Medical expert of the article
New publications
Gastrectomy
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
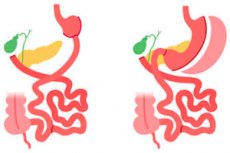
A gastrectomy is a surgical procedure in which some or all of the stomach tissue is removed. Gastrectomy can be performed for different reasons and in different amounts depending on medical necessity. Here are a few types of gastrectomy:
- Partial gastrectomy: In this procedure, only the upper part of the stomach is removed. This may be necessary if there is a tumor or ulcer in this area. A partial gastrectomy preserves most of the stomach and allows the digestive system to function normally.
- Gastrectomy with partial stomach removal: This procedure involves removing part of the stomach and connecting the remaining part to the esophagus or small intestine. It may be performed for stomach cancer or other diseases that affect this organ.
- Gastrectomy with complete removal of the stomach (complete gastrectomy): In this case, the entire stomach is removed and the esophagus is connected to the small intestine. This procedure may be necessary in cases of stomach cancer or other serious stomach abnormalities.
Gastrectomy can have different effects on patients, including changes in digestion and eating ability. People who have had a gastrectomy may need a special diet and medical supervision after surgery. This procedure is usually performed for serious stomach conditions and may improve patient health in certain cases. [1]
Indications for the procedure
This surgery may be performed for a variety of indications, including the following:
- Stomach Cancer: Gastrectomy is often used as a treatment for stomach cancer. Depending on the stage of the cancer, only the tumor or even the entire stomach may be removed.
- Polyps and precancerous conditions: Gastrectomy may be recommended if precancerous conditions or large polyps in the stomach that cannot be removed by other methods are detected.
- Obesity: Gastrectomy can be performed as a treatment for obesity in patients with a high body mass index (BMI). This procedure reduces the size of the stomach, which can lead to restricted food intake and weight loss.
- Obesity with comorbidities: Gastrectomy may also be recommended for obese patients with comorbidities such as type 2 diabetes mellitus or arterial hypertension, which may improve after weight loss.
- Complications of stomach ulcers: In some cases where stomach ulcers cause complications such as bleeding or perforation, a gastrectomy may be required.
- Gastroparesis: Gastrectomy may sometimes be used to treat gastroparesis, a condition in which the motor function of the stomach is reduced, which can cause severe symptoms.
Gastrectomy is a serious surgical procedure and the decision to perform it should be made individually by a physician based on medical indications and discussion with the patient.
Preparation
Preparation for gastrectomy plays a key role in the success and safety of the surgery and subsequent recovery. Here are the basic steps of preparation:
-
Consultation with a physician:
- The first step is a consultation with the doctor who will perform the surgery. At this appointment, you can discuss your medical history, current health status, symptoms, and wishes for surgery.
-
Examination and tests:
- You may be ordered a variety of blood and urine laboratory tests, including general blood count, biochemistry, coagulogram, and others.
- Chest X-ray and eCG to evaluate the lungs and heart.
- Gastrofibroscopy or gastric endoscopy may be needed to examine the stomach in more detail.
-
Stomach preparation:
- You may be advised to eat a liquid or semi-liquid diet for a few days before the operation. This will help reduce the volume of stomach contents and make the surgery safer.
-
Withdrawal fromcertain medications:
- Your doctor may ask you to temporarily stop taking certain medications that may affect your blood clotting or affect other aspects of the surgery.
-
Preparation for anesthesia:
- If general anesthesia will be used, you may need to fast for a short time (no food or water) before surgery. This will be discussed with the anesthesiologist.
-
Psychological support:
- Gastrectomy can affect the patient's psychological well-being. It is important to discuss your expectations and concerns with a psychologist or psychiatrist, if appropriate.
-
Plan for the post-operative period:
- Prepare yourself for the special diet and care you will need after a gastrectomy. Discuss this with your doctors and dietitians.
-
Support for family and loved ones:
- The support of family and friends plays an important role in the preparation and post-operative rehabilitation process.
-
Consent Signing:
- You will be given informed consent for the surgery, which implies that you fully understand the risks and consequences of the surgery.
-
Following medical advice:
- It is important to follow all instructions from your doctor and anesthesiologist, especially in the days leading up to surgery.
Preparing for a gastrectomy requires care and discipline. It is important to discuss all aspects of the surgery and recovery plan with your medical team to be prepared for the procedure and minimize risks.
Technique of the gastrectomies
The following is general information about the technique for performing a gastrectomy:
- Preparation for surgery:
- The patient is given a pre-operative health assessment including blood tests, electrocardiogram and other necessary examinations.
- Prior to surgery, preparation such as food and fluid restriction may be necessary to reduce the risk of complications.
- Anesthesia: The patient is given general anesthesia to ensure insensibility during surgery.
- Access to the stomach: The surgeon makes small incisions in the stomach or one large incision, depending on the type of gastrectomy (laparoscopic or open). Laparoscopic gastrectomy is performed using tiny instruments and a video camera inserted through small incisions.
