosing diseases of internal organs, which dates back to the end of the 19th century. X-ray is the scanning of internal human structures using electromagnetic waves with a length of 10 -7 -10 -12 m (X-rays) with subsequent recording of the examination results on film.
This method of research has become widely used due to its low cost and ease of diagnostics. But at the same time, everyone has long known that radiography is not a safe procedure. Ionizing radiation has a harmful effect on the body, provoking the development of pathological processes in it.
Moreover, it can only produce a regular static image on a plane, which does not allow for a detailed assessment of the condition of the organ being examined. The diagnosis is made based on the study of the X-ray shadow (a shadow image that follows the contours of the internal organs of a person). But various internal structures can overlap and distort the image somewhat.
Computer tomography is a more modern diagnostic method, which appeared 77 years after radiography, which already gives a layered image of the object of study. CT provides the ability to obtain a spatial image of an organ on a computer screen. This image can be rotated, viewed from different angles, and the study can be conducted over time (the duration of the procedure is very different from X-ray, which takes only a couple of minutes).
The information content of such a diagnostic procedure is much higher, but the equipment for its implementation is expensive, and not every clinic can afford it. It is clear that the cost of diagnostics will be significantly higher.
But that's not all. Despite the fact that during computed tomography the radiation load on the patient's body is lower, the procedure actually remains essentially the same X-ray using ionizing radiation, so the number of procedures is limited. In addition, such a study, like radiography, is not suitable for expectant mothers, because it can have a negative effect on the development of the fetus.
Magnetic resonance imaging is a method that is only 1 year older than CT, but it is fundamentally different from its predecessors in that the procedure does not use unsafe X-rays. The study is based on the properties of hydrogen atoms (and half of our body consists of them) under the influence of an electromagnetic field to change their spin and give off energy.
Different human organs have different amounts of hydrogen atoms, so the images of individual organs will differ. Tissues of different densities will also produce images of different shades. And if a tumor or hernia has formed in an organ, there is inflammation or displacement of bone structures, all this will be reflected on the computer screen.
Thus, the MRI image of the lumbar spine is nothing more than the reflection of electromagnetic rays from various internal structures of the body in the lumbosacral region, which reproduces on the computer screen the response of hydrogen atoms to the action of the magnetic field. Such an image allows you to determine the slightest changes characteristic of the initial stage of the disease of the spine or nearby structures, and those that indicate the neglect of the process.
If there is a suspicion of a tumor process in the lumbar region or it is necessary to detail the paths of metastasis after removal of the neoplasm, the MRI procedure is performed with contrast (in principle, the same is possible when performing X-rays or CT), for which gadolinium or iron oxide preparations are first injected into the patient's vein. The introduction of contrast is also useful for monitoring the condition of the spine after removal of an intervertebral hernia.
In any case, MRI allows detecting more or less dangerous pathologies, be it inflammatory-degenerative changes in the spinal column, congenital anomalies, malignant or benign tumors or the result of a spinal injury. Such diagnostics allows making an accurate diagnosis in order to assess the possible consequences of the disease and develop an effective treatment plan.
Electromagnetic radiation from an MRI scanner, unlike X-rays used in radiography and computer tormography, does not harm our body, which means that such a study can be carried out without fear as many times as necessary. It is suitable for diagnosing spinal diseases in children and pregnant women, since it has a minimum of contraindications and side effects.
Despite the fact that the cost of MRI, as well as CT scan, is significantly higher than the price of film for X-ray of the spine, such a study provides much more information to the doctor and allows to identify hidden disorders that are inaccessible to viewing by a conventional X-ray machine. In addition, when conducting MRI, the patient has the opportunity to receive 2 types of information carrier: a static image on photographic paper and a spatial-temporal image on a digital carrier (computer disk, flash drive).
The advantages of CT and MRI over the X-ray examination we are accustomed to are undeniable. Therefore, whenever possible, it is recommended to resort to more modern diagnostic methods. In some cases, for example, when examining the chest and lungs, CT is considered more preferable. For examining changes in the lumbosacral region, both methods are considered equally effective and approximately equal in cost (any tomograph is considered expensive equipment), so everything usually depends on the degree of safety and the desire of the patient.
Indications for the procedure
The lumbar spine includes 5 sequentially located vertebrae, which are separated from each other by intervertebral discs. Next comes the sacral section, consisting of 5 vertebrae fused into one common bone, and the coccyx (a rudimentary organ similar in structure to the sacrum, but smaller in size).
In fact, the lumbar region is the lowest movable part of the human spine, which bears the greatest loads, so the causes of back and lower back pain are often associated with it. The bones themselves cannot hurt, but in addition to bone structures in the form of vertebrae and intervertebral discs, the lumbar-sacral region includes ligaments, tendons, nerves, muscles, blood vessels, which can be injured as a result of vertebral displacement or degenerative changes in bone-cartilaginous structures.
