Medical expert of the article
New publications
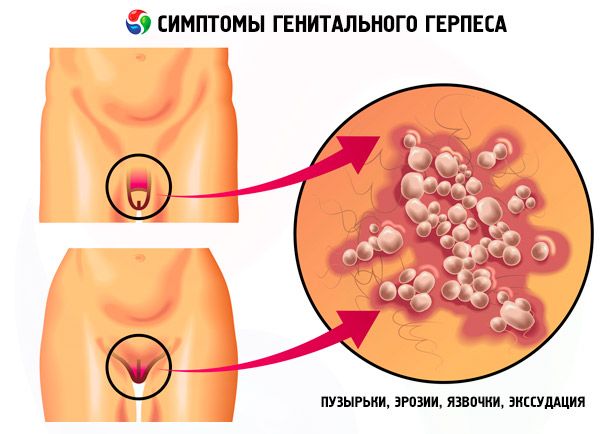
Genital herpes in women
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Genital herpes is caused by two serotypes of the herpes simplex virus: HSV-1 and HSV-2; HSV-2 is most common.
The herpes simplex virus causes pathology of pregnancy and childbirth, often leads to "spontaneous" abortions and death of the fetus or causes generalized infection in newborns. A connection between genital herpes and cervical cancer is noted.
Causes genital herpes in women
The causative agent is the Herpes simplex virus type 1 and 2 (HSV-1 and HSV-2) which causes an infection characterized by lifelong carriage of the virus and its periodic reproduction, leading to the development of a clinical relapse, or proceeding asymptomatically. The recurrence rate of HSV-2 is very high (in 98% of patients).
Ways of transmission of genital herpes:
- contact:
- direct contact (household, sexual);
- indirect contact (household items, dishes, toys, medical instruments);
- airborne;
- transplacental (from mother to fetus and during passage through the birth canal);
- parenteral (organ and tissue transplantation, artificial insemination with infected donor sperm).
About 50% of primary genital herpes is caused by HSV-1 and is transmitted by orogenital contact. Self-infection with existing HSV-1 (orolabial) is very rare. Asymptomatic transmission of the virus is possible (especially HSV-2).
The prevalence of this virus varies among different population groups. From 8 to 83% of patients in antenatal clinics have antibodies to the herpes virus (seropositive). Among prostitutes, the frequency of detection of antibodies is from 75 to 96%, and among blood donors - from 5 to 18%. According to serological studies conducted in various countries, the prevalence of HSV-2 in pregnant women ranges from 6 to 55%, and the prevalence of HSV-1 is 50–70%. 75% of seropositive people have never had any symptoms.
Pathogens
Symptoms genital herpes in women
The incubation period ranges from 1 to 26 days, with an average of about 7 days.
Genital herpes is characterized by the periodic appearance of lesions on the skin and mucous membranes with varying degrees of severity and active release of HSV, which manifests itself in various clinical forms:
- manifest,
- atypical,
- abortive,
- subclinical.
The manifest form of recurrent genital herpes is characterized by the typical development of herpetic elements in the lesion. Constant symptoms of genital herpes are blisters, erosions, ulcers, exudation, and the recurrent nature of the disease. Patients with genital herpes often complain of malaise, headache, sometimes subfebrile temperature, sleep disturbance, and nervousness. Usually, at the onset of the disease, a burning sensation, itching, and pain in the genital area are noted. The affected area swells slightly, turns red, and then a group of small blisters 2-3 mm in size appear on the hyperemic base.
Among the variants of the atypical form of recurrent genital herpes in women, there are edematous and itchy forms. The lesion may be represented by deep recurrent cracks in the tissues of the labia minora and labia majora, which epithelialize on their own within 4-5 days.
The abortive form of genital herpes usually occurs in patients who have previously received antiviral treatment and vaccine therapy. The lesion in the abortive course bypasses some stages characteristic of the manifest form and can manifest itself as an itchy spot or papule that resolves in 1-3 days.
The subclinical form of genital herpes is usually detected during examination of sexual contacts of patients suffering from STDs or married couples with fertility disorders. This form is characterized by microsymptoms (short-term appearance of superficial cracks on the mucous membrane of the external genitalia, accompanied by slight itching).
Symptoms of genital herpes are directly dependent on the location of the lesion, the intensity of the inflammatory process, the duration of the disease, the body's ability to mount protective immunological responses, and the virulence of the virus strain.
Neonatal herpes
- A rare but serious threat to the child's health.
- Antenatal infection is rare.
- Newborns are most often infected with the herpes virus during passage through the mother's birth canal.
- In newborns born to mothers with a primary infection that occurred immediately before delivery, the risk of developing the disease is increased (more than 50%), regardless of whether the mother's infection was asymptomatic or symptomatic.
- The clinical picture can develop immediately after the birth of the child, but it can also develop 4–6 weeks after birth.
 [ 20 ], [ 21 ], [ 22 ], [ 23 ]
[ 20 ], [ 21 ], [ 22 ], [ 23 ]
Symptoms of herpes infection in newborns
- Generalized herpes infection with damage to the liver, central nervous system and other organs with/without skin lesions (incubation period about 1 week).
- Isolated CNS lesion without cutaneous or visceral manifestations (incubation period 2–4 weeks).
- Lesions of the skin, conjunctiva, and oral mucosa without involvement of the central nervous system or internal organs (incubation period 1–3 weeks). Newborns with only skin lesions may develop neurological complications, so such children should receive parenteral acyclovir.
