Medical expert of the article
New publications
Metastasis to the liver
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The liver is the most common localization of hematogenous tumor metastases, regardless of whether the primary tumor is drained by the portal vein system or other veins of the systemic circulation.
Liver metastases are common in many cancers, especially those originating in the gastrointestinal tract, breast, lung, and pancreas. Initial symptoms are usually nonspecific (eg, weight loss, right upper quadrant discomfort) but sometimes present with symptoms of the primary cancer. Liver metastases are suspected in patients with weight loss, hepatomegaly, and primary tumors with an increased risk of liver metastasis. Diagnosis is usually confirmed by imaging studies, most commonly ultrasound or helical CT with contrast. Treatment usually includes palliative chemotherapy.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ]
Epidemiology
Liver metastases are found in about a third of cancer patients, and in stomach, breast, lung, and colon cancers, they are observed in half of patients. The next most common liver metastases are esophageal cancer, pancreatic cancer, and melanoma. Liver metastases from prostate and ovarian cancer are extremely rare.
Metastatic liver cancer is more common than primary liver cancer and is sometimes the first clinical manifestation of a malignant tumor in the gastrointestinal tract, breast, lung, or pancreas.
 [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
[ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ]
Pathogenesis
Liver invasion by malignant tumors of neighboring organs, retrograde metastasis through the lymphatic pathways, and spread along the blood vessels is relatively rare.
Portal emboli enter the liver from malignant tumors of the portal venous system. Occasionally, primary tumors of the uterus and ovaries, kidneys, prostate gland, or bladder may invade adjacent tissues that drain into the portal venous system, possibly leading to embolic metastases to the liver; however, liver metastases from these organs are extremely rare.
Metastatic seeding via the hepatic artery, which apparently occurs frequently, is difficult to establish histologically, since the picture is the same as with intrahepatic metastasis.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ]
Macroscopic picture
The degree of liver damage may vary. It is possible to detect only 1-2 nodes microscopically or a significantly enlarged liver, “stuffed” with metastases. Frequently, the liver mass reaches 5000 g. A case has been described where the mass of the liver affected by metastases was 21,500 g. Metastases are usually white and have clear boundaries. The consistency of the tumor depends on the ratio of the volume of tumor cells and fibrous stroma. Sometimes softening of the central part of the tumor, its necrosis and hemorrhagic impregnation are observed. Central necrosis of metastatic nodes is a consequence of insufficient blood supply; it leads to the appearance of retractions on the surface of the liver. Perihepatitis often develops over metastatic nodes located on the periphery. The nodes are sometimes surrounded by a zone of venous hyperemia. Invasion into the portal vein is often observed. Arteries are rarely affected by tumor thrombi, although they can be surrounded by malignant tissue.
Tumor cells rapidly metastasize, involving large areas of the liver both through the perivascular lymphatic pathways and along the branches of the portal vein.
Angiography results indicate that, unlike hepatocellular carcinoma, the arterial blood supply to liver metastases is poor. This is especially true for metastases from primary gastrointestinal tumors.
Histological examination
Liver metastases may have the same histological structure as the primary tumor. However, this is not the rule; often the primary lesion is a highly differentiated tumor, while its liver metastases may be so poorly differentiated that their origin cannot be determined by histological examination.
 [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
[ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ]
Symptoms liver metastases
Early liver metastases may be asymptomatic. Nonspecific signs (eg, weight loss, anorexia, fever) are most common at first. The liver may be enlarged, firm, and tender; marked hepatomegaly with easily palpable nodules demonstrates progressive disease. Rare but characteristic symptoms include a friction rub over the liver and pleuritic chest pain, right flank pain. Splenomegaly sometimes develops, especially in pancreatic cancer. Dissemination of tumor with peritoneal involvement may cause ascites, but jaundice is usually absent or mild unless the tumor causes biliary obstruction. In the terminal stage, progressive jaundice and hepatic encephalopathy herald death.
The clinical picture may consist of symptoms of liver metastases and symptoms of the primary tumor.
Patients complain of malaise, increased fatigue and weight loss. The feeling of distension and heaviness in the upper abdomen is caused by an enlarged liver. Sometimes acute or paroxysmal abdominal pain is possible, which simulates biliary colic. Fever and sweating are possible.
