Paracoccidia are the causative agents of paracoccidioidosis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Paracoccidioidosis (synonyms: South American blastomycosis, Lutz-Splendore-Almeida syndrome) is a chronic mycosis, characterized by the defeat of the lungs, skin, mucous membranes of the oral cavity and nose, a progressive course with the development of the disseminated form of the disease. Pathogen - Racoccidioides braziliensis.
 [1]
[1]
Morphology of paracocci
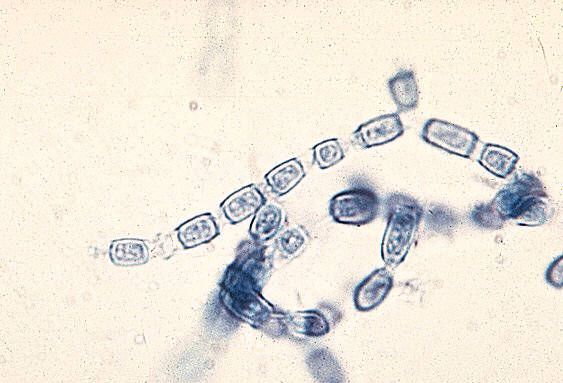
A dimorphic fungus that forms a yeast phase at 37 ° C. Yeast cells of large sizes (10-60 microns) with multiple kidneys 2-10 microns in diameter. Mycelial fungus thin septate, forms chlamydospores. Microconidia 2-3 μm in size.
Cultural properties of paracoccidia
The fungus is unpretentious to the nutrient substrate, actively multiplies in sterile soil, vegetable particles, water. On natural substrates (yeast extract, soil extract) there is intense sporulation. At 25 ° C it grows with the formation of hyaline hyphae, and at 37 ° C forms large spherical yeast cells with a lot of budding cells, which gives this structure a characteristic look of the "sea wheel".
Biochemical activity of paracoccidia
When yeast cells are grown in a nutrient medium, a fungicidal metabolite is accumulated, a phenol close in chemical structure and benzoic acid, causing protein denaturation.
Antigenic structure of paracoccidia
When growing on a liquid medium for 3 days, the mycelial form produces exoantigens 1,2,3 which can be determined by immunodiffusion in the gel.
Ecological niche of paracoccidia
Soil endemic areas in South America, especially in Brazil, as well as in Mexico and Costa Rica.
Stability in the environment of paracoccidia
The yeast phase is not very stable in the external environment. The mycelium is resistant to changes in pH, temperature fluctuations, drying. Very sensitive to the antagonistic action of the normal microflora of the environment.
Sensitivity to antibiotics
Paracoccidia are sensitive to ketoconazole, intraconazole, amphotericin B, trimethoprim / sulfamethoxazole.
Sensitivity to antiseptics and disinfectants
Paracoccidia are sensitive to the effects of commonly used antiseptics and disinfectants.
Pathogenesis of paracoccidioidosis
Infection occurs by microconidia. The lesions are located on the skin, the mucous membrane of the horny cavity, nose, in the lungs. Skin lesions are ulcerative, within which alternate areas of suppuration and scarring. With dissemination, the bones, adrenals, liver, brain, skin and mucous membranes are affected . In all the ballrooms, the spleen is involved in the inflammatory process.
Immunity cellular. The tension and duration of it have not been studied.
Epidemiology of paracoccidioidosis
The source of the causative agent of infection is the soil of endemic zones. The transmission mechanism is aerogenic, the transmission path is air-dust. The susceptibility of the population is unknown, among the diseased, rural residents predominate. Patients are safe for others.
Symptoms of paracoccidioidosis
Only people are ill. Painful ulcers are formed on the mucous membrane of the mouth or nose. Typically, the foci are multiple, less common are single pustular lesions or subcutaneous abscesses. Ulcerous lesions of the skin and mucous membranes are accompanied by an increase in regional lymph nodes. Pulmonary lesions are accompanied by such symptoms as: cough, chest pain, the formation of infiltrates.
Laboratory diagnostics of paracoccidioidosis
The investigated material is pus, cerebrospinal fluid, sputum, urine, punctate lymph nodes.
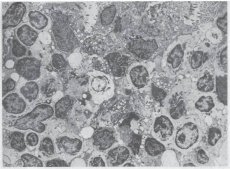
At a microscopic examination, the dye or Gram stain, Romanovsky-Giemsa and other methods are examined for smears from the test material. Mushroom cells are large, have a round or ellipsoidal shape and thick walls. The mother cell is surrounded by small daughter kidneys, looks like a crown. Similar cells are detected in tissue sections. The morphology of the yeast phase is very characteristic, therefore when diagnosed with such fungal cells, the diagnosis is unquestionable.
To isolate a pure culture, the material is inoculated onto nutrient media with carbohydrates, blood and serum agar, which are incubated at 25-30 and 37 ° C to obtain respectively mycelial and yeast colonies. The causative agent grows slowly, forming in 3 weeks a colony resembling a yeast.
Bioprobo is placed on mice or guinea pigs, infecting them with intraperitoneally studied material and isolating a pure culture from their internal organs.
Serologic testing determines antibodies in the serum of patients in the RP, ELISA, or DSC, especially at late stages of the disease. Diagnostic value have RP and DSC.
An allergic test is made with an allergen from the tissue form of the fungus.

