Medical expert of the article
New publications
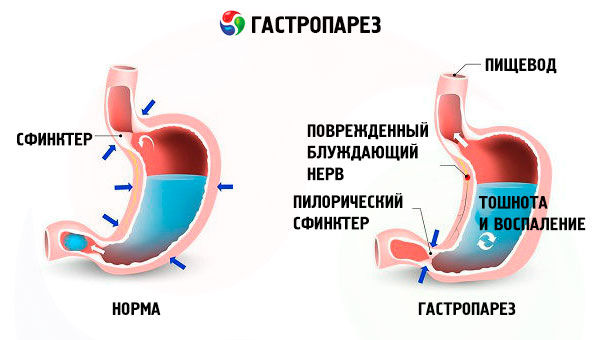
Gastroparesis
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Disruption of the muscular activity of the stomach, which results in a failure in the evacuation function of the stomach, is called gastroparesis. The absence of contractions of the muscles of the stomach leads to the retention of food in the organ, its rotting, the formation of pathogenic flora. All this causes pain in the epigastric region, various disorders in the digestive system. Why does this condition occur?
Epidemiology
It is difficult to determine the exact prevalence of the disease, since at the stage of primary medical care it is difficult to link gastric ailments with the rate of emptying of the organ. However, there is average data that 4% of the planet's inhabitants suffer from this pathology. According to statistics, women are more likely to be affected by the disease than men. In one study, their number was 87% of all observed patients.
Causes gastroparesis
The main causes of gastroparesis are:
- diabetes mellitus;
- diseases of the nervous system ( Parkinson's disease, stroke );
- pancreatitis;
- drug exposure;
- chemotherapy and radiation;
- micronutrient deficiency;
- Damage to the vagus nerve during surgery.
Risk factors
Factors that complicate the natural passage of food from the stomach into the duodenum include:
- infections;
- significant weight loss, anorexia;
- binge eating, in which a lot of food is consumed and then vomiting is induced in order to get rid of it (bulimia);
- formation of scar tissue inside the organ;
- hypothyroidism.
Pathogenesis
Gastric emptying is a combination of parallel actions of the fundus tone, phase contractions of the antral part of the organ, and simultaneous inhibition of duodenal and pyloric contractions. Their interaction is carried out by the nervous system and specialized cells. The pathogenesis of gastroparesis consists in the disruption of the links in this chain. The stomach muscles become paralyzed and cannot cope with the task of mixing food with gastric juice, pancreatic enzymes, and transporting it to the next sections of the digestive system. This leads to poor absorption of nutrients and stagnation inside the organ.
Symptoms gastroparesis
Gastric paresis is manifested by the following symptoms:
- flatulence;
- nausea and vomiting;
- decreased appetite and weight loss;
- belching;
- heartburn;
- frequent hiccups;
- blood sugar instability.
The first signs are vague painful sensations in the stomach during or after eating. Immediately after the first sips, a feeling of fullness in the stomach occurs.
Stages
Depending on the severity of the manifestations of the disease, gastroparesis is divided into 3 stages. At the initial stage of the disease, episodic manifestations of pathology occur in the form of rapid saturation, short-term pain, nausea. Symptoms are quite easy to eliminate. At the second stage, they are more pronounced, partially controlled with medications, lifestyle and diet. At this time, paralysis of the stomach muscles is formed, peristalsis gradually slows down. At the later third stage, gastroparesis becomes chronic with constant symptoms of flatulence, nausea, vomiting, weight loss. Stagnation of food forms in the organ, putrefactive processes develop.
 [ 23 ]
[ 23 ]
Forms
Among the existing types of gastroparesis, there are 3 main etiological ones:
- diabetic — provoked by diabetes mellitus (about 30% of all cases). Develops over a fairly long period of time against the background of progressive diabetes. Accompanied by constant sour belching, heaviness in the epigastric region, unstable blood sugar levels. Moreover, during the course of the disease, the boundary between cause and effect is blurred, one aggravates the other;
- idiopathic - occurring without apparent cause, its origin is unknown (36%);
- postoperative gastric paresis - occurs after operations on abdominal organs (13%). As a rule, intestinal paresis is also connected to it. These are the most common postoperative complications. The explanation is that the walls of the stomach and intestines have many receptors and during operations, due to their injury, the tone of the sympathetic nervous system increases, and catecholamines are released into the blood. Paresis of the abdominal organs is considered a protective reaction of the body to injuries and surgical interventions.
