Medical expert of the article
New publications
Intestinal obstruction
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Intestinal obstruction is a severe pathology consisting of a complete disruption of the passage of contents through the intestine. Symptoms of intestinal obstruction include spastic pain, vomiting, bloating and delayed gas passage. The diagnosis is clinical, confirmed by radiography of the abdominal organs. Treatment of intestinal obstruction consists of intensive infusion therapy, nasogastric aspiration and, in most cases of complete obstruction, surgical intervention.
Causes intestinal obstruction
| Localization | Reasons |
| Colon | Tumors (usually in the splenic flexure or sigmoid colon), diverticulosis (usually in the sigmoid colon), volvulus of the sigmoid or cecum, coprostasis, Hirschsprung's disease |
| Duodenum | |
| Adults | Cancer of the duodenum or head of the pancreas |
| Newborns | Atresia, volvulus, bands, annular pancreas |
| Jejunum and ileum | |
| Adults | Hernias, adhesions (common), tumors, foreign body, Meckel's diverticulum, Crohn's disease (rare), roundworm infestation, intestinal volvulus, intussusception due to tumor (rare) |
| Newborns | Meconium ileus, volvulus or malrotation of the intestine, atresia, intussusception |
Pathogenesis
In general, the main causes of mechanical obstruction are abdominal adhesions, hernias, and tumors. Other causes include diverticulitis, foreign bodies (including gallstones), volvulus (turning of the intestine around the mesentery), intussusception (insertion of one intestine into another), and coprostasis. Certain areas of the intestine are affected differentially.
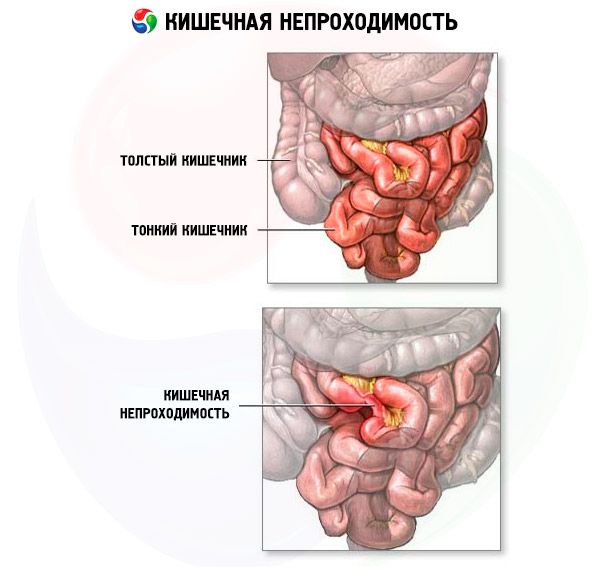
According to the mechanism of occurrence, intestinal obstruction is divided into two types: dynamic (spastic and paralytic) and mechanical (obstructive - when the lumen of the intestine is blocked by a tumor, fecal or gallstones, and strangulation, compression of the vessels, nerves of the intestinal mesentery due to strangulation, volvulus, nodulation). With adhesive disease and intussusception, intestinal obstruction of a mixed type occurs, since both obstruction and strangulation occur. By degree - complete and partial.
In simple mechanical obstruction, obstruction occurs without a vascular component. Liquid and food entering the intestine, digestive secretions and gas accumulate above the obstruction. The proximal segment of the intestine expands, and the distal segment collapses. The secretory and absorptive functions of the mucous membrane decrease, and the intestinal wall becomes edematous and congested. Significant distension of the intestine constantly progresses, increasing peristalsis and secretion disorders and increasing the risk of dehydration and the development of strangulation obstruction.
Strangulating ileus is an obstruction with compromised blood flow; it occurs in up to 25% of patients with small bowel obstruction. It is usually associated with hernia, volvulus, and intussusception. Strangulating ileus may progress to infarction and gangrene in less than 6 hours. Venous blood flow is compromised initially, followed by arterial blood flow, leading to rapid ischemia of the bowel wall. The ischemic bowel becomes edematous and imbibed with blood, leading to gangrene and perforation. Strangulation is rare in large bowel obstruction (except in volvulus).