- Stomach Isolation: The surgeon isolates the stomach from the rest of the abdomen so that the removal can be performed.
- Gastric removal: The stomach itself is removed. The method of removal depends on the type of gastrectomy:
- In a total gastrectomy (gastrectomy with complete gastric resection), the stomach is completely removed.
- In a vertical gastric resection (gastrectomy involving part of the stomach), only part of the stomach is removed.
- Revision: After the stomach is removed, the surgeon examines the surrounding organs and tissues to make sure there are no complications or leaks.
- Digestive system reconstruction: After the stomach is removed, a new way of digestion is created. This may involve connecting the esophagus directly to the intestine (esophago-jejadenoanastomosis) so that food can pass from the esophagus to the intestine.
- Wound closure: The surgeon closes abdominal incisions or skin sutures after a laparoscopic gastrectomy.
- Post-operative care: After surgery, the patient is provided with post-operative care and monitoring to monitor their condition and prevent complications.
Types of gastrectomy
There are several different types of gastrectomy depending on the amount of stomach removal and the site of removal. Here are some of them:
Total gastrectomy
Total gastrectomy is a surgical procedure in which the entire stomach is removed. This surgery can be performed for a variety of medical conditions, including stomach cancer, certain precancerous conditions, and other medical conditions. Here are the main aspects of total gastrectomy:
- Indications: The main indication for total gastrectomy is stomach cancer, especially in cases where the tumor cannot be removed without removing the entire stomach. It may also be performed in cases of severe gastric ulcers or precancerous conditions.
- Procedure: During a total gastrectomy, the surgeon removes the entire stomach. After the stomach is removed, the upper part of the esophagus (esophagus) connects directly to the intestine to allow digestion and passage of food.
- Postoperative period: Patients who have undergone total gastrectomy require special postoperative care and rehabilitation. They must follow a special diet and lifestyle to adapt to the absence of the stomach and the altered digestive system.
- Implications: Total gastrectomy can have significant consequences for the patient, including changes in eating behavior, nutrient absorption, and adaptation to a new lifestyle. Patients may also be subject to regular medical evaluations and follow-up after surgery.
- Possible complications: As with any surgical procedure, total gastrectomy is not without risks and complications. These can include infections, bleeding, digestive problems, and other complications. However, doctors try to minimize the risks and ensure the patient's well-being as much as possible.
Total gastrectomy is a complex operation that is performed only in cases with serious medical indications. The decision to perform this procedure should be made by a doctor based on a detailed examination and assessment of the patient's condition. [2]
Gastrectomy with lymphodissection.
A gastrectomy with lymphatic dissection is a surgical procedure in which the stomach is removed (complete gastrectomy or partial gastrectomy) and a lymphatic dissection is performed, which is the removal of lymph nodes in the surrounding areas. This procedure is often performed in cases of stomach cancer to remove the tumor and prevent cancer cells from spreading to surrounding tissues and lymph nodes.
Here are the key points related to gastrectomy with lymphodissection:
- Indications: The main indication for gastrectomy with lymphatic dissection is gastric cancer. This procedure may also be performed in cases of esophageal cancer where the upper part of the stomach may need to be removed.
- Types of gastrectomy: There are several types of gastrectomy, including total gastrectomy (removal of the entire stomach) and partial gastrectomy (removal of only part of the stomach). The type chosen depends on the spread of the tumor and the patient's individual characteristics.
- Lymphatic dissection: Lymphatic dissection involves removing lymph nodes in areas close to the stomach and esophagus. This is done to identify and remove cancer cells that may have spread in the lymphatic system.
- Postoperative recovery: After gastrectomy with lymphodissection, patients may require special diet and rehabilitation. Gradual introduction of food and lifestyle changes will help patients adapt to the new digestive environment.
- Medical monitoring: Patients who have undergone gastrectomy require ongoing medical monitoring to monitor their condition and respond to any complications.
Gastrectomy with lymphodissection is a complex and serious surgical procedure and requires an experienced surgeon and a well-equipped medical team. It can be an effective treatment for gastric cancer, especially in the early stages, but it has its own risks and requires careful attention to postoperative rehabilitation and patient care. [3], [4]
Subtotal gastrectomy
Subtotal gastrectomy is a surgical procedure in which part of the stomach, but not the entire stomach, is removed. In this procedure, the surgeon removes the upper part of the stomach (usually the greater curvature and part of the body of the stomach) while leaving the lower part of the stomach, which connects to the duodenum, intact. Subtotal gastrectomy may be performed for a variety of medical reasons, including stomach cancer, ulcers, polyps, or other conditions that affect the upper part of the stomach. [5]
Important aspects of subtotal gastrectomy:
- Upper stomach removal: The surgeon removes the upper part of the stomach, which may include the greater curvature, the body of the stomach and sometimes the upper part of the anatomical curvature.
