Medical expert of the article
New publications
Hyperplastic processes of the endometrium
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Epidemiology
Hyperplastic processes of the endometrium are possible at any age, but their frequency increases significantly by the perimenopause period. According to most scientists, hyperplastic processes of the endometrium are considered precursors of endometrial cancer itself. Simple endometrial hyperplasia without atypia develops into cancer in 1% of cases, the polypoid form without atypia - 3 times more often. Simple atypical endometrial hyperplasia without treatment progresses into cancer in 8% of patients, complex atypical hyperplasia - in 29% of patients.
The most common type of endometrial hyperplastic process is polyps, which occur in gynecological patients with a frequency of up to 25%. Endometrial polyps are most often detected in pre- and postmenopause. Endometrial polyps become malignant in 2–3% of cases.
Causes endometrial hyperplastic processes
Most often, hyperplastic processes of the endometrium are diagnosed in women with increased concentrations of estrogens of any genesis. Increased levels of estrogens in women taking hormone replacement therapy (HRT) increase the risk of developing endometrial hyperplasia. Tamoxifen is considered effective in the treatment of patients with breast cancer, but its use increases the risk of developing hyperplastic processes of the endometrium.
Symptoms endometrial hyperplastic processes
The main clinical manifestations of endometrial hyperplastic processes are uterine bleeding, often acyclic in the form of metrorrhagia, less often menorrhagia. Sometimes endometrial polyps are asymptomatic, especially in postmenopause.
Since the pathogenetic basis of endometrial hyperplastic processes is anovulation, the leading symptom in patients of reproductive age is infertility, usually primary.
What's bothering you?
Forms
There are three main types of endometrial hyperplastic processes: endometrial hyperplasia, endometrial polyps and atypical hyperplasia (adenomatosis).
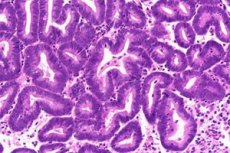
In 1994, the WHO adopted a classification of endometrial hyperplasia based on recommendations from leading gynecologists and pathologists, including hyperplasia without cellular atypia and hyperplasia with cellular atypia (atypical endometrial hyperplasia or adenomatosis). In each group, simple and complex hyperplasia are distinguished, depending on the severity of proliferative processes in the endometrium.
An endometrial polyp is a benign tumor-like formation originating from the basal layer of the endometrium. The pathognomonic anatomical feature of an endometrial polyp is its base, the "pedicle". Depending on the histological structure, there are glandular (functional or basal type), glandular-fibrous, fibrous and adenomatous polyps of the endometrium. Adenomatous polyps are characterized by intensive proliferation of glands and their epithelium with relatively high mitotic activity. Adenomatous polyps are considered precancerous conditions. Glandular polyps are most typical for the reproductive period, glandular-fibrous - for pre- and perimenopause, fibrous-glandular and fibrous - for postmenopause.
In the reproductive and premenopausal period of a woman's life, endometrial polyps as a histologically independent form can be determined both against the background of endometrial hyperplasia and with a normal mucous membrane of various phases of the menstrual cycle.
Endometrial polyps in postmenopause are usually solitary and may occur against the background of an atrophic mucous membrane. In the postmenopausal period, endometrial polyps sometimes reach large sizes and extend beyond the cervix, thereby imitating a cervical polyp.
The concept of “relapse” of an endometrial polyp is unacceptable if hysteroscopic control was not previously used during the removal of the endometrial polyp, since scraping the uterine mucosa without hysteroscopy may leave pathologically altered tissue.
From a morphological standpoint, endometrial precancer includes hyperplasia with atypia (atypical hyperplasia) and adenomatous polyps.
Diagnostics endometrial hyperplastic processes
In addition to generally accepted examination methods, an important point is the identification of concomitant diseases and assessment of the condition of the liver, cardiovascular system (CVS), gastrointestinal tract (GIT), as this is important when choosing a treatment method, especially the appointment of hormonal therapy.
The main methods of diagnosing endometrial hyperplastic processes at the present stage include cytological examination of aspirate from the uterine cavity, transvaginal ultrasound, hydrosonography and hysteroscopy. However, the diagnosis can only be finally verified after a histological examination of the endometrium, obtained by separate diagnostic curettage of the uterine mucosa.
Cytological examination of aspirate from the uterine cavity is recommended as a screening test for endometrial pathology and determination of its condition in dynamics against the background of hormonal therapy. This method allows determining the severity of proliferative changes, but does not give a clear idea of its pathomorphological structure.
