Medical expert of the article
New publications
Bleeding from gastric ulcer and 12-rectal ulcer
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Peptic ulcer disease is complicated by bleeding in approximately every tenth patient. According to research data, overt bleeding occurs in 10-15% of patients with peptic ulcer disease, and hidden bleeding, detected only by the Gregersen reaction and not clinically manifested, accompanies an exacerbation of the disease. Duodenal ulcers bleed 4-5 times more often than gastric ulcers. Bleeding is often the first sign of the disease.
The mechanism of bleeding development is that a vessel is damaged in the ulcer area and begins to bleed. If a small vessel is damaged, the bleeding is very minor, without clinical manifestations and is detected only by the Gregersen reaction.
Overt bleeding from an ulcer is characterized by three main syndromes:
- bloody vomiting;
- tarry stools;
- symptoms of acute blood loss.
Bloody vomiting is most typical for bleeding from a stomach ulcer and is much less common with a duodenal ulcer. In the latter case, bloody vomiting is observed because the contents of the duodenum with blood are thrown into the stomach. The gastric contents in bloody vomiting usually look like coffee grounds (dark brown), which is due to the conversion of hemoglobin in the spilled blood under the influence of hydrochloric acid into hydrochloric acid hematin, which has a dark color. Bloody vomiting occurs soon after bleeding, and sometimes some time after it. If the bleeding develops very quickly and the amount of spilled blood is large, vomiting of scarlet blood is possible.
Tarry stool, melena (melena) is the most important sign of bleeding from a duodenal ulcer, usually observed after the loss of more than 80-200 ml of blood.
Melena is characterized by a liquid or mushy consistency of feces and their black color. Under the influence of intestinal flora, black iron sulfide is formed from hemoglobin in the spilled blood. Typical stool with melena is black, like tar, unformed (liquid, mushy), shiny, sticky. It is necessary to distinguish melena from pseudomelena, i.e. black formed stool associated with the intake of blueberries, bismuth, bird cherry, blackberries, iron preparations. Unlike true melena, pseudomelena has a normal consistency and shape.
Melena can also be observed with massive bleeding from a stomach ulcer. In this case, blood not only erupts from the stomach in the form of "coffee grounds", but can also enter the duodenum.
It should be noted that with intense bleeding, the stool may not be tarry and may become scarlet in color.
It should be emphasized that when bleeding from a duodenal ulcer, black tarry stool appears not at the time of bleeding, but several hours or even a day after it. Melena is usually observed after a single blood loss for another 3-5 days.
A characteristic sign of ulcerative bleeding is the sudden disappearance of pain syndrome - Bergman's symptom.
General symptoms of acute blood loss
The severity of general symptoms of acute blood loss depends on its size and speed. The faster the bleeding and the more massive the blood loss, the more pronounced the general disorders.
The circulating blood volume (CBV) is 2.4 l/m2 of body surface area in women and 2.8 l/m2 of body surface area in men, or 70 ml/kg of body weight in men and 65 ml/kg in women. The average CBV of an adult weighing 70 kg is 5 l, of which 2 l is cellular elements (erythrocytes, leukocytes, platelets), and 3 l is plasma.
A blood loss of about 10% of the BCC (400-500 ml) either does not cause general symptoms (i.e. shock, a drop in blood pressure, disturbances of consciousness and other symptoms), or general disturbances will be weakly expressed (mild nausea, chills, dryness and a salty taste in the mouth, general weakness, a slight tendency to decrease blood pressure).
Blood loss of about 10-15% of the BCC is well and quickly compensated by the body by releasing deposited blood into the bloodstream.
Blood loss of about 15-25% of the BCC (700-1300 ml) causes the development of stage I hemorrhagic shock (compensated, reversible shock). This stage of shock is well compensated by activation of the sympathoadrenal system, high release of catecholamines, and peripheral vasoconstriction. The following symptoms appear in this phase:
- the patient is conscious, calm, or sometimes somewhat excited (agitated);
- the skin is pale, the hands and feet are cold;
- subcutaneous veins on the arms in a collapsed state;
- pulse accelerated to 90-100 per 1 min, weak filling;
- Blood pressure remains normal or tends to decrease;
- oliguria is observed, the amount of urine excreted is reduced by half (with the norm being 1-1.2 ml/min or 60-70 ml/h).
Blood loss is about 25-45% of the BCC (1300-1800 ml). With such a blood loss, decompensated reversible hemorrhagic shock develops. In this case, the activation of the sympathoadrenal system and high peripheral resistance cannot compensate for the sharply reduced cardiac output due to blood loss, which leads to a decrease in systemic blood pressure and the development of the following symptoms:
- the pallor of the skin is significantly expressed;
- cyanosis of visible mucous membranes (lips, nose);
- dyspnea;
- tachycardia, muffled heart sounds;
- pulse is very weak, pulse rate is up to 120-140 per 1 minute;
- Systolic blood pressure below 100 mm Hg, low pulse pressure;
- oliguria (diuresis less than 20 ml/h);
- consciousness is preserved, but the patients are restless and agitated.
Dyspnea is caused by deterioration of cerebral blood flow, as well as the development of varying degrees of "shock lung" due to impaired permeability of the vessels of the pulmonary circulation and overfilling of the lungs with blood due to blood shunting. The symptoms of shock lung develop gradually, after 24-48 hours, and in addition to dyspnea, they are manifested by coughing, scattered dry wheezing in the lungs, and in severe cases (in the terminal phase) by a picture of pulmonary edema.