- Preservation of the lower part of the stomach: The lower part of the stomach, called the anatomical curvature (gastroduodenal junction), remains intact. This allows digestion to continue and the passage of food through the stomach to be controlled.
- Reconstruction of the digestive system: After the upper part of the stomach is removed, a connection is made between the remaining stomach and the esophagus or intestines. This can be done using a variety of methods, including anatomical anastomosis (Roux anastomosis) or other variations.
- Postoperative care and recovery: After subtotal gastrectomy, the patient requires special postoperative care and diet. Food can pass through the rest of the stomach and esophagus into the intestines, but this may require changes in diet and the way food is eaten.
Subtotal gastrectomy can be an effective treatment for certain upper stomach conditions, but it can also have an impact on the way a patient digests and eats. Therefore, it is important to discuss all aspects of this surgery with your surgeon and to get advice on post-operative care and diet for best results. [6]
Distal gastrectomy
Distal gastrectomy is a surgical procedure in which the lower part of the stomach is removed while the upper part of the stomach remains. This surgery may be performed for a variety of medical reasons, including treatment of stomach cancer, stomach ulcers, or certain other upper gastrointestinal diseases. [7]
The distal gastrectomy process usually involves the following steps:
- Incision: The surgeon makes an incision in the patient's abdomen to access the stomach and surrounding structures.
- Lower stomach removal: The surgeon removes the lower part of the stomach, which often includes the antral portion of the stomach. This is removed to remove cancerous tumors or to treat other conditions.
- Creating an anastomosis: After removing part of the stomach, the surgeon creates an anastomosis between the remaining upper part of the stomach and the esophagus or duodenum. This allows the normal passage of food and digestion to continue.
- Incision closure: The created anastomosis is closed with surgical sutures or other methods to ensure a tight connection.
Distal gastrectomy can be performed either as an open surgical procedure with a large incision on the abdomen or using laparoscopic techniques (minimally invasive surgery), which can shorten the recovery period and reduce complications after surgery.
After distal gastrectomy, patients may require dietary and lifestyle changes and should follow the medical team's recommendations to successfully adjust to their new environment. [8]
Combined gastrectomy
A combined gastrectomy is a surgical procedure that involves removal of the stomach (gastrectomy) and simultaneous resection or removal of other organs or tissues in the surrounding area. This may be necessary when cancer or other stomach disease has spread to neighboring structures or organs.
The type of combined gastrectomy can vary depending on the location and stage of the tumor and other factors. Here are some examples of combined gastrectomies:
- Gastrectomy with lymphatic dissection: This is a combined procedure in which, in addition to removing the stomach, the lymph nodes in the surrounding area are also removed. This is done to determine the extent of the cancer and to prevent it from spreading further.
- Combined gastrectomy with liver resection: If stomach cancer has spread to the liver, it may be necessary to remove part of the liver along with the stomach.
- Combined gastrectomy with spleen resection: If the tumor has spread to the spleen, it may be necessary to remove the spleen along with the stomach.
- Combined gastrectomy with resection of other organs: In some cases, the tumor may spread to other organs or tissues such as the liver, pancreas, intestines, or others. In such cases, a combined gastrectomy with removal of the relevant organs is performed.
Combined gastrectomies are usually performed in medically complex cases, and they require a longer postoperative recovery period and special attention from the medical team. Patients who have undergone these procedures must receive long-term medical follow-up and follow medical recommendations for successful rehabilitation.
Laparoscopic gastrectomy.
Laparoscopic gastrectomy is a surgical procedure in which the stomach is removed using a laparoscopic (minimally invasive) technique. Laparoscopy allows surgeons to perform the operation through small incisions in the abdominal wall, using special instruments and a camera to visualize internal organs. [9]
Here are the main characteristics of laparoscopic gastrectomy:
- Indications: The main indication for laparoscopic gastrectomy is gastric cancer or other gastric diseases that require removal of this organ. The laparoscopic technique can be used for early to mid-stage cancer.
- Benefits: Laparoscopic gastrectomy has several advantages over open (traditional) surgery, including less risk of infection, faster recovery, less pain after surgery, and shorter hospitalization.
- Operation: During a laparoscopic gastrectomy, the surgeon makes several small incisions in the abdominal wall and inserts laparoscopic instruments, including a camera, to navigate and perform the operation. The stomach is removed through one of the incisions.
- Rehabilitation: After laparoscopic gastrectomy, patients may require special diet and rehabilitation to adapt to the altered anatomy and digestive method. However, recovery is usually faster than after open surgery.
- Medical follow-up: After surgery, patients undergo regular medical follow-up to monitor their condition and watch for possible complications.