 [ 24 ]
[ 24 ]
Complications and consequences
The consequences and complications of gastroparesis are manifested in chronic inflammatory processes, stenosis. The most dangerous consequence for diabetics is hypoglycemia, which threatens human health with coma and even death. This happens because not all the food consumed is processed in the stomach, and insulin is calculated taking into account its entire volume.
Diagnostics gastroparesis
Diagnosis of gastroparesis is based on the medical history, examination results, tests, in particular blood sugar test. But the most informative when gastroparesis is suspected is instrumental diagnostics.
Instrumental diagnostics consists of the following studies:
- Ultrasound of the stomach - allows you to examine the contours of the stomach on the screen;
- X-ray - using a contrast agent, shows the condition of the esophagus, stomach and duodenum;
- gastric manometry - measures pressure in different parts of the gastrointestinal tract;
- gastric endoscopy is an optical method for determining the condition of the organ from the inside;
- electrogastroenterography - determines the motor-evacuation function of the stomach by recording the biopotentials of different sections;
- gastric emptying breath test.
Differential diagnosis
Differential diagnostics excludes gastrointestinal obstruction - obstruction caused by various internal or external tumors, strictures; peptic ulcer; stenosis of the antrum of the stomach, duodenum, pylorus.
Who to contact?
Treatment gastroparesis
Treatment for gastroparesis depends on the patient's condition and ranges from a special diet and eating regimen to surgical treatment.
The diet should include a minimum of fats and fiber, portions are not abundant, but meals are frequent. Substances necessary for the body, but difficult to digest in crushed, liquid form. Medicines that increase the contractile activity of the stomach are also used. For diabetics, it is important to maintain sugar levels at the desired level. In special cases, parenteral or intravenous nutrition is used, but this is a temporary measure.
Medicines
Medicines used for gastric paresis include:
Cerucal - tablets, injection solution. It has anti-nausea and antiemetic effect, normalizes the tone of the gastrointestinal tract muscles. Tablets are taken half an hour before meals. The dose for children over 3 years old is determined at the rate of 0.1 mg per kilogram of body weight, older than this age - 10 ml four times a day. Solutions are administered as short-term infusions or long-term intravenously. Alkaline solutions are not used to prepare the injection. The drug is contraindicated for pregnant women, during lactation, children under 3 years of age. It is not prescribed for intestinal obstruction, bronchial asthma, gastrointestinal bleeding, hypersensitivity to sulfites. Cerucal can cause side effects: headache, tachycardia, stool disorders, tinnitus.
Domperidone is available in tablets, granules, suspensions, solutions, and suppositories. Eliminates nausea, hiccups, and regulates gastric motility. The dose for children weighing 20-30 kg is half a tablet twice a day, and for those weighing more, one tablet. Suspension and 1% solution are a more convenient form of the drug for small children. The dose for suspension is 2.5 ml per 10 kg of the child's weight; solution: 1 drop per kilogram three times a day. Adults are prescribed 10 mg (1 piece) 3-4 times; in case of severe vomiting, the dose may be increased to 20 mg with the same frequency. The drug may cause an allergic reaction, dry mouth, and diarrhea. It is contraindicated in patients with gastric perforation, intestinal obstruction, allergies to components, pregnant women, nursing mothers, and children weighing under 20 kg.
Erythromycin - tablets, antibiotic, accelerates the evacuation of food from the stomach. For children under 14 years old, the daily dose is 20-40 mg / kg, divided into 4 doses. After this age, 0.25 mg is taken every 4-6 hours 1-1.5 hours before meals. Do not prescribe for hypersensitivity to the drug, severe liver dysfunction. Side effects are rare, such as nausea, vomiting, diarrhea.
Metoclopramide - is produced in tablets and ampoules, accelerates digestion of food, eliminates nausea, hiccups, and vomiting. The dose for adults is a tablet before meals three times a day, in severe cases one ampoule is administered intramuscularly or intravenously. Children from 6 years of age are prescribed half a tablet or a tablet. The drug can cause drowsiness, rarely tremors and impaired coordination of movement. Not recommended for driving.