Perforation may occur in an ischemic area of the intestine (typical for the small intestine) or with significant dilation. The risk of perforation is very high if the cecum is dilated in diameter >13 cm. Perforation of a tumor or diverticulum may occur at the site of obstruction.
Symptoms intestinal obstruction
The symptoms are polymorphic, they depend on the type and height of the intestinal lesion (the higher, the brighter the picture and the faster the change of stages), the stage of the disease.
The main symptom is pain: contractions, quite sharp, constantly increasing, initially in the area of intestinal obstruction, but may not have a constant localization, then throughout the entire abdomen, becomes constant and dull, and practically disappears in the terminal phase.
Flatulence (bloating) is more pronounced in the obstructive form, although it occurs in all types, it determines the asymmetry of the abdomen during examination: in the dynamic form of the large intestine - bloating is uniform throughout the abdomen, small intestine - more often in one area of the abdomen (in the high - in the upper floor, in the case of volvulus - in the middle part, in intussusception - in the right half). Retention of stool and gases at the onset of the disease may not manifest itself, especially with high intestinal obstruction, since stool and gases leave the distal parts of the intestine, sometimes even on their own or when performing enemas. On the contrary, vomiting is more characteristic of high intestinal obstruction, it appears faster and is more intense. Vomiting initially contains gastric contents mixed with bile, then contents appear, and finally, the vomit acquires a fecal odor. The appearance of continuous vomiting that does not bring relief is more characteristic of the obstructive and adhesive forms.
Peristalsis depends on the form and stage. In obstructive and mixed forms, hyperperistalsis is initially observed, sometimes audible at a distance and visible to the eye, accompanied by increased pain. When the process is localized in the small intestine, it occurs early, simultaneously with pain, frequent, short, in the large intestine - peristalsis becomes stronger later, sometimes on the second day, attacks are rare, long or have a wave-like character. Peristalsis is especially clearly determined by auscultation of the abdomen. Gradually, peristalsis subsides and with the onset of intoxication it comes to naught and is not determined even by auscultation. A sign of the transition from the neuroreflex stage to intoxication is the appearance of dry tongue, sometimes with a "varnished" bright red tint due to dehydration and chloropenia.
Symptoms of intestinal obstruction appear soon after the onset of the disease: spasmodic pain in the umbilical or epigastric region, vomiting, and, in the case of complete obstruction, bloating. Patients with partial obstruction may experience diarrhea. Severe, constant pain suggests the development of strangulation syndrome. In the absence of strangulation, pain syndrome is not expressed during palpation. Hyperactive, high-frequency peristalsis is characteristic with periods coinciding with spasmodic attacks. Sometimes dilated intestinal loops are palpated. With the development of infarction, the abdomen becomes painful and peristaltic sounds are not heard during auscultation or are sharply weakened. The development of shock and oliguria is an unfavorable symptom indicating advanced obstructive obstruction or strangulation.
Signs of intestinal obstruction of the colon are less pronounced and develop gradually compared to small intestinal obstruction. Gradual delay in stool is characteristic, leading to its complete delay and abdominal distension. Vomiting may occur, but it is not typical (usually several hours after the onset of other symptoms). Spasmodic pain in the lower abdomen is reflex and is caused by the accumulation of feces. Physical examination reveals a characteristically distended abdomen with a loud rumbling. There is no pain on palpation, and the rectum is usually empty. A volumetric formation in the abdomen can be palpated, corresponding to the zone of obstruction by the tumor. General symptoms are moderate, and the deficit of fluid and electrolytes is insignificant.
Volvulus often has a sudden onset. The pain is continuous, sometimes colicky and wave-like.
Where does it hurt?
Stages
In dynamics, three stages are distinguished: neuro-reflexive, manifested by the syndrome of "acute abdomen"; intoxication, accompanied by a violation of water-electrolyte, acid-base states, chloropenia, microcirculation disorder due to thickening of the blood to a greater extent in the portal blood flow system; peritonitis.
