Medical expert of the article
New publications
Eustachyitis
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
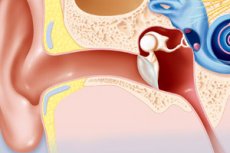
When it comes to diseases of the hearing organ, one diagnosis that usually comes to mind is otitis media (inflammation of the middle ear). In fact, the hearing aid is a rather complex system consisting of several important structures. The damage to each of them has its own name. So labyrinthitis is an inflammation of the inner ear, and the diagnosis of "external otitis" indicates the localization of inflammation in the area of the auditory canal from the ear drum to the eardrum. But what is eustachyitis of the ear? After all, this disease also belongs to the sphere of activity of ENT doctors.
One of the causes of hearing loss
Eustachitis (another name for turbo-otitis) is one of the diseases of the hearing organ of inflammatory nature. The disease has a clear localization in the eustachian tube, which is an extension of the external auditory canal and connects one of the important structures of the hearing organ (tympanic cavity) with the nasopharynx.
The Eustachian tube is an auditory canal in the middle ear that performs several functions at once:
- Drainage of mucous membranes and removal of exudate (the ear mucosa produces a secretion that helps moisturize and remove dust, foreign substances, dying epithelial cells from the ear canal),
- Air exchange between the tympanic cavity and the nasopharynx, which takes place during swallowing (at this moment the lumen of the tube expands),
- Maintaining a balance between the pressure in the tympanic cavity and the external atmospheric pressure (this is necessary for proper conduction of the vibrations of the tympanic membrane to the labyrinth of the inner ear),
- Production of antimicrobial secretion (multiple epithelial glands, the number of which increases closer to the pharynx, provide antimicrobial defense of the ear and nasopharynx).
Any violation of the functionality of the auditory canal is accompanied by an inflammatory process. And damage to the mucous membrane of the eustachian tube, located in the middle ear, easily turns into otitis media.
Disturbance of the balance of external and internal pressure changes the auditory sensation, so the main complaint in eustachyitis is deterioration of hearing, a feeling of deafness, discomfort inside the ear when talking.
Causes of the eustachyita
The causes may be different, but the mechanism of disease development remains constant and consists of several stages:
- As a result of complete or partial impairment of the patency of the auditory tube (and it has a diameter of only 2 mm, so even a small swelling becomes a big problem) worsens or stops ventilation of the tympanic cavity.
- The air remaining in it is sucked in, the pressure inside is reduced, causing the eardrum to retract.
- Due to the reduced pressure in the tympanic cavity there is an effusion of transudate, which contains fibrin, protein, and then cells involved in inflammatory reactions, catarrhal inflammation develops.
- Congestion prepares the ground for multiplication of conditionally pathogenic and pathogenic microorganisms, which are always in our body, or get into it from outside (in most cases, infection from the throat and nose spreads to the eustachian tube and middle ear). On the background of low immunity, the catarrhal form of the disease easily passes into purulent otitis media, while eustachitis remains as a concomitant disease.
- The inflammatory process, provoked by microbes, is accompanied by swelling, which further impedes ventilation, does not allow the auditory tube to normally perform its function of maintaining pressure balance, and this in turn is accompanied by hearing impairment. Prolonged inflammation becomes a risk factor for the development of adhesions.
But why do some people develop inflammation when exposed to the same factors, while others do not? And here already a big role is played by such moments as:
- Weak immunity (usually a consequence of chronic diseases),
- Improper diet,
- Immunodeficiencies,
- Poor social conditions, lack of body and hand hygiene,
- Allergic predisposition,
- Frequent blowing of both nostrils at the same time in prolonged runny nose,
- Chronic cough, frequent sneezing fits,
- Childhood, when immunity is not yet strong enough and adenoid growth is often diagnosed.
As you can see, eustachitis is a multifactorial disease, although according to statistics, most often the disease is still a complication of infections of the ENT organs. The primary disease in any case reduces the body's resistance to infection, and improper treatment only opens the way for it to go deeper.