In cases of significant weight loss, patients appear emaciated, and the abdomen is enlarged. The liver may be of normal size, but sometimes it enlarges so much that its contours are visible in the upper abdomen. Metastatic nodes have a dense consistency, sometimes with umbilical depressions on the surface. Friction noise may be heard above them. Due to poor blood supply, arterial noise is absent. Splenomegaly is common, even with normal portal vein patency. Jaundice is mild or absent. Intense jaundice indicates invasion of large bile ducts.
Edema of the lower extremities and dilation of the veins of the anterior abdominal wall indicate compression of the inferior vena cava by the affected liver.
The supraclavicular lymph nodes on the right may be affected.
Pleural effusion, along with some other local symptoms, may indicate metastases to the lungs or the presence of a primary tumor in the lung.
The development of ascites reflects the involvement of the peritoneum in the process, and in some cases - portal vein thrombosis. As a result of portal vein thrombosis and portal hypertension, bleeding may develop. A rare complication of liver metastases from breast cancer, colon cancer, or small cell lung cancer is the development of mechanical jaundice.
Metastases are the most common cause of true liver enlargement.
Hypoglycemia is a rare symptom of liver metastases. The primary tumor is usually sarcoma. In rare cases, massive tumor infiltration and liver parenchyma infarctions can lead to fulminant liver failure.
If malignant carcinoid tumors of the small intestine and bronchi are accompanied by vasomotor disorders and bronchial stenosis, then multiple metastases are always detected in the liver.
Stool discoloration occurs only with complete obstruction of the bile duct. If the primary tumor is localized in the digestive tract, the stool test for occult blood may be positive.
Where does it hurt?
What's bothering you?
Diagnostics liver metastases
If liver metastases are suspected, liver function tests are usually performed, but they are usually not specific for this pathology. Typically, alkaline phosphatase, gamma-glutamyl transpeptidase and sometimes - to a greater extent than other enzymes - LDP are elevated; aminotransferase levels vary. Instrumental studies are quite sensitive and specific. Ultrasound is usually informative, but spiral CT with contrast often provides more accurate results. MRI is relatively accurate.
Liver biopsy provides a definitive diagnosis and is performed when other studies are insufficiently informative or when histological verification is required (e.g., liver metastasis cell type) to select a treatment method. Biopsy is preferably performed under ultrasound or CT guidance.
 [ 46 ]
[ 46 ]
Biochemical indicators
Even with a large liver, its function may be preserved. Compression of relatively small intrahepatic bile ducts may not be accompanied by jaundice. Bile may flow through unaffected ducts. An increase in the serum bilirubin level above 2 mg% (34 μmol/l) indicates a violation of the patency of large bile ducts in the region of the liver porta.
Biochemical criteria for liver damage by metastases include increased activity of alkaline phosphatase or LDH. Increased activity of serum transaminases is possible. If the concentration of bilirubin in the serum, as well as the activity of alkaline phosphatase, LDH and transaminases are within normal limits, the probability of the absence of metastases is 98%.
Serum albumin concentration is normal or slightly decreased. Serum globulin levels may be elevated, sometimes significantly. Electrophoresis may reveal elevated alpha 2- or y-globulins.
In some patients, carcinoembryonic antigen is detected in the serum.
The ascitic fluid has an increased protein content, sometimes carcinoembryonic antigen is present; LDH activity is 3 times higher than that in serum.
 [ 47 ], [ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ], [ 53 ]
[ 47 ], [ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ], [ 53 ]
Hematological changes
Neutrophilic leukocytosis is quite common, sometimes the number of leukocytes increases to 40-50•10 9 /l. Mild anemia is possible.
 [ 54 ], [ 55 ], [ 56 ], [ 57 ]
[ 54 ], [ 55 ], [ 56 ], [ 57 ]
Liver biopsy
The diagnostic value of liver biopsy is increased when performed under visual control with ultrasound, CT, or peritoneoscopy. Tumor tissue has a characteristic white color and loose consistency. If a tumor column cannot be obtained, any blood clot or debris should be examined for tumor cells. Even if tumor cells cannot be aspirated, the detection of proliferating and abnormal bile ducts and neutrophils in edematous portal tracts, as well as focal dilation of the sinusoids, indicates the presence of metastases in adjacent areas.
Histological examination of preparations does not always allow to establish the localization of the primary tumor, especially in cases of pronounced anaplasia of metastases. Cytological examination of aspirated fluid and biopsy preparation prints may somewhat increase the diagnostic value of the method.
Histochemical staining is particularly important for cytological examination and small tissue sample sizes. Monoclonal antibodies, particularly HEPPARI, which react with hepatocytes but not with bile duct epithelium and nonparenchymatous liver cells, can differentiate primary liver cancer from metastatic liver cancer.