Transvaginal ultrasound scanning is a valuable method for diagnosing endometrial hyperplastic processes due to its high information content, non-invasiveness, and harmlessness to the patient. Ultrasound allows assessing not only the condition of the endometrium, but also the myometrium, and identifying adenomyosis and uterine myoma. Ultrasound should also be performed to determine the size of the ovaries and assess their functions.
The diagnosis of endometrial hyperplasia by ultrasound is based on the detection of an enlarged anteroposterior size of the median uterine echo (M-echo) with increased acoustic density. In menstruating women, the thickness of the M-echo should be assessed in accordance with the phase of the menstrual cycle. It is best to conduct the study immediately after menstruation, when a thin M-echo corresponds to complete rejection of the functional layer of the endometrium, and an increase in the anteroposterior size of the M-echo along its entire length, or locally, is regarded as pathology. It is impossible to distinguish glandular hyperplasia of the endometrium from atypical by ultrasound.
If the postmenopausal period does not exceed 5 years, the thickness of the M-echo up to 5 mm is considered normal, with postmenopause more than 5 years, the thickness of the M-echo should not exceed 4 mm (with a homogeneous structure). The accuracy of ultrasound diagnostics for endometrial hyperplastic processes is 60-70%.
Hydrosonography can significantly improve diagnostic results. Ultrasound image of endometrial polyps shows ovoid, less often round inclusions in the structure of the M-echo and the uterine cavity with increased echo density. Diagnostic difficulties arise with glandular polyps of the endometrium, which have a leaf-shaped or flattened configuration in the shape of the uterine cavity and are not capable of leading to thickening of the M-echo. In terms of sound conductivity, they are close to the surrounding endometrium. Registration of color echo signals during Doppler examination in the structure of the inclusion makes it possible to differentiate polyps from intrauterine adhesions, and in menstruating patients - from blood clots, but blood flow in polyps is not always determined during color duplex mapping. The information content of transvaginal ultrasound for endometrial polyps is 80-90%. Contrasting the uterine cavity during hydrosonography can increase the diagnostic capabilities of ultrasound. Transvaginal hydrosonography and endometrial biopsy allow diagnosing GPE in 98%.
The informative value of hysteroscopy in diagnostics of endometrial hyperplastic processes is 63–97% (depending on the type of endometrial hyperplastic processes). Hysteroscopy is necessary both before curettage of the uterine mucosa to clarify the nature of the pathology and its localization, and after it in order to control the thoroughness of tissue removal. Hysteroscopy allows visually assessing the condition of the uterine walls, identifying adenomyosis, submucous uterine myoma and other forms of pathology. Atypical endometrial hyperplasia does not have characteristic endoscopic criteria, the hysteroscopic picture resembles ordinary glandular cystic hyperplasia. In severe atypical hyperplasia, glandular polypoid growths of a dull yellowish or grayish color can be identified.
Histological examination of scrapings of the uterine mucosa is the definitive method for diagnosing hyperplastic processes of the endometrium.
 [ 26 ]
[ 26 ]
What do need to examine?
Who to contact?
Treatment endometrial hyperplastic processes
Therapy for women of different ages consists of stopping bleeding, restoring menstrual function during the reproductive period or achieving menopause at an older age, as well as preventing recurrence of the hyperplastic process.
Treatment of endometrial hyperplastic processes in patients of reproductive age
Hormonal therapy is considered a traditional method of treating endometrial hyperplastic processes.
Relapses of the endometrial hyperplastic process indicate insufficient therapy or hormonally active processes in the ovaries, which requires clarification of their condition, including visual diagnostic methods (ultrasound, laparoscopy, ovarian biopsy). The absence of morphological changes in the ovaries allows continuing hormonal therapy with higher doses of drugs. It is necessary to exclude an infectious factor as a possible cause of the disease and the ineffectiveness of hormonal therapy.
If hormone therapy is ineffective, or there is a relapse of endometrial hyperplasia without atypia, ablation (resection) of the endometrium is advisable. Endometrial ablation can be performed using various methods: using mono- and bipolar coagulators, lasers, and balloons. Necessary conditions for performing ablation: the woman does not want to have children in the future, is over 35 years old, wants to preserve the uterus, and the uterus size is no more than 10 weeks of pregnancy. Uterine fibroids are not considered a contraindication to endometrial ablation; if none of the nodes exceeds 4–5 cm, then adenomyosis worsens the results of the operation.