Vitamins
To maintain the muscle tone of the stomach, vitamins of group B are necessary. The diet must include nuts, cereals, grains, cabbage, beans (B1), wheat bread, tomatoes, meat, milk (B2), asparagus, green peas, kidneys, liver, garlic (B3), poultry, meat, peppers, potatoes (B6), lettuce, beets, bananas, avocado (B9), soy, seaweed, heart (B12). Carotenes and vitamin A promote the production of glycoproteins that protect the gastric mucosa from the aggressive effects of hydrochloric acid. They are found in foods such as liver, eggs, butter, fish, fish oil.
Physiotherapy treatment
Physical exercises have been developed during and after meals to help remove food from the stomach. These include bending back and forth, alternately drawing in and inflating the stomach. Walking and jogging speed up the digestion process. Physiotherapeutic treatment also includes electrical stimulation, which affects the muscles and nerves of the organ using pulsed currents. This procedure enhances blood circulation, metabolism, and the contractile function of the stomach muscles.
Folk remedies
For the treatment of gastroparesis, folk recipes are used that help in the absorption of food, improve digestion. Simple water with lemon juice, drunk before meals, promotes its absorption. It is recommended to precede meals with a decoction of corn silk. Bee capping also stimulates the motility of the gastrointestinal tract. Bees seal honeycombs with it. It is a mixture of bee saliva, wax, bee bread, pollen, propolis. To obtain a therapeutic effect, it is enough to simply chew it.
Herbal treatment will help reduce the feeling of heaviness in the stomach (coriander, dill, chamomile), flatulence (fennel, caraway, anise), improve digestion (dandelion, buckthorn, artichoke leaves, oregano, centaury). You should not resort to sedatives: valerian, mint, motherwort.
Homeopathy
Medicines that normalize the tone of the stomach and eliminate the symptoms associated with it include:
Iberogast is a multicomponent herbal preparation in the form of drops. The recommended dose is 20 drops in a small amount of water before or after meals three times a day. The course of treatment is a month. It is not prescribed to children under 18 years of age, since clinical studies have not been conducted on children, pregnant women, during lactation, with a diagnosis of calculous cholecystitis. Side effects include allergies, shortness of breath, nausea. In this case, treatment should be discontinued.
Gepazin is an oral drop, a supportive drug for patients with diabetes, reducing nausea, stomach fullness, flatulence, and belching. It is used for children over 11 years old in a dose of 15 drops, dripped into a small amount of water 3 times a day, for adults - 30 drops. Duration of treatment is 2 weeks. Contraindicated in case of hypersensitivity to the components.
Sodium phosphoricum salt Dr. Schuessler No. 9 - tablets, promotes digestion of fatty foods, reduces flatulence. For all ages, the dose used is 1 tablet, but with different frequency of administration: children under 5 years old once a day, 6-11 years old - 2 times, over 12 years old - 3 times (chronic condition). In acute manifestations, the frequency increases. Side effects are associated with the presence of wheat starch and occur in people with an allergy to cereals.
Amarin - drops for oral administration, used for disorders of stomach contractility. Acceptable for use from 11 years. Recommended 10 drops three times a day for children, the maximum dose can be increased to 30 drops if necessary. Adults dose is 10-20 drops, maximum 60. Contraindicated for children under 11 years, people with high stomach acidity, hypertension, gastrointestinal ulcer.
Surgical treatment
Surgical treatment is used in cases of severe conditions of patients and consists of widening the passage between the stomach and the duodenum. This method promotes faster emptying of the stomach and improvement of the general condition. Another method is the placement of a food tube in the small intestine. Nutrients are supplied through the abdomen, bypassing the stomach. It is also possible to implant an electrostimulator of the stomach, electrodes are connected to the organ, stimulating contractions.
Prevention
Preventive measures include monitoring sugar levels in patients with diabetes and mandatory familiarization with the instructions for the medication being taken, since painkillers, calcium channel blockers, and certain antidepressants provoke the development of gastroparesis. The main preventive measures should be aimed at preventing the occurrence of the cause that led to the weakening of gastric motility.
Forecast
If the cause that led to the disease is reversible, then the prognosis is favorable. Diabetic gastroparesis is also reversible if sugar is maintained at a normal level and the functions of the vagus nerve are restored. In other cases, the pathology is not cured, but only worsens over time.