Laparoscopic gastrectomy requires an experienced surgeon and a well-equipped operating room. It has become the preferred method for many patients because it is usually associated with faster recovery and fewer complications than traditional open surgery. [10]
Sleeve gastrectomy (gastrectomy with gastric pear formation)
Sleeve Gastrectomy is a surgical procedure used to treat obesity and reduce the size of the stomach in order to reduce food intake and control appetite. During a sleeve gastrectomy, the surgeon removes most of the stomach, turning it into a narrow vertical sleeve-shaped organ. This method has become popular in bariatric surgery and can help patients achieve significant weight loss. [11]
Basic steps and characteristics of sleeve gastrectomy:
- Removal of part of the stomach: The surgeon creates a vertical incision in the patient's abdomen and access to the stomach. Most of the stomach is then removed, leaving only a narrow vertical sleeve. The removed portion of the stomach is usually about 75-80% of its original volume.
- Pyloric valve preservation: The pyloric valve (the valve that separates the stomach and duodenum) is usually preserved to allow normal movement of food from the stomach to the intestines.
- Reduced stomach volume: After surgery, the stomach has a significantly smaller volume, which results in smaller food portions and less appetite. This helps patients to feel satiety faster and reduce calorie intake.
- Effect on appetite and hormonal balance: Sleeve gastrectomy can also affect the hormonal balance in the body, which helps control appetite and metabolism.
Sleeve gastrectomy is considered a relatively safe procedure for many obese patients. It can help achieve significant weight loss and improve obesity-related medical problems such as type 2 diabetes mellitus, arterial hypertension and obstructive sleep apnea. However, like any surgical procedure, sleeve gastrectomy is not without risks and requires careful medical monitoring before and after surgery.
Patients considering sleeve gastrectomy should have a consultation with a bariatric surgeon to discuss the indications, risks and benefits of the procedure, and prepare for lifestyle and dietary changes after surgery.
Extended gastrectomy
An extended gastrectomy is a surgical procedure that removes most or all of the upper part of the stomach, and sometimes even part of the esophagus and other nearby structures. This surgery may be performed in cases of stomach cancer when the tumor is so large or has spread so far that radical removal of the affected tissue is required.
The process of an extended gastrectomy includes the following steps:
- Incision: The surgeon makes an incision in the patient's abdomen to access the stomach, esophagus, and other structures.
- Removal of the stomach and other tissues: The surgeon removes most or all of the upper part of the stomach and sometimes part of the esophagus, lymph nodes, and other affected tissues.
- Creating an anastomosis: After removing the diseased tissue, the surgeon creates an anastomosis between the remaining part of the esophagus and the intestinal tract to allow normal passage of food and digestion.
- Incision closure: The created anastomosis is closed with surgical sutures or other methods to ensure a tight connection.
An extended gastrectomy can have significant consequences for the patient, including lifestyle and dietary changes. After surgery, patients may require specialized nutrition and close medical supervision. Surgical removal of a large portion of the stomach is considered a radical measure and is discussed carefully with the patient based on medical indications and individual case characteristics.
Palliative gastrectomy
Palliative gastrectomy is a surgical procedure performed to relieve symptoms and improve the quality of life of patients with advanced gastric cancer or other incurable conditions when radical treatment is no longer effective or possible. It is not aimed at a radical cure, but at alleviating symptoms and providing comfort to patients. [12]
The primary goals of palliative gastrectomy include:
- Symptom Reduction: Gastrectomy can reduce symptoms such as abdominal pain, nausea, vomiting, dysphagia (difficulty swallowing) and other discomfort that often accompanies advanced stomach cancer.
- Improving digestion: Removing part or all of the stomach can help restore normal digestion when a tumor in the stomach interferes with the normal passage of food.
- Improved quality of life: Palliative gastrectomy can improve patients' quality of life, allowing them to better manage their symptoms and continue to eat normally.
- Prolonging life: In some cases, palliative gastrectomy can extend the patient's remaining time of life by improving their general condition and allowing them to continue medical treatment or symptomatic therapy.
It is important to note that palliative gastrectomy can be a complex operation and it is not appropriate for all patients with advanced gastric cancer or other similar conditions. The decision to undergo palliative gastrectomy should be carefully considered and based on each patient's individual circumstances, overall health and expectations of treatment. Before palliative gastrectomy is performed, it is important to have a detailed consultation with the medical team and discuss all aspects of the operation, risks and benefits to the patient. [13]
Davidoff gastrectomy.
Davydov gastrectomy is a surgical procedure that is performed to treat stomach cancer, especially when the tumor is located in the distal (lower) part of the stomach. This procedure was developed by Soviet surgeon Andrei Davydov and has its own characteristics.
The Davydov Gastrectomy procedure includes the following steps:
- Stomach removal: During surgery, part or all of the stomach is removed, depending on how far the cancer has spread and medical reasons. The lower (distal) part of the stomach is most often removed.
- Esophageal resection: The upper part of the esophagus (esophagus) is resected and only the lower part remains, which connects to the intestine.
- Creating a gastrointestinal anastomosis: The remaining part of the esophagus (esophagus) connects to the small intestine (duodenum) to allow food to pass into the intestines and digestion.
- Lymph node removal: The surgeon also removes lymph nodes in the surrounding area to determine how far the cancer has spread and to prevent it from spreading further.
