Medical expert of the article
New publications
Gastric bypass surgery: reviews and results
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
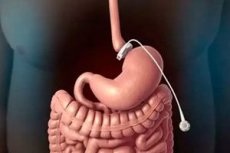
In some cases, bariatric surgery is used to treat obesity, a chronic endocrine-metabolic disorder of the body, and one of the most common types of surgery is gastric bypass. During this operation, surgeons reduce the volume of the stomach and reconstruct part of the small intestine adjacent to it.
Indications for the procedure
Bariatric gastric bypass or bariatric gastroenterostomy can be used for morbid obesity that does not respond to conservative treatment (with a low-calorie diet and energy-burning physical exercise), and the desire to “reduce” the stomach to lose weight is not enough.
Indications for gastric bypass include diagnosed grade 3 obesity (or morbid obesity) - when the BMI (body mass index) is equal to or exceeds 40 (recall that the normal BMI is 18.5-25). That is, body weight, according to Western experts, should be 45-50 kg higher than normal (in domestic bariatric surgery, this figure is higher and averages about 80 kg).
The operation may be prescribed for the specified degree of obesity if the patient seriously suffers from concomitant diseases, in particular, if there is a history of severe arterial hypertension, type II diabetes mellitus, degenerative joint pathologies (osteoarthritis) or arthritis, cardiovascular diseases, chronic pulmonary hypoventilation syndrome or sleep apnea.
Also, candidates for this surgery should have a history of unsuccessful attempts to lose excess weight through controlled dietary changes.
Where can I have gastric bypass? This operation is performed in gastroenterological clinics, where there are specialists who know how to perform gastroenterostomy, or in specialized departments of endoscopic (laparoscopic) abdominal surgery. However, free gastric bypass – as a bariatric operation – is not provided.
Preparation
Preparation for gastric bypass surgery involves the same comprehensive preoperative evaluation that is given to patients before abdominal surgery. The medical history and physical examination are designed to identify concomitant diseases that may cause complications.
Usually, a clinical and biochemical blood test is required (for coagulation levels, lipid content, thyroid hormones, ferritin).
An ECG, chest X-ray, ultrasound of the stomach and intestines or gastroendoscopy (to determine possible gastric pathology) are performed. The gallbladder, spleen and liver are also examined using ultrasound sonography.
In addition, preparation includes a preoperative liquid diet (for one to two weeks before surgery) - to reduce the amount of fat in the liver and spleen. The diet includes pureed soups and vegetable purees; protein shakes; rice broth; drinks without sugar, caffeine and carbon dioxide; vegetable juices. Moreover, drinks should be consumed half an hour after eating.
Also, one week before the operation, you should stop taking certain medications, including anticoagulants, steroids, NSAIDs, oral contraceptives, and vitamin E.
If the patient smokes, he or she should give up this habit several weeks before the operation, as smoking slows down recovery and increases the risk of complications.
 [ 11 ]
[ 11 ]
Technique gastric bypass
Today, the technique of gastric bypass involves dividing the stomach (by suturing with titanium staples) into two parts, with the upper part having a volume of no more than 30-50 ml. From the distal side of the smaller part (which will perform all the functions of the stomach), the axially dissected jejunum (the diverting part) is sutured, i.e. an anastomosis is formed. The remaining (larger in volume) part of the stomach is mechanically excluded from the digestive process.
Minimally invasive laparoscopic gastric bypass is performed without laparotomy – with limited access through 4-6 small incisions (ports): an endoscope connected to a video camera is inserted through one, and the others provide access for specialized surgical instruments. Surgical manipulations are visualized on the monitor.
By reducing the volume of the stomach, the main goal of bariatric gastroenterostomy is achieved - reducing the amount of food that can be consumed by the patient at one time, and therefore digested and absorbed (absorbed in the small intestine). Thus, the body will receive fewer calories from the food consumed.
In addition, the "change in route" of food in the gastrointestinal tract - its entry into the initial sections of the jejunum, bypassing the stomach cavity (that is, bypassing it, through an anastomosis) - leads to the appearance of a feeling of satiety and lack of appetite. Experts associate this with the fact that food entering directly into the proximal part of the jejunum reduces the production of ghrelin - a peptide hormone that regulates appetite.
Contraindications to the procedure
Since gastric bypass is a complex combined surgical procedure to create a gastrointestinal anastomosis, it is contraindicated in patients with a BMI below 35.
Also, contraindications to gastric bypass surgery concern patients over 60 years of age; existing inflammation of the esophageal mucosa (esophagitis). This operation is not performed in cases of mental disorders and in cases of alcohol or drug addiction of patients.
