Medical expert of the article
New publications
An eyesore on a man's eye
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
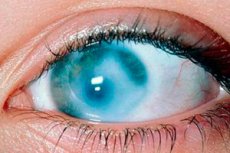
It is not difficult to guess why the name of a scar on the cornea – an eyesore – has become a figurative expression, because the phraseological unit “like an eyesore” is used when talking about something that is very annoying and disturbing.
The medical term for a dense white spot on the front transparent part of the eye is corneal leukoma. What does leukoma mean? In Greek, leukos means "white" and cornea is the Latin name for the cornea.
According to ICD-10, in the class of ophthalmological diseases, the code for this pathology is H17.0 (in the section - Scars and corneal opacities).
Epidemiology
The most common causes of corneal opacity were ocular trauma (50.6%), retinal disease (15.5%), measles (9.5%), and congenital etiology (5.5%).[ 1 ] The prevalence of corneal leukoma is about 0.03%.[ 2 ] The prevalence of visual impairment and blindness among patients with corneal opacity was 46.2% and 19.2%, respectively.[ 3 ]
Causes eyesore
Corneal leukoma often occurs in keratitis and corneal wounds due to multiple factors such as physical, chemical and congenital. Corneal opacity leads to cosmetic problems. If the scar is in the visual axis, it can lead to vision loss and even functional blindness.
Ophthalmologists have included the following in the list of the most common and possible causes of a cataract in the eye: [ 4 ]
- eye damage – mechanical injuries, thermal or chemical burns of the cornea;
- inflammation of the cornea - keratitis of any etiology, which, in turn, can lead to the formation of a corneal ulcer, healing with scarring of its underlying tissue (stroma);
- dry cornea (xerophthalmia);
- corneal injury due to abnormal eyelash growth (trichiasis);
- congenital blenorrhea (in infants) with gonorrhea or diffuse parenchymatous keratitis associated with congenital syphilis;
- intraepithelial neoplasia of the conjunctiva or cornea, retinoblastoma;
- genetically determined corneal dystrophy (degradation);
- hereditary metabolic disorders with corneal lesions;
- infectious diseases (measles). [ 5 ]
Risk factors
All of the above reasons also relate to risk factors for the formation of a cataract.
For example, severe penetrating eye injuries leading to corneal rupture require emergency surgery: the eye can be saved, but postoperative scarring leads to progressive corneal opacity, and after some time a white film forms on the eye.
By the way, it should be taken into account that visual impairment in advanced cases of beta-carotene (vitamin A) deficiency can manifest itself as clouding of the cornea. [ 6 ], [ 7 ]
Alteration of the cornea with its subsequent inflammation can be caused by lagophthalmos (incomplete closure of the eyelid) in patients with facial nerve paralysis, blepharism (increased blinking in nervous tics or Tourette syndrome) or, conversely, a decrease in the frequency of blinking, for example, in Parkinson's disease, glaucoma. [ 8 ]
It remains to add the increased risk of developing infectious inflammation of the cornea when wearing unsterilized contact lenses, the presence of a hereditary factor (if there have been cases of corneal leukoma in the family), [ 9 ] as well as age (as the body ages, morphological changes in the structure of the corneal stroma of a degenerative nature are possible).
Pathogenesis
The structure of the corneal stroma is formed by fibers of the fibrillar protein collagen and sulfated glycosaminoglycans, represented by keratan sulfate type I (the content of which is much higher compared to cartilage tissue) and keratan sulfate high-molecular proteins (proteoglycans) with a high content of leucine: keratocan, lumican, osteoglycin. Together, they make the cornea sufficiently strong, optimally elastic and absolutely transparent. In addition, the extracellular matrix of the cornea contains adhesive glycoproteins: several isoforms of laminin and fibronectin, which fasten all elements of the corneal layer of the eye.
The apical region of the stroma, Bowman's membrane, is a dense acellular layer between the stroma itself and the corneal epithelium, consisting mainly of tightly woven collagen fibrils. So, the pathogenesis of scar formation on the cornea is associated with damage to this membrane, since alterations that do not affect it do not leave scars during healing. [ 10 ]
Fibronectin, produced by corneal keratocytes, and keratoepithelin, synthesized by corneal epithelial cells and stromal fibroblasts, promote the adhesion of collagen microfibrils and sulfated glycosaminoglycans to accelerate the reparation of damaged corneal tissue. The formation of a corneal leukoma is the result of the accumulation of excess protein fibers throughout the middle and anterior stroma. [ 11 ]
In addition, an important role in the disruption of the remodeling processes of the damaged extracellular matrix of the cornea is played by the deficiency of limbal stem cells (LSC) produced by its epithelium, as well as deviations associated with the expression of extracellular enzymes - matrix metalloproteinases, which are designed to ensure the timely apoptosis of obsolete (damaged) keratocytes and the differentiation of cells of regenerated tissues.
Symptoms eyesore
The very first signs of the formation of a cataract are manifested by a sensation of a veil in front of the affected eye - if the scar tissue is concentrated closer to the center.
When leukoma begins to form on the periphery of the cornea, symptoms in the form of decreased vision will appear later - as the affected area increases.
Many patients complain of increased tear production, a feeling of clogged eyes, and light spots and lines appearing before their eyes.