The probability of detecting metastases during liver puncture biopsy is higher with a significant tumor mass, large liver size and the presence of palpable nodes.
X-ray examination
Plain abdominal radiography reveals an enlarged liver. The diaphragm may be elevated and irregular in outline. Calcification of primary cancer or hemangioma and metastases of colon, breast, thyroid and bronchial cancer are occasionally observed.
Chest radiography may reveal associated pulmonary metastases.
X-ray contrast examination of the upper gastrointestinal tract with barium allows visualization of esophageal varices, leftward displacement of the stomach and rigidity of the lesser curvature. Irrigoscopy reveals prolapse of the hepatic angle and transverse colon.
Scanning
Scanning usually allows us to identify lesions with a diameter of more than 2 cm. It is important to determine the size of tumor nodes, their number and location, which is necessary to assess the possibility of liver resection and monitor the patient.
Ultrasound is a simple, effective diagnostic method that does not require large expenses. Metastases in ultrasound appear as echogenic foci. Intraoperative ultrasound is especially effective for diagnosing liver metastases.
In AG, metastases appear as foci with low radiation absorption. Metastases from the colon usually have a large avascular center with a ring-shaped accumulation of contrast agent at the periphery. In approximately 29% of patients who have undergone colon resection for cancer, CT reveals hidden liver metastases. Delayed accumulation of contrast agent increases the frequency of metastasis detection. CT with iodolipol contrast is also used.
T1-weighted MRI is the best method for detecting liver metastases from colon cancer. T2-weighted images show swelling of liver tissue adjacent to metastases.
MRI with iron oxide or gadolinium has greater sensitivity. Duplex color Doppler ultrasound reveals less pronounced congestion in the portal vein than in liver cirrhosis and portal hypertension.
 [ 61 ], [ 62 ], [ 63 ], [ 64 ], [ 65 ], [ 66 ], [ 67 ]
[ 61 ], [ 62 ], [ 63 ], [ 64 ], [ 65 ], [ 66 ], [ 67 ]
Diagnostic difficulties
In a patient with a diagnosed primary tumor and suspected liver metastasis, it is usually not possible to confirm the presence of metastases based on clinical data. Increased serum bilirubin levels, serum transaminase activity, and alkaline phosphatase indicate possible liver metastasis. Liver aspiration biopsy, scanning, and peritoneoscopy are performed to confirm the diagnosis.
Another diagnostic problem, which is usually of purely scientific interest, is the unknown location of the primary tumor in diagnosed metastatic liver disease. The primary tumor may be breast cancer, thyroid cancer, or lung cancer. Positive results of a stool occult blood test indicate tumor localization in the gastrointestinal tract. A history of removed skin tumors and the presence of nevi suggest melanoma. Suspicion of pancreatic body cancer dictates the need for endoscopic retrograde cholangiopancreatography. Usually, the localization of the primary tumor can be determined based on the results of a puncture biopsy of the liver. However, sometimes a biopsy reveals only squamous, scirrhous, cylindrical, or anaplastic cells, but the localization of the primary lesion remains unknown.
What do need to examine?
What tests are needed?
Who to contact?
Treatment liver metastases
Treatment depends on the extent of metastasis. In colorectal cancer with solitary or multiple metastases, resection may prolong survival. Depending on the characteristics of the primary tumor, systemic chemotherapy may shrink the tumor and prolong survival but is not curative; intra-arterial chemotherapy sometimes achieves the same results with fewer or less severe systemic adverse effects. Liver radiation therapy sometimes relieves pain in advanced metastases but does not prolong survival. Advanced disease is fatal, so the best approach is to palliate the patient and support the family.
Treatment results remain unsatisfactory. In patients with a more favorable prognosis without treatment (for example, in patients with rectal cancer with liver metastases), it improves with specific treatment. Most published results are obtained in uncontrolled studies. Nevertheless, treatment should be carried out in all cases so as not to deprive patients and their relatives of hope. The treatment method that can slow tumor growth to the greatest extent with the least side effects is chosen.
Combination therapy is performed with 5-fluorouracil and mitoxantrone in combination with methotrexate and lomustine. It is accompanied by severe side effects, and there are no results of controlled studies. The best treatment results are observed in metastatic breast cancer.
Metastases are resistant to radiation therapy. In carcinoid syndrome, surgical intervention is indicated, which is associated with a high risk. Metastatic nodes are quite easily enucleated. Apparently, embolization of the branches of the hepatic artery that feed the tumor nodes is more preferable. In metastases of other tumors, embolization of arteries with gelatin foam is also used.