Blood loss of 50% of the BCC or more (2000-2500 ml) causes the development of severe hemorrhagic shock (some authors call it decompensated, irreversible). The latter term is somewhat arbitrary, since timely and correctly performed therapy even at this stage can lead to an improvement in the patient's condition.
Main clinical symptoms:
- the patient is unconscious;
- the skin is very pale, covered with cold, sticky sweat;
- dyspnea;
- the pulse is threadlike, its frequency is more than 140 per 1 minute;
- systolic blood pressure is sometimes not determined;
- oliguria is characteristic.
Laboratory and instrumental data in acute bleeding from gastric ulcer or duodenal ulcer
- Complete blood count. Posthemorrhagic anemia develops. However, the degree of anemia is not an indicator of the amount of blood lost, since acute blood loss reduces the volume of the vascular bed. In the first hours of major blood loss, a moderate decrease in hemoglobin and the number of erythrocytes may be observed. 1-2 days after the bleeding has stopped, normochromic or hypochromic anemia develops (due to hemodilution - the transition of fluid from the interstitial spaces into the vascular bed in order to increase the volume of the BCC). A decrease in the number of leukocytes and platelets is also possible.
- ECG. Sinus tachycardia is noted, sometimes various types of extrasystoles. Diffuse changes in the myocardium are characteristic in the form of a decrease in the ST interval downwards from the isoline and a significant decrease in the amplitude of the T wave in the chest and standard leads. In elderly people, a negative symmetrical T wave may appear as a manifestation of ischemic changes in the myocardium.
- Chest X-ray in severe hemorrhagic shock reveals a picture of pulmonary edema (decreased transparency of lung tissue, the appearance of foci of infiltration, and root darkening in the form of a “butterfly”).
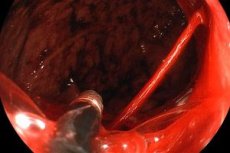
- Fibrogastroduodenoscopy. If ulcer bleeding is suspected, and especially if ulcer bleeding is present, urgent FGDS should be performed for diagnostic and therapeutic purposes. If a bleeding vessel is detected during FGDS, it should, if possible, be coagulated using diathermo- and laser coagulation in order to stop the bleeding.
Determining the degree of blood loss
Various methods have been proposed to determine the degree of blood loss. Most of them assess the degree of blood loss in relation to the BCC.
Calculation of the Algover shock index
The Algover shock index is the ratio of the pulse rate to the systolic blood pressure level.
Determination of the degree of blood loss using the Algover shock index
Shock index indicators |
Volume of blood loss |
0.8 and less |
10% BCC |
0.9-1.2 |
20% BCC |
1.3-1.4 |
30% BCC |
1.5 and more |
40% BCC |
About 0.6-0.5 |
Normal BCC |
Determination of the degree of blood loss according to Bryusov P.G. (1986)
The method is based on the definition of the following indicators:
- general condition of the patient;
- blood pressure value;
- pulse rate;
- hemoglobin and hematocrit values.
There are four degrees of bleeding severity.
Mild bleeding:
- the deficit of the BCC does not exceed 20%;
- the patient's condition is satisfactory;
- weakness and dizziness may occur;
- pulse rate up to 90 per 1 minute;
- Blood pressure is normal or there is a tendency for it to decrease slightly;
- hemoglobin content above 100 g/l;
- hematocrit greater than 0.30.
Moderate severity of blood loss:
- BCC deficit within 20-30%;
- the patient's condition is moderate;
- marked general weakness, dizziness, and darkening before the eyes are noted;
- pulse rate up to 100 per 1 minute;
- moderate arterial hypotension;
- hemoglobin content 100-70 g/l;
- hematocrit 0.30-0.35.
Severe bleeding:
- BCC deficit 30-40%;
- the patient's condition is serious;
- severe weakness, severe dizziness, shortness of breath, possible pain in the heart area (mainly in the elderly and patients with coronary heart disease);
- pulse rate 100-150 per 1 minute;
- Systolic blood pressure decreases to 60 mm Hg;
- hemoglobin content 70-50 g/l;
- hematocrit less than 0.25.
Extremely severe bleeding:
- BCC deficit over 40%;
- the patient's condition is extremely serious;
- the patient is unconscious, covered in cold sweat, the skin is pale, the mucous membranes are cyanotic, there is shortness of breath;
- pulse and blood pressure are not determined;
- hemoglobin below 50 g/l;
- hematocrit less than 0.25-0.20.
 [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
[ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ]
Determination of the degree of blood loss according to G.A. Barashkov (1956)
The method of G. A. Barashkov is based on the determination of the relative density of blood using a series of copper sulfate solutions with a relative density from 1.034 kg/l to 1.075 kg/l.
A drop of venous heparinized blood is dropped into vials with copper sulfate solutions. If the blood density is lower than the density of the solution, the drop immediately floats, if higher, it sinks. If the drop of blood remains suspended for 3-4 seconds, this indicates that their density corresponds.
Bleeding from gastric ulcers and duodenal ulcers must be differentiated from bleeding from the esophagus, stomach and intestines of other etiologies.