Since scar tissue on the cornea has no capillaries, there can be no red cataract in the eye. But neovascularization of the cornea, that is, excessive growth of blood vessels from the limbal vascular plexus, can occur. And redness of the sclera occurs for a number of reasons, detailed in the material - Redness of the eyes.
Complications and consequences
If the cornea is damaged by infection or has been injured, the resulting opacity can distort or block light passing through the cornea, causing complications and consequences such as decreased visual acuity and deprivation amblyopia.
If the intraocular pressure is elevated, that is, there is a history of glaucoma, and the leukoma is not very thick, then it can protrude significantly relative to the corneal surface, and then a corneal staphyloma is formed.
Leukoma localized in the central part of the cornea can cause blindness.
Diagnostics eyesore
Slit lamp examination – corneal biomicroscopy – is a classic ophthalmological examination of the eye. [ 12 ]
In addition, instrumental diagnostics are performed using corneal keratometry and optical coherence tomography. Visual fields are determined using computer perimetry; intraocular pressure is also measured.
Differential diagnosis
Differential diagnostics aim to distinguish corneal leukoma from the whitish tint of the pupil associated with clouding of the lens in a disease such as cataract.
A cataract does not form on the white of the eye (on the sclera), but there may be a slightly raised yellowish formation on the white of the eye or conjunctiva (closer to the inner corners of the eyes), similar to a fatty tumor on the eye, or, as is often said, a growth on the human eye. This benign formation occurs in older people and is called a pinguecula; it does not affect vision and, as a rule, does not manifest itself in any way.
Treatment eyesore
What to do if a cataract appears on the eye? Go quickly to an ophthalmologist (eye doctor) who knows how to remove a cataract from the eye.
Only surgical treatment can completely remove corneal leukoma: corneal transplantation orkeratoprosthesis surgery using a synthetic corneal analogue (keratoprosthesis). [ 13 ]
Corneal transplants such as penetrating keratoplasty (PK) and lamellar keratoplasty (LK) are excellent treatments for cataracts in people who want to restore their visual acuity. However, after corneal transplantation, many people experience graft rejection and chronic endothelial cell loss.[ 14 ]
Kerato-pigmentation (KTP) has been used for centuries for cosmetic purposes when visual reconstruction is ineffective. [ 15 ] Galen (131-201 CE) used copper sulfate to stain corneal leukoma [ 16 ], [ 17 ]. Later, surgeons used India ink to shade scars in patients with corneal leukoma. Cosmetic contact lenses are known to be the most commonly used method to improve aesthetic appearance [ 18 ]. However, people may be intolerant to wearing contact lenses, refuse the prosthesis for psychological reasons, or have chronic inflammation and infection [ 19 ].
But in the early stages of the formation of a pterygium, drug therapy is used.
To improve microcirculation in the eye and enhance fibrinolysis, drugs containing methylethylpyridinol hydrochloride are used: [ 20 ] Lakemoks, Emoksipin, Emoksifarm. Method of application: instillation into the conjunctival sac (three times a day, one or two drops). The duration of treatment is determined by the doctor. Drops can cause temporary itching, burning and redness of the eye.
Eye drops for cataracts such as Carnosine (Sevitin), Taurine (Taufon), Hilo-care (with sodium hyaluronate and dexpanthenol), and the Ayurvedic remedy Uzala (Ujala) may also be prescribed. Drops with glucocorticosteroids are used, in particular with dexamethasone (reduces neovascularization and lymphangiogenesis, improves the barrier function of the eye), [ 21 ], [ 22 ] hyaluronidase. [ 23 ]
The anti-scar preparation Collalizin (in the form of a lyophilisate for the preparation of a solution) is used by electro- and phonophoresis. [ 24 ] Physiotherapeutic treatment is also carried out using another proteolytic enzyme - lidase, corticosteroids (hydrocortisone) and potassium iodide solution.
It is recommended to take vitamins, primarily ascorbic acid (vitamin C accelerates the proliferation of corneal epithelial cells and the healing of epithelial defects) [ 25 ], tocopherol acetate [ 26 ], [ 27 ], and thiamine. [ 28 ] For more information, see - Vitamins and Vision
It should be borne in mind that treating a cataract at home does not make it disappear, and that dripping onion juice (mixed with honey or milk) into the eyes is useless and dangerous, since this “folk remedy” can cause additional irritation of the cornea and retina.
There is no clinical evidence of the effectiveness of herbal treatment, in particular, washing and instilling eye drops with decoctions of eyebright (Euphrasia officinalis), golden mustache (Callisia fragrans) and blue cornflower (Centaurea cyanus). Although these medicinal plants, including onion juice, [ 29 ] can be used as an adjuvant for inflammation of the conjunctiva of the eye.
Prevention
There is another phraseological unit – “to protect like the apple of one’s eye”, that is, to try to preserve something important. The cornea is the most important structure of our eyes: before light reaches the photoreceptors of the retina, it must pass through the cornea, and therefore it must remain transparent.
Prevention of corneal leukoma includes early detection and treatment of corneal inflammation (herpetic or bacterial keratitis), dry eyes; use of protective glasses at work, eye protection from ultraviolet radiation, etc.
Forecast
In the case of an old leukoma, the prognosis depends on the effectiveness of its treatment. But from the point of view of etiology, the formation of a scar on the cornea is directly dependent on the diseases that affect the cornea, as well as the severity and nature of the damage.