It should not be surprising that children are sick with turbo-otitis (eustachyitis) more often than adults and their disease has a more pronounced acute course.
Risk factors
External factors worth mentioning include:
- Improper treatment of inflammatory diseases of the throat and nose, especially of infectious nature (sore throat, acute respiratory viral infections, influenza, measles, pharyngitis, whooping cough, rhinitis, sinusitis), eustachitis can be called one of the frequent complications of the common cold,
- Medical procedures (prolonged nasal tamponade to stop bleeding, surgical treatment of ENT organs and aftercare),
- Pressure drop (rapid immersion or ascent from deep water, airplane flight: ascent and landing, airplane crashes, explosions and contusions).
Any of the above-mentioned causes is a risk factor for the development of eustachyitis. Their influence does not always lead to ear disease, but definitely increases the risk of the disease.
Pathogenesis
In the pathogenesis of eustachianitis, doctors consider several groups of factors that can cause inflammation of the eustachian tube. To internal factors can be attributed:
- Abnormalities of the ear and nasopharynx (deviated nasal septum, hypertrophy of the lower nasal bones, irregular shape or narrowing of the eustachian tube, etc.),
- Neoplasms (enlarged adenoids, nasal polyposis),
- Allergic reactions (chronic inflammation of nasal mucous membranes - vasomotor rhinitis),
- Wisdom teeth growth accompanied by severe inflammation.
Symptoms of the eustachyita
Since the disease can be caused by different causes, the clinical picture of eustachyitis of different types can be somewhat different. This is especially noticeable at the initial stage of the disease. The first signs of infectious turbotitis can be considered symptoms of the underlying disease, which are localized in the area of the lesion: runny nose, cough, sore throat.
Primary(catarrhal) eustachitis has a very different beginning, although in most cases at first everything is limited to a slight discomfort in the diseased ear, a feeling of its congestion, extraneous noises.
Common signs of acute otitis media in adults are:
- Hearing changes (impaired hearing, especially perception of low frequencies, noise and ringing in the ear),
- Headaches, less often ear pain,
- Distorted perception of the sound of one's own speech (autophony), the sound seems to echo in the ear, causing pain,
- The sensation of water pooling and overflowing in the ear.
Less often, patients complain of heaviness in the eye area, difficulty breathing, dizziness.
Patients claim to feel some relief when chewing, yawning, swallowing saliva, eating, or tilting the head. This is due to a short-term opening of the lumen of the eustachian tube and a change in the level of fluid. Vasoconstrictor drops can also help.
Acute non-infectious eustachitis can go away on its own, but this does not mean that the disease should be ignored. After all, the infection can join later, because often the causative agents of purulent inflammation are opportunistic pathogens (streptococci, staphylococci, etc.) living on the surface of the skin and mucous membranes.
Eustachitis in a baby
Usually occurs in an acute form with distinct symptoms:
- Ear/ear stuffiness(constant or intermittent),
- Mild dull pain in the ears,
- Painfulness when speaking, caused by amplification of the sound of one's speech, "echo" of one's own voice,
- A sensation of water overflowing in the ear that keeps coming back,
- Children and adults may also complain of a lump in the throat.
Headaches, nausea, balance problems, and dizziness are more common in children than in adults with eustachyitis. The temperature rises rarely and to subfebrile values.
Infants have a subfebrile temperature more often, the baby feels unwell, becomes tearful, cranky, may refuse to eat. The child does not sleep well, looks lethargic, often regurgitates after eating.
In the chronic form of the disease, the symptoms are less pronounced. They intensify with an exacerbation. The clinical picture expands if eustachitis is complicated by otitis media. In this case, other symptoms may appear:
- A rise in temperature,
- Dizziness and headaches,
- Increased ear pain,
Decreased hearing acuity is a fairly specific symptom of prolonged eustachyitis. However, patients get used to it and do not seek help until other unpleasant manifestations of the disease appear.
Forms
The inflammatory process in eustachitis most often affects only one side of the paired hearing organ. If the right side is affected, right-sided eustachitis develops, while left-sided eustachitis is diagnosed when the eustachian tube of the left ear becomes inflamed. But there are cases when inflammation spreads to both ears at once. In this case, we speak of bilateral e ustachitis.