Davidoff gastrectomy may be chosen when stomach cancer is located in the lower part of the organ and can be removed, preserving part of the upper stomach and esophagus. This preserves more normal digestion and quality of life in patients after surgery.
As with other types of gastrectomy, Davidoff Gastrectomy is a complex surgery and patients require special post-operative care and rehabilitation afterward.
Gastrectomy anastomoses
During a gastrectomy, especially a complete gastrectomy (removal of the entire stomach), special anastomoses are created to restore normal digestion and the passage of food from the esophagus to the rest of the gastrointestinal tract. Here are a few types of anastomoses that can be created during a gastrectomy:
Esophago-duodenal anastomosis (EDA)
This is a type of anastomosis that is created during surgery of the upper esophagus and duodenum. This type of anastomosis connects the end of the esophagus to the first section of the duodenum (duodenum). The creation of an EDA can be used in a variety of surgical procedures, including gastrectomy (removal of the stomach) and correction of pathologies of the esophagus and upper gastrointestinal tract.
Examples of instances where an EDA may be needed:
- Total gastrectomy: When the entire stomach is removed (total gastrectomy), the end of the esophagus is connected to the first part of the duodenum by an EDA. This creates a new pathway for food to pass from the esophagus to the intestine.
- Esophageal surgery: In some cases, when defects or tumors in the esophagus need to be repaired, an EDA may need to be created to restore the normal passage of food.
- Correction of structural abnormalities: EDA can be used to correct structural abnormalities such as stenoses (narrowings) or other abnormalities of the upper esophagus and duodenum.
- Gastrointestinal bypass procedures: In some obesity treatments, such as Roux-en-Y gastrointestinal bypass, an EDA is created as part of the procedure to redirect the flow of food.
Creating an EDA is a complex surgical technique that requires an experienced surgeon. After surgery, patients may require a special diet and medical monitoring to ensure successful recovery and adaptation to altered digestion.
Esophago-gastric anastomosis (EJA).
This is a surgical procedure that connects the esophagus (esophagus) to the stomach after removal of part or all of the stomach or other upper gastrointestinal surgery. This anastomosis is created to restore the normal passage of food from the esophagus to the stomach, allowing digestion to continue.
The process of creating an esophago-gastric anastomosis can vary depending on the specific surgical procedure and individual patient characteristics, but it typically involves the following steps:
- Esophagus and stomach incision: The surgeon makes incisions at the ends of the esophagus and stomach at the point where the connection will be created.
- Creating an anastomosis: Aftermaking incisions in the esophagus and stomach, the surgeon joins the ends of these organs so that food can pass freely from the esophagus to the stomach.
- Incision closure: The created anastomosis is closed with surgical sutures or special medical devices to ensure a tight connection.
Esophago-gastric anastomosis can be part of various surgical procedures such as gastric resection for gastric cancer, correction of esophageal defects, bariatric surgery and others. This procedure plays an important role in restoring digestive function after such surgeries and ensures that patients are able to continue eating and digesting normally.
Esophago-gastric anastomosis with Roux-en-Y (EJA with Roux-en-Y)
Roux-en-Y anastomosis (Roux-en-Y anastomosis) is one method of repairing the digestive tract after a gastrectomy (removal of the stomach). This method is named after French surgeon Cesar Roux, who first described it. Roux anastomosis is often used during gastrectomy to treat stomach cancer or other medical conditions that require removal of part of the stomach. Here are the basic steps and characteristics of Roux anastomosis:
- Gastric removal: First, part or all of the stomach is removed depending on the medical condition. The surgeon can remove the large curvature of the stomach (partial gastrectomy) or the entire stomach (complete gastrectomy).
- Creating a gastrointestinal anastomosis: The surgeon creates a connection between the esophagus (after removing the stomach) and the small intestine. This is done by using a part of the intestine called the distal or far end. This procedure creates a gastrointestinal anastomosis that allows food to pass into the intestine.
- Roux limb (Roux limb): The far end of the small intestine (distal end) is cut off and an outlet (roux) is created to attach to the gastrointestinal anastomosis. The roux is a short loop of intestine that points down and to the left of the anastomosis.
- Creation of a biliopancreatic diverticulum: In rare cases, a biliopancreatic diverticulum can be created, which is a manual diversion of bile and pancreatic juices from the main part of the intestine (alimentary anastomosis) into a separate loop of intestine. This can help prevent reflux of bile and juices into the esophagus.
Roux anastomosis allows food to enter the intestine, bypassing the removed stomach, and continue digestion. This method can reduce the risk of reflux of bile and pancreatic juices into the esophagus, which can be a problem after gastrectomy.
Duodeno-gastric anastomosis (DDA)
This is a type of surgical anastomosis that connects the upper part of the stomach to the first part of the duodenum (duodenum). This anastomosis can be created in a variety of surgical procedures that involve altering or reconstructing the stomach and esophagus.