Forms
Obstructive intestinal obstruction is divided into small bowel obstruction (including the duodenum) and large bowel obstruction. Obstruction can be partial or complete. Approximately 85% of cases of partial small bowel obstruction resolve with conservative measures, while approximately 85% of cases of complete small bowel obstruction require surgery.
According to the clinical course, acute, subacute and chronic forms are distinguished.
Diagnostics intestinal obstruction
Mandatory radiography with the patient in the supine and upright positions usually allows the diagnosis of obstruction. However, only laparotomy can definitively diagnose strangulation; a complete serial clinical and laboratory examination (e.g., complete blood count and biochemistry, including lactate levels) ensures timely diagnosis.
Specific symptoms play a major role in diagnosis.
- Matieu-Sklyarov's symptom - upon palpation, with a slight shaking of the abdominal wall, a noise is detected, a splash of fluid accumulated in a stretched intestinal loop - characteristic of obstructive intestinal obstruction.
- The Shiman-Dans symptom is characteristic of ileocecal intussusception: upon palpation, the right iliac fossa becomes empty.
- Chugaev's symptom - when lying on the back with the legs pulled up to the stomach, a deep transverse stripe appears on the stomach - characteristic of the strangulation form.
- Schlange's symptom - upon palpation of the abdomen, a sharp increase in peristalsis is noted in the initial stage of obstructive and mixed forms.
- During auscultation of the abdomen with simultaneous percussion, the following symptoms can be identified: Kivul's (metallic sound), Spasokukotsky's (the sound of a falling drop), Wils's (the sound of a bursting bubble).
When examining the rectum, which is mandatory in all cases of abdominal pathology, it is possible to detect a tumor, the presence of fluid in the pelvis, the Obukhov Hospital symptom (the rectal ampulla is dilated, the anus is gaping - typical for the obstructive or strangulation form), the Gold symptom (palpation of a distended loop of the small intestine). When performing enemas, it is possible to detect the Zege-Manteuffel symptom - with intestinal obstruction of the sigmoid colon, it is not possible to introduce more than 500 ml of water into the rectum; the Babuk symptom is typical of intussusception - with the primary enema there is no blood in the rinsing water, after a five-minute palpation of the abdomen with a repeated siphon enema, the rinsing water has the appearance of "meat slops".
If intestinal obstruction is suspected, the condition of all hernial orifices is necessarily checked to exclude strangulation. The second obligatory examination, even before enemas, is a general radiography of the abdominal cavity. Pathognomonic for intestinal obstruction are: Kloiber's cups, arches, transverse striation of the small intestine distended with gases (it is better revealed in the supine position in the form of Casey's symptom - a type of circular ribbing resembling a "herring skeleton"). In unclear cases, a contrast X-ray examination of the intestine is carried out (the patient is given 100 ml of barium suspension) with repeated studies of the passage of contrast every 2 hours. Signs are: a delay in the contrast in the stomach or small intestine for more than 4 hours. In case of incomplete intestinal obstruction, the passage of contrast is monitored until it is removed to the depot above the site of obstruction - this sometimes takes up to two days. In case of intestinal obstruction of the large intestine, it is advisable to perform a colonoscopy. If dynamic intestinal obstruction has occurred, it is necessary to identify the cause that caused the spasm or paresis: appendicitis, pancreatitis, mesenteritis, thrombosis or embolism of the mesenteric vessels and other acute abdominal pathology.
On plain radiography, a series of distended small bowel loops resembling a ladder is characteristic of small bowel obstruction, but this pattern may also be seen with right colonic obstruction. Horizontal fluid levels in the bowel loops may be seen with the patient in an upright position. Similar but less pronounced radiographic findings may be seen in paralytic ileus ( intestinal paresis without obstruction); differential diagnosis of intestinal obstruction may be difficult. Distended bowel loops and fluid levels may be absent in high jejunal obstruction or in closed strangulation obstruction (as may occur with volvulus). Infarcted bowel may produce a space-occupying lesion on radiography. Gas in the bowel wall (pneumatosis of the intestinal wall) indicates gangrene.