So, according to the localization of inflammation, eustachyitis can be divided into uni- and bilateral. But there are other signs by which the disease is classified:
Form of flow (stages):
- Acute eustachitis (up to 3 weeks)
- Subacute eustachitis (up to 3 months),
- Chronic form (as a consequence of severely weakened immunity, improper treatment or lack thereof)
Etiology (causes):
- Infectious,
- Allergic,
- Traumatic, including barotraumas: air (aero-otitis) and underwater (mareotitis).
The acute form of the disease is characterized by the severity of symptoms, so it is simply impossible not to notice it. It represents an active inflammatory process, most often transferred from the pharynx or nose. It is always accompanied by severe swelling, but with the right approach to treatment, it passes within a week.
Chronic eustachitis can be asymptomatic, but its complications are more dangerous. If acute turbo-otitis is left untreated, it can easily turn into chronic turbo-otitis and cause hearing loss.
Barotrauma-related eustachyitis is the bane of divers, divers, pilots, and those who use airfreight services. The pressure differential can cause the eardrum to become depressed. If nothing is done, a non-infectious inflammatory process develops.
Complications and consequences
Acute eustachyitis is an unpleasant disease, the timely treatment of which makes it possible to restore the functionality of the auditory tube in just a week. If the disease has a catarrhal form, it is believed that it can pass on its own, when the inflammation, not supported by microbes, subsides. But the very impairment of ventilation and stagnation of exudate and transudate within the ear can cause the bacterial complication of eustachyitis, which without treatment can spread further to the middle and inner ear. And damage to the inner ear can lead to permanent hearing loss and even deafness.
Infectious eustachitis must be treated, especially if it is a consequence of an untreated cold of a bacterial nature, such as sore throat, whooping cough or adenoiditis. The growth of adenoids is associated with inflammation of lymphoid tissue, where multiple pathogens accumulate. Enlarged adenoids themselves can block the mouth of the eustachian tube, disrupting its drainage and functionality, causing hearing impairment. They can also become a source of infection for the whole body, which can spread not only to the nasopharynx, but also inside the hearing organ.
All this is very unpleasant, but doctors have developed an effective treatment for turbootitis of any etiology. If nothing is done or inadequate treatment is carried out, the disease can be prolonged. Complaints that eustachyitis does not pass, in most cases are associated with improper treatment. Not only that a person for a long time remains obsessive symptoms of noise and gurgling in the ears, their own conversation causes discomfort and pain inside the hearing organ, so a long-lasting inflammatory process becomes in addition and the cause of adhesions.
Given the extremely small diameter of the eustachian tube, it is clear that even small fibrous tissue tracts within it will be an obstacle to normal ventilation and secretion. They will not "dissolve" on their own, they will have to be surgically removed, otherwise there will be a gradual decrease in hearing up to deafness.
The same is seen if the inflammation spreads to the structures of the inner ear and labyrinthitis develops.
The feeling of stuffy ears and impaired hearing in eustachian syndrome can persist for quite some time, even after treatment has been successfully completed. Understandably, many people are concerned about when will their hearing return?
Doctors cannot give a definite answer to this question. In some patients, hearing loss is noted within 1-3 weeks in the acute, adequately treated form of turbo-otitis. In the complicated course of this may take months: in most cases up to 3, but it happens that deafness does not pass even within six months. Chronic form causes a gradual adhesion of the walls of the eustachian tube due to adhesions, hearing worsens and independently can not come back to normal. Any exacerbation only aggravates the situation. So inflammation is dangerous even in the case of a strictly localized process in the ear canal.
Diagnostics of the eustachyita
Most patients diagnosed with eustachitis come to the doctor with complaints of sore throat, runny nose and other symptoms of a cold or were treated for it the day before. And only when there is a pronounced blockage of the ears, discomfort and distorted perception of the sound of his voice, a person begins to think that the disease is not the nasopharynx, and the hearing organ. And since it is a complex organ and the pathological process can be localized in different parts of it, it is impossible to make an accurate diagnosis without the help of specialists.