Gastric bypass is performed under general anesthesia, and the operation can last from two to four hours. Therefore, surgeons also take into account the presence of contraindications to general anesthesia: serious heart rhythm disturbances, post-infarction and post-stroke conditions, cerebral vascular pathologies, severe bronchial asthma, and some others.
Consequences after the procedure
This surgical intervention may be accompanied by both complications after the procedure and numerous long-term negative consequences of gastric bypass.
The main postoperative complications of gastric bypass, which occur in almost a quarter of cases, include early anastomotic leakage (in 2% of cases), intra-abdominal infection (about 3% of cases), gastrointestinal hemorrhage (1.9%), and pulmonary embolism (0.4%). Damage to the stomach, intestine, or other organs during surgery cannot be ruled out. Mortality during the first month after surgery is estimated to range from 2.5% to 5% of cases, and 0.5% during the six months after surgery.
Over time, the consequences of gastric bypass may manifest as a hernia (in 0.5% of those operated on), gallstones (in 6-15% of patients), gastric stenosis (4.7% of cases), intestinal obstruction due to adhesions (1.7%). Deficiency of vitamins B12 and D, folic acid, calcium and iron can lead to the development of secondary hyperparathyroidism, bone resorption and iron deficiency anemia. Cases of gastritis and gastric ulcers are also noted.
For this reason, it is recommended to visit your doctor quarterly during the first year after gastric bypass; twice a year during the second year, and then annually (with a comprehensive biochemical blood test).
Care after the procedure
Most patients stay in the clinic for three to four days after surgery, but doctors recommend sitting up in bed and walking a little on the first day.
Post-procedure care includes ensuring the sterility of the post-operative wound, the catheter (it is necessarily installed during laparotomy bypass), medicinal prevention of blood clots, pain relief, etc.
Medical staff monitors blood pressure, the state of gas exchange in the lungs and general metabolism after surgery (complete blood count, with prothrombin time and electrolyte levels, kidney and liver function).
To prevent deep vein thrombosis after bariatric surgery, their condition is assessed based on ultrasound or angiography. Patients are advised to use compression hosiery on their legs.
Immediately after the operation – the first two days – it is strictly forbidden to consume any food or drink.
Diet and Nutrition After Gastric Bypass
The diet after gastric bypass during the first week (excluding the first postoperative days) allows you to drink only clear liquids (no more than 30-45 mg per hour); this can be water (still), skim milk or broth, juice without sugar.
For the next two weeks, the patient eats only liquid food, consisting of protein shakes, low-fat soft cheese, cottage cheese or boiled white meat (65 g of protein per day) mashed with skim milk or broth. In addition, at least 1.5-1.6 liters of water per day should be drunk: in small portions, slowly, about half an hour before meals and every hour after meals.
It is essential to take daily multivitamins and iron supplements as prescribed by your doctor, as well as calcium citrate (0.4 g twice a day).
Diet and nutrition after gastric bypass at 4-5 weeks include gradual introduction of soft food - chopped boiled meat (lean chicken, turkey), fish (also boiled) and boiled vegetables. Recommendations regarding water consumption are the same. Vitamin D3 is added to the vitamins and minerals already taken (1000 IU per day).
In the sixth week, patients begin to eat solid food. But this does not mean that you can eat everything. The diet limits total daily consumption to 800-1200 kcal during the first year and to 1500 kcal after 1.5 years of gastric bypass. You should also avoid foods that are poorly digested (beef, pork, whole grains, mushrooms, grapes, corn, legumes), whole milk, canned food, fatty and spicy foods, sweets.
Bariatric experts warn: overeating after gastric bypass is out of the question. At the physiological level, overeating is prevented by the so-called dumping syndrome, which occurs as a result of too fast or excessive absorption of food (especially sweet and fatty). The stomach, reduced by surgery, simply “dumps” food into the small intestine, which causes vomiting, diarrhea, bloating, weakness, muscle cramps, hyperhidrosis, and rapid heartbeat (this usually lasts for one to two hours). So, patients after gastric bypass, who have tried a couple of times to return to the habit of “eating heavily,” simply stop “experimenting” with their stomach.
The portion size at each meal should not be larger than your fist.
Reviews and results
As noted by experts from the American Society for Metabolic and Bariatric Surgery (ASMBS), the prognostic results of bariatric gastric bypass surgery are getting rid of 50-60% of excess kilograms during the first 12 months after surgery: an average of 5-7 kg per month.
It is important to understand that over time, weight loss will decrease and in the long term, much of it will depend on lifestyle: healthy eating and physical activity.
Feedback from some patients indicates that gastric bypass surgery resulted in the greatest weight loss in the first 6-8 months after its implementation. Many emphasize the fact of lowering blood pressure, normalizing glucose levels, and lowering cholesterol levels in the blood.

