Mycoplasma pneumonia
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Causes of the mycoplasma pneumonia
Mycoplasmas are a special kind of microorganisms. They do not have a cell wall. In terms of morphology and cellular organization, mycoplasmas are similar to L-forms of bacteria, and are similar in size to viruses.
Twelve species of mycoplasmas have been isolated from the human nasopharynx and urinary tract, but three are pathogenic to humans: Mycoplasma pneumoniae, Mycoplasma hominis, Mycoplasma urealyticum.

M.pneumoniae affects the mucous membrane of the respiratory tract, and M.hominis and M.urealyticum - the urogenital system (causing the development of urethritis, cervicitis, vaginitis).
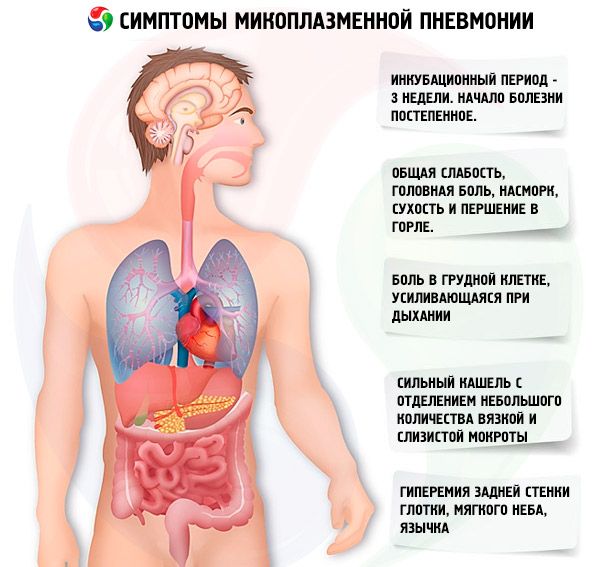
Symptoms of the mycoplasma pneumonia
Mycoplasma pneumoniae is a frequent causative agent of respiratory tract infections. In 1930, M. Pneumoniae was first isolated during the study of atypical pneumonia, and in 1962 it was characterized and classified as a separate type of bacteria.
The disease is transmitted by airborne droplets.
According to V.I. Pokrovsky (1995), all clinical manifestations of mycoplasmal pneumonia are grouped as follows.
- Respiratory
- upper respiratory tract (pharyngitis, tracheitis, bronchitis);
- pulmonary (pneumonia, pleural effusion, abscess formation).
- Non-respiratory
- hematologic (hemolytic anemia, thrombocytopenic purpura);
- gastrointestinal (gastroenteritis, hepatitis, pancreatitis);
- musculoskeletal (myalgia, arthralgia, polyarthritis);
- cardiovascular (myocarditis, pericarditis);
- dermatological (erythema polymorphic, other rashes);
- neurological (meningitis, meningoencephalitis, peripheral and cranial neuritis, cerebellar ataxia);
- generalized infections (polymymphoadenopathy, septicemia).
Mycoplasma infection has an incubation period that averages 3 weeks. The development of pneumonia is preceded by a clinic of lesions of the upper respiratory tract. The onset of the disease is gradual. Patients are worried about moderate general weakness, headache, runny nose, dry and sore throat, cough (dry first, then with the separation of viscous mucous sputum). Characteristic features of cough are its duration and paroxysmal character. During a coughing attack, its intensity is quite pronounced. Constant hyperemia of the posterior pharyngeal wall, soft palate, uvula. With the development of bronchitis, hard breathing and dry rales are heard. In case of mild mycoplasmal acute respiratory infections, predominantly catarrhal rhinitis and pharyngitis are observed. With moderate flow there is a combined lesion of the upper and lower respiratory tract in the form of rhinobronchitis, pharyngobronchitis, rinofaringobronchitis. Body temperature in patients is usually subfebrile.