Diagnosis and treatment of the ENT organs is performed by an otolaryngologist. He performs a physical examination of the patient, listens to complaints, examines the state of the sinuses, pharynx, pharynx, tonsils (rhino-, laryngo- and pharyngoscopy). Collection of anamnesis largely helps to clarify the etiology of eustachyitis, because the treatment of infectious, allergic and traumatic turbo-otitis has its own features.
Standard tests do not give a complete picture of the disease. A blood test can only indicate inflammation, but its localization will remain a mystery. However, an immunoglobulin assay can provide enough information about the nature of the inflammation and the timing of its onset.
More specific will be a swab from the pharynx or laboratory examination of the separation from the nose and throat, where the pathogen is usually found. Symptoms in different types of turbo-otitis are similar, but the presence of pathogenic microflora in the smear allows you to say that the disease is infectious in nature and identify the causative agent in order to properly select medications. If allergic turbo-otitis is suspected, allergy tests are performed.
Otoscopy, during which such changes are detected, allows to diagnose impaired functionality of the auditory tube:
- Retraction of the tympanic membrane,
- Its clouding and redness,
- Light cone deformation,
- Narrowing of the ear canal.
Next is to examine the functionality of the auditory tube:
- To determine the patency of the auditory tube are used: Valsava test, blowing the auditory tube with a balloon Politzer (blowing the tympanic cavity under high pressure), Levy test, test with an empty throat and with clamped nostrils (Toynbee test).
- Ear manometry (tympanomanometry) examines the ventilation function of the auditory tube and measures the pressure in the tympanic cavity with a special ear manometer.
- Audiometry examines changes in hearing function (hearing loss usually occurs in low frequencies up to 25-30 dB). Speech tests and measurement of hearing acuity with an electroacoustic audiometer are used.
- Impedanceometry is an instrumental diagnostic method that provides information about the internal structures of the ear: middle ear, auditory tube, cochlea, auditory and facial nerves. It allows the localization of inflammation to be determined with great accuracy.
Since impaired patency of the eustachian tube may be associated with tumor processes, patients are prescribed additional examinations if such a suspicion arises. CT and MRI in eustachianitis allow to determine the presence and specify the localization of the tumor, without the removal of which it is impossible to restore the functionality of the auditory tube. Biopsy will answer the question: is it a benign neoplasm or a cancerous tumor.
Differential diagnosis
Eustachitis is a disease of the ear, most often a complication of other pathologies, so its clinical picture, especially at the beginning of the disease, can be blurred, unclear, with uncharacteristic manifestations. Differential diagnosis allows to make an accurate and definitive diagnosis, differentiating turbo-otitis from similar diseases in terms of symptoms.
Thus, maxillary sinusitis (inflammation of the maxillary sinuses) may be accompanied by headaches, stuffy nose and ears after blowing, a feeling of bloating, tinnitus, spreading from the sinuses to the eyes and internal structures of the ear. Identical symptoms are noted in eustachyitis, but rhinoscopy will reveal an accumulation of inflammatory exudate in the maxillary sinuses while the tympanic membrane remains intact.
A pressing feeling in the head, stuffy nose and ears, especially when blowing, are characteristic of different types of sinusitis, when one of the sinuses is inflamed. Like eustachyitis, the disease most often develops as a complication of respiratory pathologies of an infectious nature. Endoscopic examination of the nasal passages and otoscopy can accurately determine the localization of inflammation and exclude tubrootitis.
In laryngitis there is a sensation of a lump in the throat, which is also the case with eustachyitis, but there is no ear stuffiness, no sensation of fluid overflow, the voice itself changes (becomes hoarse or hoarse), but not its perception. Laryngoscopy reveals redness of the laryngeal mucosa and vocal cords, their swelling.