Recurrence of atypical endometrial hyperplasia in patients of reproductive age is an indication for in-depth examination and exclusion of polycystic ovary syndrome.
Treatment in pre- and perimenopause
The first stage of treatment includes hysteroscopy with separate diagnostic curettage of the uterine mucosa. The choice of further therapy depends on the morphological structure of the endometrium, concomitant gynecological and extragenital pathology. The choice of hormonal drug, the scheme and duration of treatment are also determined by the need to maintain a rhythmic menstrual-like reaction (up to the age of 50) or a persistent cessation of menstruation.
In case of recurrent endometrial hyperplasia without atypia, impossibility of hormone therapy due to concomitant extragenital pathology, hysteroscopic surgery - endometrial ablation is indicated. Recurrences of endometrial hyperplastic processes, as well as the combination of this pathology with uterine myoma and/or adenomyosis in patients in pre- and perimenopause are indications for surgical intervention (hysterectomy).
Postmenopausal treatment
Separate diagnostic curettage with hysteroscopy is indicated for patients with suspected endometrial pathology detected during screening examination. In case of newly detected endometrial hyperplasia in postmenopausal women, it is advisable to prescribe hormonal therapy.
In case of atypical endometrial hyperplasia in postmenopause, it is necessary to immediately decide on a radical operation - panhysterectomy. In case of severe extragenital pathology and increased risk of surgical treatment, long-term treatment with hormonal drugs indicated in Table 3 is permissible.
Against the background of hormonal therapy, it is advisable to recommend hepatoprotectors, anticoagulants, and antiplatelet agents in normal doses.
Recurrence of endometrial hyperplasia in postmenopause is an indication for surgical intervention: hysteroscopic ablation of the endometrium or extirpation of the uterus with appendages. Supravaginal amputation of the uterus with appendages is acceptable (in the absence of cervical pathology).
The main method of treating patients with endometrial polyps in postmenopause is targeted polypectomy. Radical removal of an endometrial polyp (with the basal layer at the site of localization of the polyp) is possible only with the use of hysteroscopic equipment. For polypectomy, both mechanical endoscopic instruments and electrosurgical technology, as well as a laser, can be used. Electrosurgical excision of the polyp during hysteroscopy is recommended for fibrous and parietal polyps of the endometrium, as well as for recurrent endometrial polyps.
After removal of glandular and glandular-fibrous polyps of the endometrium, it is advisable to prescribe hormonal therapy. The type of hormonal therapy and its duration depend on the morphological structure of the polyp and the accompanying pathology.
Hormonal therapy for endometrial polyps in postmenopause
| Preparation | Glandular fibrous, fibrous polyps | Glandular polyps |
| Norethisterone | 5 mg/day for 6 months | 10 mg/day for 6 months |
| Hydroxyprogesterone caproate | 250 mg once a week for 6 months | 250 mg 2 times a week for 6 months |
| Medroxyprogesterone | 10–20 mg/day for 6 months | 20–30 mg/day for 6 months |
Further management
Patients with endometrial hyperplasia should be under dispensary observation for at least 2 years after cessation of hormonal therapy; in case of atypical hyperplasia (if hormonal therapy was performed), the period of dispensary observation should be at least 5 years. Ultrasound of the pelvic organs and cytological examination of aspirate every 6 months are mandatory. The sensitivity of endometrial biopsy with Pipelle is 99% for determining endometrial cancer and 75% for endometrial hyperplasia in postmenopausal women. If pathology is detected according to ultrasound and cytological examination, hysteroscopy and separate diagnostic curettage of the uterine mucosa with histological examination of scrapings are indicated. Recurrence of endometrial hyperplastic processes serves as a basis for revising the management tactics. If the patient has received hormonal therapy in full, the question of ablation (in the absence of pathology in the ovaries) or hysterectomy should be raised.
Difficulties in patient management are presented by patients who underwent ablation or endometrial resection, after which synechiae may occur in the uterine cavity. Ultrasound examination of these patients should be performed by a specialist who is proficient in interpreting the echographic signs of synechiae. However, the presence of bloody discharge in these patients serves as an indication for hysteroscopy and separate diagnostic curettage of the uterine mucosa in a specialized gynecological institution.
More information of the treatment