Examples of situations where a duodeno-gastric anastomosis may be necessary:
- Gastric surgery: In surgical procedures such as gastric cavity resections (partial removal of the stomach) or correction of gastric abnormalities, DDA may be used to restore the normal passage of food from the upper stomach to the duodenum.
- Duodenal atresia: Newborns with duodenal atresia, which is a congenital malformation of the duodenum, may require a DDA to restore normal passage of food.
- Gastrointestinal bypass: In some surgical treatments for obesity, such as the biliopancreatic bypass (BPD) or Scopinaro procedure, a DDA can be created to redirect the flow of food and gastric juices.
Creating a DDA is a major surgical procedure that requires an experienced surgeon and careful planning. After surgery, patients must follow a special diet and medical guidelines to ensure successful recovery and adaptation to the altered digestion.
Brown anastomosis for gastrectomy.
A Brown anastomosis (also known as a Brown duodenojejedenostomy or duodenojejunal anastomosis) is a surgical procedure that creates a connection between the remaining portion of the esophagus and duodenum (duodenum) after gastrectomy or other surgeries on the stomach and upper gastrointestinal tract.
This type of anastomosis can be performed when the stomach has been removed or there are problems with its function and it is necessary to allow food to pass from the esophagus to the intestinal tract. The Brown anastomosis allows food to pass from the esophagus to the duodenum, bypassing the missing stomach.
The procedure includes the following steps:
- Esophageal incision: The surgeon makes an incision at the end of the esophagus.
- Creating an anastomosis: A connection is created between the end of the esophagus and the duodenum, allowing food to pass freely into the intestinal tract.
- Closure of the incision: The created anastomosis is closed with surgical sutures or other methods.
Brown anastomosis helps to restore digestive function and ensure normal digestion after surgical removal of the stomach or other upper gastrointestinal surgeries. This procedure can be part of a comprehensive surgical treatment for gastric cancer or other pathologies where the food pathway needs to be rerouted.
These anastomoses are created by the surgeon to allow normal digestion and passage of food into the intestine after the stomach has been removed or altered. The specific type of anastomosis chosen depends on the surgical procedure, the goals of the surgery, and the patient's condition. After surgery, it is important to strictly follow the recommendations of doctors and nutritionist for successful recovery and adaptation to the new digestive process.
Contraindications to the procedure
Contraindications may include the following conditions or circumstances:
- General impairment: If the patient is critically ill or has multiple serious comorbidities, gastrectomy may not be acceptable because of the high risk to life.
- Inability to tolerate surgery: Some patients may have other factors that make surgery impossible or too risky.
- Late Stages of Gastric Cancer: In some cases where stomach cancer is in advanced stages and has already metastasized to other organs, a gastrectomy may be futile and patients may be offered other treatments or palliative care.
- Esophageal or gastric obstruction: If the esophagus or stomach is blocked or has intractable obstructions, gastrectomy may not be possible.
- Psychological or social problems: Some patients may have psychological or social problems that can affect the success and postoperative recovery.
The decision-making process for gastrectomy should be thorough and include an evaluation of all medical and psychological factors. The decision to operate is usually made by the physician based on clinical evaluation and medical indications. Patients should discuss all of their questions and concerns with their physician in order to make an informed decision about gastrectomy.
Consequences after the procedure
The consequences and effects after gastrectomy can vary greatly depending on the type of procedure (total or partial gastrectomy), medical conditions, and individual patient characteristics. Here are some of the common effects that can occur after gastrectomy:
- Changes in eating behavior: After gastrectomy, patients may experience changes in appetite and ability to consume large portions of food. This can lead to rapid satiety and weight loss.
- Reflux and digestive problems: Post-gastrectomy patients may experience increased reflux of stomach contents into the esophagus, which can cause heartburn and other digestive problems.
- Nutrient deficiencies: After gastrectomy, patients may need to pay special attention to nutrition and nutrient absorption because the stomach that is removed plays an important role in digestion and absorption of certain vitamins and minerals.
- Lifestyle changes: Patients may need to make lifestyle changes, including eating smaller meals more often and eating protein foods.
- Health risks: Gastrectomy can reduce the risk of certain diseases, such as diabetes and hypertension, if it is performed to treat obesity. However, it may also increase the risk of deficiencies in certain vitamins and minerals.
- Psychological aspects: Gastrectomy can have an impact on the patient's psychological well-being, as changes in eating behavior and appearance can cause stress and adaptive difficulties.
It is important to realize that each case is different and outcomes may vary. After gastrectomy, patients usually require careful medical monitoring and support to minimize risks and maximize the benefits of the procedure. Patients are also advised to follow the recommendations of physicians and dietitians for successful rehabilitation and health maintenance after gastrectomy.