The proximity of the lumbar and sacral spine leads to the fact that in order to determine the cause of pain and limited mobility of the spine in the lumbar region, doctors consider it appropriate to examine both sections, so the procedure in most cases is called MRI of the lumbosacral spine.
Usually, a spine examination is required if the patient complains of back pain closer to the lower back, which prevents the body from changing position. After the patient tells about the symptoms that have appeared, the doctor already begins to suspect possible pathological processes in the body that cause the appearance of the described clinical picture. With a certain degree of accuracy, the diagnosis can be confirmed by a blood test or a spinal puncture, but only specialized instrumental studies can help make a final diagnosis, outline the affected area, see what processes led to the disease and develop a further scheme for solving the problem, one of which is MRI of the lumbar spine.
Indications for MRI examination may include:
- suspicion of any pathologies and injuries of the spine,
- suspicion of tumor processes in the lumbar region,
- suspected developmental anomalies of other parts of the spine, such as the cervical or thoracic,
- monitoring the recovery period after removal of intervertebral hernia,
- identifying the route of metastasis after removal of a tumor in the lumbar or sacral region,
- impaired mobility of the limbs in the sacral region,
- leg pain and back pain of unknown etiology,
- preparation for the upcoming operation in the lumbar region and monitoring in the postoperative period,
- diagnosis of multiple sclerosis and determination of the degree of its progression,
- suspected syringomyelia, a pathology characterized by the formation of cavities inside the spinal cord,
- identifying the causes of circulatory disorders in the lower extremities (risk factors for such disorders may include injuries, inflammatory and degenerative processes in the vertebral area, as a result of which blood vessels are compressed).
As for spinal diseases, in addition to injuries (fracture or severe contusion of the spinal column, its instability), doctors also consider the following pathological processes:
- inflammatory processes in the spinal cord ( myelitis ),
- infectious inflammation of bone tissue ( osteomyelitis ),
- decreased bone density of the spine ( osteoporosis ),
- the appearance of spiky growths along the edges of the vertebrae and their proliferation, which impairs the mobility of the spine and leads to a narrowing of its canal ( spondylosis ),
- dystrophy of the cartilaginous tissue of the spine ( osteochondrosis of the lumbar spine, which is a very common disease, for which MRI is more informative, allowing the doctor to determine the extent of the lesion and make prognoses of the disease),
- damage to the cartilaginous tissue of the joints with involvement of soft tissues, tendons and bones ( osteoarthritis ),
- displacement of vertebrae ( spondylolisthesis ),
- pathologies of intervertebral discs (their displacement, hernia, protrusions, chronic pain syndrome in the spine or dorsopathy, inflammation and fusion of intervertebral joints or Bechterew's disease ),
- the presence of transitional vertebrae on the border of the lumbar and sacral regions (if they are asymmetrical, instability of the spine occurs, lumbar scoliosis develops, etc.),
- stenosis or narrowing of the spinal column, which is a consequence of long-term inflammatory and degenerative processes in the spine
- formation of a cyst in the coccyx area.
MRI provides very valuable information when tumor processes are suspected. The study not only helps to identify the presence of a tumor, but also accurately determine its location, size, structure and the presence of metastases in other organs. The procedure can be prescribed even if the tumor was located in other areas, but there is a suspicion that its metastases have penetrated the lumbar spine. MRI allows you to control the quality of the metastasis removal process.
In diagnostics of intervertebral hernia and instability of the spine in the areas of transitional vertebrae, MRI with verticalization is very indicative. This study involves studying the condition of the spine in the lying and sitting positions, when the tomograph table and magnet are raised to a vertical position. In this case, the spine begins to experience a noticeable axial load, and defects become more obvious.
Preparation
MRI of the lumbar spine is one of the diagnostic examinations that does not require special preparation for the procedure. The patient will not have to reconsider their daily routine and food preferences or worry about the medications they take. The tomograph readings will not depend on what the person ate the day before the examination or when they visited the toilet. This is one of the advantages of the MRI method.
You will not need to bring bedding or special clothing for the procedure. Disposable items are given to the patient at the clinic where the examination is taking place. The patient will also be asked to remove any items containing metal parts (watches, rings, earrings, bracelets, piercings, etc.) that may interact with the magnetic field, causing unwanted changes and threatening tissue burns.
If the patient has not told the doctor about any metal objects inside the body (dentures, pacemakers, implants, artificial joints or heart valves, IUDs, etc., including shell fragments and bullets) the day before, now is the time to tell the doctor, indicating the material (if possible) from which the implant or prosthesis is made. Any large metal implants and fragments, as well as electronic devices and implants made of ferromagnetic materials that cannot be removed, will be an obstacle to performing an MRI.