In colonic bowel obstruction, abdominal radiography shows dilation of the colon proximal to the obstruction. In cecal volvulus, a large gas bubble may be seen occupying the mid-abdomen or left upper quadrant. In cecal and sigmoid volvulus, a radiocontrast enema may visualize the distorted obstruction as a "bird's beak" twist; this procedure can sometimes actually resolve the sigmoid volvulus. If a contrast enema is not feasible, colonoscopy may be used to decompress the sigmoid volvulus, but this procedure is rarely effective in cecal volvulus.
What do need to examine?
How to examine?
Who to contact?
Treatment intestinal obstruction
Patients with suspected intestinal obstruction should be hospitalized. Treatment of intestinal obstruction should be carried out simultaneously with diagnostics. A surgeon should always be involved in this process.
Metabolic therapy is mandatory and is similar for both small- and large-bowel obstruction: nasogastric aspiration, intravenous fluids (0.9% saline or lactated Ringer's solution to restore intravascular volume), and bladder catheterization to monitor urine output. Electrolyte resuscitation should be guided by laboratory tests, although serum Na and K are likely to be low in cases of repeated vomiting. If bowel ischemia or infarction is suspected, antibiotics should be given (eg, a third-generation cephalosporin such as cefotetan 2 g IV).
Specific events
In case of duodenal obstruction in adults, resection is performed or, if the affected area cannot be removed, palliative gastrojejunostomy is performed.
In complete small bowel obstruction, early laparotomy is preferred, although in cases of dehydration and oliguria, the operation may be delayed for 2 or 3 hours to correct the fluid-electrolyte balance and diuresis. Areas of specific bowel lesion should be removed.
If the cause of the obstruction was a gallstone, cholecystectomy may be performed simultaneously or later. Surgical measures to prevent recurrence of obstruction should be performed, including hernia repair, removal of foreign bodies, and removal of adhesions. In some patients with signs of early postoperative obstruction or recurrence of obstruction due to adhesions, in the absence of abdominal symptoms, simple intubation of the intestine with a long intestinal tube (many consider nasogastric intubation to be the standard as the most effective) may be performed instead of surgery.
Disseminated abdominal cancer occluding the small bowel is the leading cause of death in adult patients with gastrointestinal malignancies. Bypass anastomoses, surgical or endoscopic stenting may provide short-term improvement.
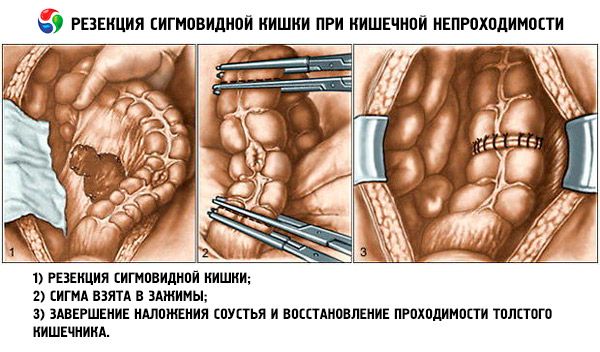
Obstructing colon cancers are most often treated with immediate resection and primary anastomosis. Other options include unloading ileostomy and distal anastomosis. Occasionally, unloading colostomy with delayed resection is necessary.
If the obstruction is due to diverticulosis, perforation often occurs. Removal of the affected area may be quite difficult, but it is indicated in cases of perforation and general peritonitis. Bowel resection and colostomy without anastomosis are performed.
Coprostasis usually occurs in the rectum and can be resolved by digital examination and enemas. However, the formation of single- or multi-component fecal stones (i.e., with barium or antacids) causing complete obstruction (usually in the sigmoid colon) requires laparotomy.
Treatment of cecal volvulus consists of resection of the involved portion and anastomosis or fixation of the cecum in its normal position with cecostomy in debilitated patients. In sigmoid volvulus, an endoscope or long rectal tube can often decompress the loop and resection and anastomosis can be delayed over several days. Without resection, intestinal obstruction almost inevitably recurs.
Drugs


 [
[