Anemia after gastrectomy
This is a common complication of this surgical procedure. It can occur due to a number of factors related to changes in the digestive system and nutrient absorption after stomach removal. [14] Here are some of the possible causes of anemia after gastrectomy:
- Iron deficiency: Gastrectomy can lead to decreased absorption of iron from food, as the stomach plays an important role in this process. This can cause iron deficiency anemia. [15]
- Vitamin B12 deficiency: The stomach is also necessary for the absorption of vitamin B12 from food. After gastrectomy, patients may require external administration of this vitamin, and a deficiency can cause anemia.
- Folic Acid Deficiency: There may also be decreased absorption of folic acid after gastrectomy, which may contribute to anemia.
- Surgical complications: Compl ications after surgery, such as bleeding or infections, can also lead to anemia.
- Dietary Restrictions: Patients who have undergone gastrectomy are often recommended a special diet and may not receive adequate nutrients due to a reduced ability to consume food.
To prevent or treat anemia after gastrectomy, it is important to work closely with your medical team and follow the recommendations for diet and vitamin and mineral intake. Treatment may include taking iron, vitamin B12, folic acid, and other essential micronutrients. Regular blood tests and consultations with your doctor will help to monitor your health and identify and treat anemia in a timely manner.
Esophageal erosion after gastrectomy
It is a condition in which the esophageal mucosa undergoes inflammation and damage that can be caused by a variety of factors. Gastrectomy, in which part or all of the stomach is removed, can alter the anatomy of the digestive system and create conditions that contribute to the development of esophageal erosion. Below are some of the possible causes and factors that may contribute to the development of esophageal erosion after gastrectomy:
- Reflux of gastric contents: After gastrectomy, especially total gastrectomy, the esophagus may experience increased reflux (backflux) of gastric contents upward toward the esophagus. This can cause irritation and damage to the esophageal mucosa, leading to erosions.
- Hydrochloric Acid Deficiency: Post-gastrectomy patients may have a lack of hydrochloric acid in the stomach, which can alter the chemical conditions in the esophagus and increase the risk of erosions.
- Changes in eating behavior: Patients after gastrectomy may change their eating behavior and diet, which can affect the condition of the esophageal mucosa. For example, increased consumption of acidic foods or snacking between meals may contribute to the development of erosion.
- Use of Uncontrolled Medications: Uncontrolled or improper use of medications, such as certain anti-inflammatory drugs or aspirin, may increase the risk of developing esophageal erosion.
Treatment for esophageal erosion after gastrectomy may include changing your diet and eating behavior, taking antacids or other medications that can reduce the acidity of stomach contents, and consulting with a gastroenterologist for more detailed evaluation and treatment. It is important to discuss any symptoms or concerns with your doctor to get appropriate treatment and prevent further damage to the esophagus.
Complications after the procedure
As with any surgery, it can cause a variety of complications. Complications after a gastrectomy may include:
- Infections: Infections at the surgical site can be a serious complication. It is important to follow the rules of asepsis and antisepsis both before and after surgery.
- Bleeding: There may be bleeding from vessels that have been crossed during surgery. This may require additional surgical intervention.
- Bloodclots: After surgery, the risk of blood clots (blood clots) may increase. This can cause serious complications such as pulmonary embolism or stroke.
- Vitamin and Mineral Deficiency Syndrome: Because gastrectomy alters the digestive process, patients may experience deficiencies of important vitamins and minerals such as vitamin B12, iron, calcium, and others. This can lead to anemia and other health conditions.
- Gastric reflux: Patients after gastrectomy may develop reflux of gastric contents into the esophagus. This can cause discomfort and inflammation.
- Dumping syndrome: After gastrectomy, some patients may experience dumping syndrome, which includes symptoms such as nausea, vomiting, diarrhea, and weakness after eating foods, especially those rich in sugar.
- Eating Difficulties: After gastric removal, patients may have difficulty eating and digesting food. This may require a change in diet and eating patterns.
- Psychological aspects: Gastrectomy can affect the patient's psychological well-being, causing depression, anxiety, or other emotional problems.
It is important to note that complications after gastrectomy can vary depending on the type of surgery and the patient's individual characteristics. The surgeon and medical team should provide the patient with detailed information about possible complications and how to prevent and treat them. Following medical advice and regular check-ups can help reduce the risk of complications and ensure a successful recovery after gastrectomy. [16]
Care after the procedure
After a gastrectomy procedure, specialized care is required to help the patient recover faster and adapt to the digestive changes. Here are some basic aspects of care after gastrectomy:
- Diet: After a gastrectomy, patients are usually advised to follow a special diet. Doctors can develop a customized diet plan depending on the type of gastrectomy and the patient's condition. Typically, the introduction of food starts with a liquid diet and then progresses to a soft diet and then to regular food.
- Medications: Patients may be prescribed medications to reduce the risk of infection and facilitate healing. It may also be necessary to take medications to improve digestion, control symptoms, and maintain health.
- Physical activity: A gradual increase in physical activity will help the patient to return to a normal life. Physical therapy can be helpful in regaining strength and maintaining optimal fitness.