Otitis media is a frequent complication of eustachianitis, when inflammation from the eustachian tube spreads to middle ear structures that are in contact with it. This is characteristic of the infectious type of the disease. Not surprisingly, the diagnosis of eustachianitis is often made in conjunction with otitis media. The latter is characterized by quite severe pain in the ear (with turbo-otitis, the pain is usually insignificant), hearing loss, nausea (in children), increased body temperature with intracranial complications. Otoscopy shows a bulging, erythematous tympanic membrane and displacement of the light reflex.
If the mastoid process is involved, the diagnosis is "Mastoiditis ", the symptoms of which are similar to otitis media. Hearing loss in this disease is not always noted, and otoscopy does not show the picture characteristic of eustachyitis. Radiography and tomography of the temporal area help to clarify the diagnosis if there is doubt.
When diagnosing eustachitis, it is very important not only to confirm the diagnosis, but also to identify possible complications (otitis media, mastoiditis, development of hearing loss). If there is an inflammatory process in the nasopharynx, it will have to be treated simultaneously with the ears.
Who to contact?
Treatment of the eustachyita
Treatment of eustachitis can be started only after the nature of the inflammation has been determined. Bacterial inflammation requires the use of antimicrobial agents, fungal inflammation requires antifungal agents, viral inflammation requires strengthening of general and local immunity. The consequences of barotraumas suggest improving drainage (blowing), eliminating the consequences of hemorrhages and preventing the formation of pus in the auditory tube. But the treatment of allergic turbo-otitis is impossible without taking antihistamines that reduce the severity of non-infectious inflammation.
Read also:
Read more about the treatment of different types of eustachyitis. The goals of the therapeutic treatment of the disease are:
- Improving ventilation of the auditory tube,
- Controlling infection and preventing complications,
- Restoration of hearing and control of unpleasant symptoms of the disease.
Eustachitis, the causative agents of which are viruses, involves the use of immunostimulants and antiviral agents (Ingavirin, Ergoferon, Viferon). Viral turbo-otitis proceeds in a catarrhal form and often passes independently. But without a doctor to determine who caused the disease: viruses or bacteria, it is impossible. In addition, people with weakened immunity (for example, who have had a cold or children) are difficult to fight the disease on their own, and this opens the way to the attachment of bacterial infection, which must be treated with antibiotics.
Bacterial (purulent) eustachitis cannot be treated without antibiotics. Its cause can be streptococci, staphylococci, pneumococci and other pathogens with which the immune system can not cope. This can be understood already by the fact that bacterial turbotitis is secondary to respiratory infections. If the infection went from the throat or nose further into the interior of the body, it indicates a lack of defenses.
Antibiotics are prescribed after determining the causative agent of the disease, but most often, preference is given to drugs with a broad spectrum of action. Combined agents in the form of drops containing both antimicrobial components and anti-inflammatory drugs (GCS) are prescribed topically
Fungal forms of the disease are supposed to be treated with multicomponent preparations, which include an antimycotic (for example, "Candibiotic").
For all types of eustachyitis, including those caused by barotrauma, topical anti-inflammatory and analgesic agents are used to reduce inflammation and pain:
- GCS in combination with anesthetics (drops "Otipax"),
- Antihistamines ("Tavegil ", "Loratadine", "Suprastin ", "Claritin", "Diazolin"), which can be prescribed both for allergic eustachyitis and other types of eustachyitis to relieve inflammation and swelling.
- Vasoconstrictor drops ("Naftisin ", Vibrocil, Sanorin, and "Nazonex ") to help control swelling.
There is no unambiguous answer to the question of how long eustachitis is treated. Usually the disease passes within a week. But if we are talking about a bacterial infection, then you need to take into account that the course of antibiotic therapy can be different. Antimicrobial drugs are usually prescribed for a course of 5-7 days, but the question is when the patient began to take them, because not everyone hurries to see a doctor at the appearance of the first symptoms.
The fight against the disease can also be prolonged in the case of viral infections, when there is a risk of bacterial complications (e.g. In case of improper treatment or weakened immunity). A longer course is also characteristic of those whose bodies are weakened by prolonged, recurrent illnesses.
