Medical expert of the article
New publications
Basalioma of the eyelid
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
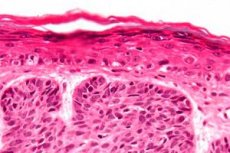
Basal cell carcinoma (basalioma) of the eyelid is the most common malignant disease, most often affecting elderly patients. Important risk factors are light skin that is unable to tan and chronic insolation. In 10% of cases, the lesions are localized on the head and neck, and in 10%, the eyelid is affected.
Insufficient treatment makes tumors more aggressive and difficult to treat.
 [ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 1 ], [ 2 ], [ 3 ], [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
Causes eyelid basaliomas
One of the following diseases in young patients can lead to the development of basal cell carcinoma of the eyelid.
Xeroderma pigmentosum is an autosomal recessive disorder characterized by progressive skin dispigmentation as a result of sun exposure. Patients have a characteristic bird-like facial appearance and are prone to basal cell carcinoma, squamous cell carcinoma, and melapoma, often multiple. Conjunctival malignancies have also been described.
Gorlin-Goltz syndrome (nevoid basal cell carcinoma syndrome) is a rare autosomal dominant disorder characterized by severe malformations of the eyes, face, bones, and central nervous system. Many patients develop multiple, small basal cell carcinomas during their second decade of life. There is also a predisposition to other malignancies, including medulloblastoma, breast carcinoma, and Hodgkin lymphoma.
 [ 11 ]
[ 11 ]
Symptoms eyelid basaliomas
Basalioma is the most common malignant tumor of the eyelid, accounting for 90% of all neoplasms. As a rule, the lower eyelid is affected. The affected areas (in decreasing frequency) are the medial canthus, upper eyelid, and outer canthus. The tumor is characterized by slow invasive growth without metastasis. Tumors located near the inner canthus often penetrate into the orbit and sinuses and, compared to tumors in other locations, are difficult to treat and are prone to relapse.
Nodular-ulcerative form - a shiny pearly node with small telangiectasias on the surface. In the initial period, basalioma grows slowly, in 1-2 years the tumor reaches a size of 0.5 cm in diameter. If the tumor is not recognized and treated at an early stage, with further rapid growth, an ulceration with ridge-like edges and dilated blood vessels on the sides (an "eaten" ulcer) occurs in its center. Over time, it can destroy a significant part of the eyelid.
The scleroeic form is less common and quite difficult to diagnose, since the tumor grows from under the epidermis in the form of a hard plaque, deforming the eyelid. The edges of the tumor are unclear, palpation reveals much larger sizes than visual examination. Upon superficial examination, the sclero-like form of basalioma can be mistaken for local chronic blepharitis.
What do need to examine?
How to examine?
Who to contact?
Treatment eyelid basaliomas
Complete tumor removal with maximum preservation of healthy tissue is recommended. When removing small basalioma, the tumor is resected within 4 mm of healthy tissue. Larger and more aggressive basaliomas of the SCC and KSZh types require a significant amount of radical surgical intervention. In this case, frozen section control is used using the standard method or micrographic surgery, which increases the success of the operation.
The standard frozen section control method is aimed at conducting a histological examination of the edges of the excised neoplasm during surgery to ensure complete removal of tumor tissue. If tumor cells are not detected in the section, the eyelid is reconstructed; if tumor cells are present, additional excision of the formation is performed.
Moh's micrographic surgery - removal with a series of frozen horizontal sections under the base of the tumor. The sections are color-coded or schematically coded to identify the undeleted areas of the tumor. Despite the length of the procedure, the examination increases the guarantee of complete tumor excision with maximum preservation of healthy tissue. This technique is especially useful in the case of tumors with difficult to detect borders or with finger-like outgrowths at the edges of the tumor, such as sclerosing forms of basal cell carcinoma, cystic fibrosis, recurrent tumors or tumors located in the area of eyelid adhesions.
Reconstruction technique
The choice of technique depends on the degree of horizontal resection, the size of the defect and the weakness of the eyelid. An important point is the restoration of the anterior and posterior plates of the eyelid. If one of the plates was damaged during the tumor removal process, it should be restored with similar tissue.
- Small defects, covering less than 1/3 of the eyelid, are usually sutured if the surrounding tissues are elastic enough to allow repositioning of the wound edges. If necessary, lateral cantholysis can be reconstructed using additional tissue if the defect cannot be sutured.
- Small defects, occupying less than 1/2 of the eyelid, are sutured using a Tenzel semicircular skin flap.
- Large defects, covering more than 1/2 of the eyelid, can be restored using one of the following methods.
- The Mustarde technique (taking a skin flap from the cheek) is used to close the defect of the lower eyelid. The posterior plate is restored with cartilage and mucous membrane of the nasal septum or mucous membrane of the cheek of the required thickness, or a Hughes flap;
- The eyelid splitting technique can also be used, but with caution. When restoring the lower eyelid, the function of the upper eyelid must be fully preserved.
- The diamond flap technique from the interbrow area is used to close defects located in the medial canthus and the middle part of the upper eyelid.
Indications for radiation therapy for basal cell carcinoma of the eyelid:
- Small nodululo-ulcerative basal cell carcinomas of the medial canthus in patients who are not candidates for surgery or in cases where the patient refuses surgery.
- Kaposi's sarcoma.
Contraindications to radiation therapy for basal cell carcinoma of the eyelid
- Basalioma of the medial canthus, as damage to the lacrimal canals by radiation therapy causes lacrimation.
- Upper eyelid margin swelling as subsequent keratosis causes discomfort.
More information of the treatment