You cannot take keys, payment cards, mobile phones and other electronic devices with you to the procedure. They can be left with relatives.
The tomograph is a large torus-shaped device with a sliding table. Some people, for example those who suffer from claustrophobia, may be afraid of the moment when the table they are lying on moves into the cavity of the device or remains there for a long time. If such a fear is present, it is necessary to tell the doctor about it, who will first make sure that the patient is given a sedative.
In principle, this is where the preparation for the tomograph examination procedure ends. But this is only if the MRI is performed without the introduction of contrast. The introduction of contrast chemicals into the body requires special caution.
The patient will have to take blood and urine tests, and undergo an allergy test. Gadolinium and iron oxide used for MRI are not as strong allergens as contrast agents for CT, but it is still better to be on the safe side to avoid harming a person. Urine analysis will show the condition of the kidneys, which are primarily affected by drugs, and blood tests will help confirm or rule out the presence of hemolytic anemia, in which red blood cells are destroyed (a magnetic field can enhance this process).
If during MRI without contrast the patient can eat until the beginning of the procedure, then the introduction of contrast requires abstinence from food and medications at least 3-4 hours before the beginning of the examination. This will help to avoid unpleasant consequences in the form of nausea and vomiting.
What do you need to bring with you for an MRI of the lumbar spine with or without contrast? There is no mandatory list, but it is recommended to have documents proving the patient's identity, an outpatient card, the results of previous spine studies (if any), test results, and a doctor's referral. But even if a person does not have all of these documents with them, this is not a reason to refuse to conduct an MRI diagnosis.
Technique Lumbar MRI
After the person is ready for the examination, they are dressed in special disposable clothing and placed on the tomograph table. The doctor will ask you not to move during the scan, since any movement can distort the overall picture of the examination. If a person has difficulty staying in a static position for a long time, which often happens with small children or with severe pain in the spine, their body will be fixed with special belts. Alternatively, intravenous anesthesia or painkillers can be administered, which do not affect the accuracy of the results.
The patient is warned in advance that during the procedure he will be alone in the room where the tomograph is located (although in some cases the presence of relatives or clinic staff is allowed). The doctor and, if necessary, the patient's relatives will be in another room at this time, where it is possible to observe what is happening. That is, the doctor will monitor the patient's condition remotely. In addition to remote visual contact, there is the possibility of two-way voice communication. The tomograph is equipped with a microphone, and the patient has the opportunity to call for help or report discomfort during the procedure. While in another room, the patient hears all the doctor's instructions regarding the correct behavior during the procedure.
The operating device produces a monotonous hum, which can frighten or irritate patients, so those being examined are given special vacuum headphones to help them feel more comfortable.
The table on which the patient is placed moves inside the tomograph until the part of the body that needs to be scanned is inside the device. After this, a magnetic field is turned on, which is many times greater than the Earth's magnetic field, and the device begins scanning the area affected by the disease.
The answer to the question of how long an MRI of the lumbar spine lasts is ambiguous. In most cases, everything is limited to 15-20 minutes, but in some cases, diagnostics can take even 30-40 minutes, depending on the complexity of the pathology. If contrast is administered, the duration of the procedure will be somewhat longer than an MRI without contrast.
MRI of the lumbar spine is usually performed in two projections: axial (transverse) and sagittal (vertical). During the entire procedure, the device, the magnet inside of which rotates around the area being examined several times (as specified in the instructions), takes a series of images that allow a full three-dimensional image of the area being examined to be restored on the computer screen.
Contraindications to the procedure
Magnetic resonance imaging is one of the safest diagnostic procedures, but this does not mean that this method has no contraindications. However, the limitations of the diagnostic examination are associated not so much with the pathologies present in the body, but with the metals previously introduced into the patient's body.
There are not so many absolute contraindications to MRI of the lumbar spine without contrast. The procedure is not performed on patients whose bodies contain ferromagnetic implants or metals that can interact with a magnetic field or can cause tissue burns, and electronic devices that support the patient's life (a magnetic field can adversely affect the operation of pacemakers and other similar devices). Ferromagnetic components may be present in artificial middle ear simulators, shell fragments, the Ilizarov apparatus, and some other implants.
Relative contraindications include the use of an insulin pump, portable electrical stimulators of the nervous system, the presence of middle and inner ear implants, heart valve simulators, hemostatic clips, dental implants and braces made of metals that are not ferromagnetic. Some precautions will have to be taken when performing the procedure on patients with decompensated heart failure, claustrophobia and inadequate patient behavior (in this case, drug-induced sleep is recommended).