- Monitoring: Regular medical monitoring is important to keep track of the patient's condition and detect any complications or side effects after gastrectomy.
- Support and counseling: Patients may need psychological support and counseling to adjust to new diets and lifestyles. Support groups can be useful for sharing experiences and advice with others who have undergone similar procedures.
- Following yourdoctor's instructions: It is important to follow your doctor's instructions and prescriptions to prevent complications and achieve the best possible results after gastrectomy.
- Safety: After a gastrectomy, patients may be more at risk of developing certain conditions such as anemia or vitamin and mineral deficiencies. Doctors may recommend taking special supplements to compensate for these losses. [17]
Nutrition and diet after gastrectomy
Nutrition and diet after gastrectomy depend on the type of surgery (total gastrectomy or partial gastrectomy) and the individual needs of the patient. It is important to discuss dietary recommendations with your doctor or dietitian, as they can be individualized for each case. Here are general guidelines for nutrition after gastrectomy:
- Gradual introduction of food: After surgery, patients usually start with a liquid diet and gradually move on to denser foods. This allows the body to adapt to the new digestive conditions.
- Liquid diet: At this stage, the menu may include broths, liquid soups, fermented milk drinks, low-fat broths and pureed fruits and vegetables.
- Semi-solid diet: Gradually introduce more solid foods such as porridge on water, mashed vegetables and fruits, low-fat cottage cheese puree.
- Soft diet: This stage includes soft foods such as soft chicken, fish, soft fruits and vegetables. Individual meals should be well chewed.
- Balanced nutrition: When dieting after gastrectomy, it is important to provide a balanced diet that includes protein, carbohydrates, fats, vitamins and minerals. Vitamin B12 is often prescribed in supplement form because its absorption may be impaired after gastrectomy.
- Small portions: After a gastrectomy, the stomach is smaller, so it is important to eat small and frequent meals. This helps prevent overstretching of the stomach and discomfort.
- Avoiding certain foods: Some foods may cause discomfort or inconvenience after a gastrectomy, so your doctor may recommend avoiding them. These may include foods that are too fatty, sweet, spicy, or carbonated.
- Weight management: After surgery, patients are sometimes at risk for weight loss due to limited ability to absorb food. It is important to monitor weight and discuss strategies for weight maintenance with your doctor if necessary.
Each patient may have individual differences and limitations, so a dietitian or physician should work to develop a nutrition plan that best fits the needs and capabilities of each individual case.
List of authoritative books and studies related to the study of gastrectomy
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA. 2004 Oct 13;292(14):1724-37.
- Csendes A, Burdiles P, Braghetto I, et al. A Prospective Randomized Study Comparing D2 Total Gastrectomy Versus D2 Total Gastrectomy Plus Splenectomy in 187 Patients with Gastric Carcinoma. Surgery. 2002 May;131(5):401-7.
- Gastric Cancer Surgery: Morbidity and Mortality in Western Countries. Ann Surg Oncol. 2003 Feb;10(2):218-25.
- Stomach Cancer Surgery: New Techniques and Strategies. World J Surg. 1995 Nov-Dec;19(6):765-72.
- Deans C, Yeo MS, Soe MY, et al. Cancer of the Gastric Cardia Is Rising in Incidence in an Asian Population and is Associated with Adverse Outcome. World J Surg. 2011 Nov;35(11):617-24.
- Dikken JL, van Sandick JW, Allum WH, et al. Quality of Care After Surgery for Gastric Cancer in the Netherlands: A Population-based Study. Ann Surg Oncol. 2011 Jun;18(6): 1757-65.
- Karanicolas PJ, Smith SE, Inculet RI, et al. The Impact of Obesity on the Complications of Laparoscopic Nissen Fundoplication. J Gastrointest Surg. 2007 Jun;11(6): 738-45.
- Lee KG, Lee HJ, Yang JY, et al. Comparison of Complications After Laparoscopy-assisted Distal Gastrectomy and Open Distal Gastrectomy for Gastric Cancer Using the Clavien-Dindo Classification. Surg Endosc. 2012 Feb;26(2):1287-95.
- Mohiuddin K, Noura S, Subhani J, et al. Comparative Study of Complications after Laparoscopic and Open Sleeve Gastrectomy. J Coll Physicians Surg Pak. 2017 Nov;27(11):696-699.
- Lee SS, Chung HY, Kwon OK, et al. The Learning Curve for Laparoscopic Gastrectomy for Gastric Cancer. Surg Endosc. 2011 Apr;25(4):1083-90.
Literature
- Chissov, V. I. Oncology / Ed. By V. I. Chissov, M. I. Davydov - Moscow: GEOTAR-Media, 2008. I. Chissov, M. I. Davydov - Moscow: GEOTAR-Media, 2008.
- Saveliev, V. S. Clinical Surgery. In 3 vol. Vol. 1: national manual / Ed. By V. S. Saveliev. С. Savelyev, A. I. Kirienko. - Moscow: GEOTAR-Media, 2008.