- Postnatal HSV infection is rare, but possible during primary contact with the mother or another person with herpes infection.
What's bothering you?
Stages
Depending on the location and severity of lesions in patients with genital herpes, three stages are conventionally distinguished:
- Stage I - damage to the external genitalia;
- Stage II - herpetic colpitis, cervicitis and urethritis;
- Stage III - herpetic endometritis, salpingitis or cystitis.
In women, herpetic lesions are usually localized on the labia minora and labia majora, in the area of the vulva, clitoris, vagina, and cervix. Herpetic vesicles form characteristic polycyclic scalloped figures. Subsequently, superficial ulcers covered with a grayish coating form in accordance with the number of former vesicles or a continuous erosion with a smooth bottom and unbroken edges surrounded by a bright red rim. The ulcers are not deep and do not bleed. Herpetic ulcers are sometimes very painful. Ulcers and erosions heal without leaving scars. Herpetic eruptions on the labia minora and vulva in women, in some cases, cause significant swelling of the labia. With herpetic lesions, the cervix is edematous, often eroded. Relapses occur either spontaneously, or after sexual intercourse, or after menstruation. Often, the appearance of genital herpes is provoked by other infections. Herpetic recurrent infection can affect not only the area of the external genitalia, but also the mucous membrane of the vagina, the cervix and penetrate ascendingly into the mucous membrane of the uterus and tubes, urethra and bladder, causing specific damage in them.
Complications and consequences
- Extragenital herpes with nasopharyngeal lesions, ophthalmic herpes.
- Generalized herpesvirus infection.
- In pregnant women, genital herpesvirus infection may increase the risk of neonatal meningitis in the fetus when passing through the mother's birth canal infected with herpes lesions.
Diagnostics genital herpes in women
Laboratory diagnostic methods for genital herpes
- Direct immunofluorescence (DIF) is the detection of viral antigens by treating the material with specific fluorescent antibodies.
- Molecular biological methods (real-time PCR) - detection of DNA virus.
- Isolation of virus in cell culture.
- Serological diagnostics (enzyme-linked immunosorbent assay (ELISA)) is not of decisive importance (about 90% of the Russian population is seropositive). To establish the fact of primary infection in pregnant women, it is necessary to determine IgG, IgM and determine the IgG avidity index. The presence of low-avidity antibodies (avidity index below 30%) indicates an acute, first-time infection.
Material for examination - contents of vesicles and/or discharge from the erosive-ulcerative surface of manifestations on the skin and mucous membranes, in asymptomatic forms - scraping of the epithelium of the urethra and/or cervical canal. For serological examination, blood is taken from a vein.
The material must be collected during the period of virus isolation: during primary infection it lasts about 12 days, during relapses - about 5 days.
If complications develop, consultation with related specialists is required.
Procedure for a doctor to follow when a diagnosis of genital herpesvirus infection is established
- Informing the patient about the diagnosis.
- Providing information about the patient's behavior. Genital herpes is a recurrent and incurable infection. Therefore, counseling is considered an essential part of patient management. All patients with genital herpes and their sexual partners should be aware of their chronic disease.
- Counseling patients with genital herpes.
- It is necessary to explain the nature of the disease, focusing on the recurrent nature of the disease, frequent asymptomatic course and sexual transmission. Sexual transmission is possible with asymptomatic course, in the absence of any damage. In this case, it is necessary to discuss with the patient measures to prevent infection.
- Inform the patient that during the period of rashes it is necessary to abstain from sexual activity and to inform the sexual partner about the presence of genital herpes. During sexual relations with a new sexual partner it is necessary to use a condom.
- Condoms are not effective enough to prevent the transmission of herpes virus infection, as other localization of damage or asymptomatic progression is possible, and there is a high risk of transmission of infection by the orogenital route. Other methods of safe sex should be discussed with the patient.
When recommending long-term condom use to monogamous couples, it is important to weigh the pros and cons.
- Discuss the risk of neonatal infection with your patients, including men. Women with genital herpes should be advised to report it at pregnancy registration, which will ensure monitoring (especially for herpes infection) throughout pregnancy.
- Patients with a primary episode of genital herpes should be advised to undergo short-term antiviral therapy to reduce the duration of the rash, as well as long-term suppressive antiviral therapy to reduce the number of relapses.
- Follow-up counseling of patients with genital herpes is an important step in patient management.
- Collection of sexual anamnesis.
- Detection and examination of sexual contacts is carried out depending on the clinical manifestations of the disease and the expected period of infection - from 15 days to 6 months. A patient with genital herpes should inform his sexual partner about the diagnosis so that he knows the risk in case of infection and can help the partner if the disease develops.
Patient education
Patient education should focus on measures to prevent infection of sexual partners.
What do need to examine?
What tests are needed?
Who to contact?
Treatment genital herpes in women
Treatment of genital herpes involves the administration of antiviral drugs (Acyclovir (Zovirax), Famciclovir (Famvir), Valaciclovir (Valtrex). They:
- They speed up the healing process of ulcers.
- Reduces the severity, intensity and duration of symptoms.
- Reduce the frequency of disease recurrence.
- Minimize the risk of transmission of the herpes simplex virus.
The therapy lasts from 7 to 10 days.
More information of the treatment
Prevention
Preventive measures for genital herpes are the same for all STIs. To prevent the development of herpes infection in newborns - with primary clinically expressed infection in the mother before childbirth (presence of vesicular rashes in the genital tract), a cesarean section is indicated.