It is not advisable to perform magnetic resonance imaging on patients in very serious condition, as well as on pregnant women in the early stages, but if urgent diagnostics of pathologies is necessary, MRI of the lumbar spine can be performed even on such patients, and it is considered more preferable than the popular X-ray or CT scan.
An obstacle to MRI may also be the presence of tattoos that were applied using titanium compounds. In this case, there is a risk of tissue burns.
Tomographs used for MRI diagnostics can have a closed or open circuit. An open circuit device allows the procedure to be performed by many patients with relative contraindications.
If we are talking about MRI with contrast, it is not performed to diagnose spinal pathologies in pregnant women at any stage (contrast agents can affect fetal development), in patients with hemolytic anemia and severe renal failure (the half-life of the chemical increases and, accordingly, its negative impact on the body). Accordingly, contrast is unacceptable in patients with allergic reactions to the administered drug.
 [ 5 ]
[ 5 ]
Normal performance
The results of MRI of the lumbosacral spine are deciphered after the completion of the examination procedure. Although some clinics have the ability to conduct tomography with visualization, and already in the process make some conclusions about the condition of the spine and surrounding tissues.
Some people may find the MRI procedure too time-consuming (compared to a regular X-ray), but it is necessary to obtain a three-dimensional image consisting of many individual flat images taken in increments of 0.5-5 mm. You will have to wait even longer for the results of the examinations. Most often, it takes a specialist about 60 minutes to decipher them, but in the case of multiple or complex fractures, as well as in the presence of tumor processes, the results can be obtained even the next day.
What does an MRI of the lumbosacral spine show? On the image obtained using an MRI scanner, the doctor can see:
- curvature of the spinal column in the lumbosacral region,
- inflammatory processes in various tissues (cartilage, muscles, nerves, etc.),
- degenerative changes in bone and cartilage tissue (hardening or thinning of cartilage, destruction (decrease in density) of bones, appearance of growths, decrease in the distance between vertebrae, etc.),
- tumors and other neoplasms in the lumbosacral region, which on an MRI image appear as a round spot that is darker than other tissues,
- tumor metastases in the form of clearly defined objects of various shapes, surrounded by edematous tissues,
- displacement of the vertebrae relative to the axis,
- disturbances of blood flow in the vessels of the pelvic region and lower extremities,
- the presence of voids in the spinal cord.
MRI allows not only to visualize pathology, but also to assess the degree of damage to the spine and adjacent structures, because changes in the structure and position of the bone structures of the spinal column often lead to circulatory disorders and the appearance of neurological symptoms due to pinched nerve fibers.
Hence the pain syndrome with which patients come to a therapist, traumatologist or orthopedist. A person may go to a doctor complaining of pain, weakness and loss of sensitivity in the legs, and an MRI of the lumbar region will reveal the cause of these symptoms in changes in the structure of the spine in the lumbar and sacral region.
Complications after the procedure
MRI of the lumbar spine is considered a safe procedure, with no immediate or long-term consequences. It is clear that we are talking about diagnostics taking into account absolute and relative contraindications, as well as requirements for high-quality scanning.
As for discomfort during the examination, there are practically none. Some patients may feel slight twitching in the muscles of the body or a slight tingling, which is a normal variant and should not frighten the person being examined.
When MRI is performed with contrast and requires the introduction of chemicals into the body, patients may experience headaches, nausea or vomiting after the procedure, which are associated with the action of "chemistry" and not the magnetic field. If we are not talking about increased sensitivity of the body to chemotherapy drugs, these symptoms pass rather quickly and have no consequences. To reduce the severity of such unpleasant consequences, a test for sensitivity to contrasts is carried out in advance and a requirement is introduced not to eat for 1.5-2 hours before the procedure.
If there are tattoos on the body in the area of the body exposed to a strong magnetic field, the patient may feel a noticeable burning sensation, which is a consequence of tissue burns.
MRI machines do not use ionizing radiation, which can cause various complications after the procedure. But the magnetic field can affect the operation of electronic devices implanted in the body and attract prostheses made of ferromagnetic alloys, so it is not worth taking risks. The doctor should be aware of the possible risks to the same extent as the patient, who is warned about the consequences before the procedure.
In any case, there is constant communication between the person being examined on the tomograph table and the doctor performing the procedure, and the person has the opportunity to report any unpleasant sensations that require stopping the device and medical assistance.
Care after the procedure
MRI of the lumbar spine is a non-invasive and painless examination, so no post-procedure care is required. Immediately after the diagnostic examination, the patient can go home. But since the diagnostics are carried out purposefully, their results usually indicate a certain pathology that requires appropriate treatment. That is, after conducting magnetic resonance imaging and receiving its results, the patient will have to visit some more medical specialists (traumatologist, surgeon, phlebologist, neurologist, etc.), who, having studied the MRI information, will develop an effective treatment plan for the disease identified.