If eustachitis has become chronic, treatment is carried out in courses in case of exacerbations. In the period of remission it is necessary to carry out preventive measures aimed at strengthening the immune system.
Prevention
Eustachitis is a disease that is more difficult to treat than to prevent its development. Therefore, medical professionals recommend adhering to generally recognized preventive measures:
- Hardening as the basis of health and resistance of the body to infections.
- Healthy lifestyle: moderate physical activity, avoidance of bad habits.
- Strengthening the body through a set of physical exercises, regular walks in the fresh air, proper nutrition, rich in vitamins and minerals.
- Improving immunity and preventing respiratory infections: immunostimulants and vitamin complexes during epidemics, consumption of berries and fruits rich in vitamins C, A, E and others,
- Nasal rinsing immediately after contact with sick people or being in a crowded room during the period of increased incidence of acute respiratory infections.
- Timely and effective treatment of any infectious diseases, especially those involving the respiratory system. Sinusitis, rhinitis, maxillary sinusitis, pharyngitis, tonsillitis and other diseases can cause eustachitis and hearing loss. In any case, nasal congestion should not be ignored.
- Allergy treatment, i.e. Identifying the allergen and limiting contact with it. Preventive visits to an ENT doctor, especially during epidemics. This will help to detect the disease in its early stages, when symptoms are not yet present, and start its effective treatment.
- Pilots and crew, as well as divers, divers and others whose activities take place under conditions of fluctuating atmospheric pressure, should take measures to protect the hearing organ from sudden changes in pressure. Protect the ears from water entering the auditory tube when swimming in a pool.
Eustachitis often develops during childhood. Parents can be advised to take these measures to prevent the disease in their children:
- Take care to treat respiratory and respiratory system diseases in a timely manner.
- Dress your child for the weather and avoid overheating and hypothermia.
- Immunize your baby regularly according to the immunization schedule.
- Watch your child's diet, which should be nutritious, rich in vitamins and minerals.
- Don't forget to take regular walks. Ventilate the room both in summer and winter when the baby is not in the room.
- Breastfeed your baby in an upright position (this will reduce the risk of milk getting into the ears).
- Properly rinse your baby's nose when he or she has a cold. Use an aspirator to remove mucus from the nose for children who do not know how to blow their nose. Older children should be taught to blow their nose correctly, using each nostril in turn.
- Protect your child's ears from water when bathing in a bathtub, pool, or open water body. Explain that when diving, cover the nose and avoid pulling water into both nostrils.
- Remove adenoids in a timely manner and avoid long-term chronic inflammation of the tonsils. It is better to remove them and protect your child from chronic infections.
- Small children are better protected from pressure fluctuations (try to spare the child from flights, hitting the ears out of pampering, etc.).
Both children and adults should be treated for eustachitis only after a medical diagnosis. Medical examination will help to determine the cause of the disease, the degree of severity, possible complications. This will help not only to choose the right effective treatment, but also to avoid errors in the choice of methods and means.
Forecast
Doctors consider eustachyitis to be a complicated disease. However, with proper treatment, it can be resolved within a week. However, it may take longer to restore hearing. Moreover, the earlier the treatment is started, the lower the risk of hearing deterioration, normalization of which in severe situations is delayed even for six months, although in most cases it takes no more than 3 weeks.
If the disease is left untreated or treated incorrectly (e.g., warming the ear in the presence of purulent exudate or refusing antibiotics in the case of bacterial eustachyitis), there is a good chance that the disease will become chronic, with hearing loss becoming the norm.
Another option is the development of adhesive otitis media, which is accompanied by hearing loss, congestion and constant tinnitus. As a result, dense connective tissue, adhesions and fusions are formed inside the ear, which limit the mobility of the auditory ossicles and the sensitivity of the ear to sound (hearing loss develops). Treatment of the disease is long, and if it is ineffective, hearing aids, surgical intervention to dissect adhesions or their stretching are used.
The danger of infectious eustachitis is also due to the location of the hearing organ in the skull. The infection can spread deep into the organ itself and even reach the brain membranes, causing them to become inflamed. This outcome can be expected in childhood.