Administration of chemotherapy drugs into the hepatic artery
Primary and secondary liver tumors are supplied with blood mainly from the hepatic artery, although the portal vein also plays a small role. Cytostatics can be administered to the tumor by catheterization of the hepatic artery. The catheter is usually placed in the hepatic artery, inserted through the gastroduodenal artery. The gallbladder is removed. The chemotherapy drug usually used is floxuridine, 80-95% of which is absorbed during the first pass through the liver. It is administered using an implantable infusor gradually monthly for 2 weeks.
This treatment results in tumor regression in 20% of patients and improves the condition in 50%. In colorectal cancer, survival with this treatment increased to 26 months compared to 8 months in the control group. According to one study, the results of regional chemotherapy were better than the results of systemic therapy. In another study, when chemotherapy was administered through the hepatic artery, 35 of 69 patients showed improvement, 9 had no change in their condition, and 25 had tumor progression.
Complications included sepsis and catheter dysfunction, peptic ulcers, chemical cholecystitis and hepatitis, and sclerosing cholangitis.
Perfusion of drugs through the hepatic artery can be used as an additional treatment method after liver resection.
There is a report on the combination of cryotherapy with regional perfusion of cytostatics through the hepatic artery.
Interstitial laser photocoagulation under ultrasound control was also performed. CT revealed a 50% reduction in tumor volume.
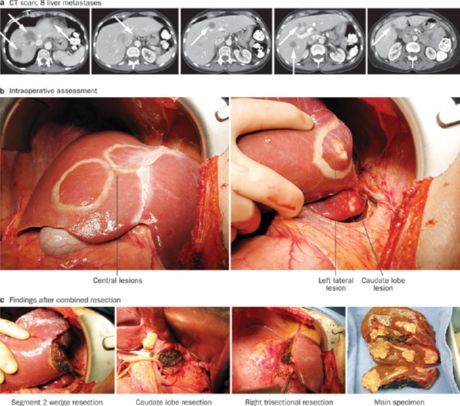
Removal of colon cancer metastases
Metastatic tumors grow slowly, can be solitary, and most of them are localized subcapsularly. Resection of the affected liver area can be performed in 5-10% of patients. Liver scanning is performed before surgery. CT during arterial portography has high sensitivity. Intraoperative ultrasound is also necessary. Liver resection is indicated in cases where there are no more than four metastases in the liver and there is no damage to other organs or severe concomitant diseases. In every fourth patient, the expected volume of resection must be increased during surgery, and in every eighth patient, it must be abandoned. Usually, lobectomy or segmentectomy is performed.
In a multicenter study that included 607 patients with resected metastases, recurrence of liver metastases was noted in 43% of patients, and recurrence of lung metastases was noted in 31%. In 36% of patients, recurrence was detected within the first year. Twenty-five percent of patients survived the 5-year period without signs of tumor recurrence. In another study, the 10-year survival rate was quite high and amounted to 21%. If the concentration of carcinoembryonic antigen in the serum of patients did not exceed 200 ng/ml, the resection margin was at least 1 cm from the tumor, and the mass of excised liver tissue was less than 1000 g, the 5-year survival without signs of recurrence exceeded 50%. An increased risk of recurrence is noted in cases where resection fails to retreat a sufficient distance from the tumor and when metastases are localized in both lobes. In a study that included 150 patients, liver resection (46% of patients) increased life expectancy to an average of 37 months, after “non-radical” resection (12% of patients) life expectancy was 21.2 months, and for unresectable tumors (42% of patients) - 16.5 months.
However, controlled studies are needed to finally assess the effectiveness of surgical treatment of liver metastases.
 [ 73 ], [ 74 ], [ 75 ], [ 76 ], [ 77 ]
[ 73 ], [ 74 ], [ 75 ], [ 76 ], [ 77 ]
Liver transplantation
The two-year survival rate after liver transplantation for metastatic cancer averages only 6%.
Liver transplantation was found to be more effective in patients with endocrine tumors of the pancreas and liver metastases, provided that the primary tumor was also removed.
Forecast
The prognosis depends on the location of the primary tumor and the degree of its malignancy. In general, patients die within a year after the detection of liver metastases. A comparatively more favorable prognosis is observed for tumors of the rectum and colon. The average life expectancy of patients with liver metastases after colon resection is 12±8 months.