These symptoms of mycoplasma infection increase by 5-7 days, the body temperature rises to 39-40 ° C and can hold on to these figures for 5-7 days, later on it decreases to subfebrile and lasts for 7-12 days, sometimes and longer. A characteristic feature of mycoplasma pneumonia is a long and strong cough with a small amount of viscous and mucous sputum. Cough lasts at least 10-15 days. The vast majority of patients also have chest pain, aggravated by breathing.
Physical signs of pneumonia usually appear on the 4-6 day of the disease and are characterized by focal weakening of vesicular respiration, crepitus, fine bubbling rales, shortening of percussion sound, but this is an infrequent symptom. Approximately 20% of patients with physical signs of pneumonia are not detected, lung damage is diagnosed only by X-ray.
In some patients, fibrinous or moderately severe exudative pleurisy may develop.
Where does it hurt?
What's bothering you?
Diagnostics of the mycoplasma pneumonia
X-ray mycoplasma pneumonia can have the following manifestations:
- strengthening and thickening of the pulmonary pattern, mainly interstitial changes in 50% of cases;
- segmental and focal infiltration of lung tissue (in 30% of patients); infiltrate is localized mainly in the lower pulmonary fields, less often - in the upper and middle lobes of the right lung, in the basal segments. Infiltrates are heterogeneous and inhomogeneous, without clear boundaries; in 10-40% are bilateral;
- extensive lobar infiltration (rare).

 [25], [26], [27], [28], [29], [30], [31], [32], [33]
[25], [26], [27], [28], [29], [30], [31], [32], [33]
Laboratory diagnosis of mycoplasma pneumonia
General analysis of peripheral blood is characterized predominantly by the normal number of leukocytes (no more than 8 x 10 9 / l), in 10-15% of cases - by leukopenia or leukocytosis; regular increase in the number of lymphocytes; lack of leukocyte shift to the left; increase in ESR.
It should be noted that mycoplasma pneumonia is often mixed (mycoplasma-bacterial) due to the attachment of bacterial microflora (mainly pneumococcus). This is usually the later pneumonia. Primary mycoplasma pneumonia develops in the first days of the disease. In general, the course of mycoplasma pneumonia is often not severe, but prolonged. However, in some cases, possible and severe; it is due to the severity of pneumonia itself or the addition of non-respiratory manifestations of mycoplasmal infection.
Diagnostic criteria for mycoplasma pneumonia
When making a diagnosis of mycoplasma pneumonia, the following main points should be considered.
- Gradual onset with a short prodromal period, acute pharyngitis, rhinitis, tracheitis, intense, prolonged cough with viscous, difficult to separate mucous sputum.
- Low severity of physical signs of pneumonia.
- The presence of extrapulmonary (non-respiratory) manifestations: hemolytic anemia, myocarditis, pericarditis, hepatitis, skin rashes, polylymphoadenopathy.
- Positive results of serological diagnosis. To confirm the diagnosis of mycoplasma pneumonia, the determination of antibodies to mycoplasma in the blood is performed using the complement fixation test, paired sera are studied with an interval of 15 days. The 4-fold increase in the antibody titer (not less than 1:64) is diagnostically significant.
Cultural diagnostics (sputum culture) with mycoplasmal pneumonia is practically not used due to the need to use highly selective media and the low information content of the method.
- Detection of mycoplasma antigens in sputum using monoclonal antibodies using the method of immunofluorescence or enzyme immunoassay. In recent years, the determination of mycoplasma (its DNA molecules) in the sputum has been carried out using the polymerase chain reaction method. With conventional bacterioscopy of sputum smear mycoplasma is not detected.
What do need to examine?
Who to contact?
Treatment of the mycoplasma pneumonia
Mycoplasma is highly sensitive to erythromycin and new macrolides (azithromycin, clarithromycin, etc.), and new macrolides are more effective than erythromycin, and are considered drugs of the first row. Tetracyclines are also effective in mycoplasma pneumonia. To β-lactam antibiotics (penicillins, cephalosporins) mycoplasma is stable.
More information of the treatment
Drugs

