Knee-joint
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The knee joint (art genus) is the largest and most complex in structure. It is formed by the femoral, tibial bones and patella. The articular surfaces of the medial and lateral condyles of the femur are articulated with the upper articular surface of the tibia and the patella. Inside the joint, there are semilunar forms of intraarticular cartilage - lateral and medial menisci, which increase congruence of the articulating surfaces, and also perform a cushioning role.
The lateral meniscus (meniscus lateralis) is wider than the medial meniscus (meniscus medialis). The lateral margin of the meniscus is fused with the capsule of the joint. The inner thinned end of the meniscus is free. The anterior and posterior ends of the meniscus are attached to the intercondylar elevation of the tibia. The anterior ends of the meniscus are joined by the transverse ligament of the knee (lig. Transversum genus).
|
Read also: |
Articular capsule of the knee joint is thin. On the femur, it is attached, retreating approximately 1 cm from the edges of the articular surfaces, on the tibia and patella - along the edges of the joint surfaces. The synovial membrane forms several folds containing adipose tissue. The largest paired pterygoid folds (plicae alares) are located at the sides of the patella. From the patella to the anterior intercondylar field, vertically downwards there is an unpaired subperiar synovial fold (plica synovialis infrapatellaris).

Knee joint ligaments
The knee joint is strengthened with ligaments. The collateral ligament collateral ligament (lig. Collaterale fibulare) is extra-capsular, from the lateral epicondyle of the femur to the lateral surface of the fibular head. The tibial collateral ligament (lig. Collaterale tibiale), fused with the capsule, begins on the medial epicondyle of the femur and is attached to the upper part of the medial edge of the tibia. On the posterior surface of the joint is an oblique poplite ligament (lig. Popliteum obliquum), which is the final bundles of the tendon of the semimembranous muscle. This ligament is woven into the back wall of the articular sac, and also attached to the posterior surface of the medial condyle of the tibia.
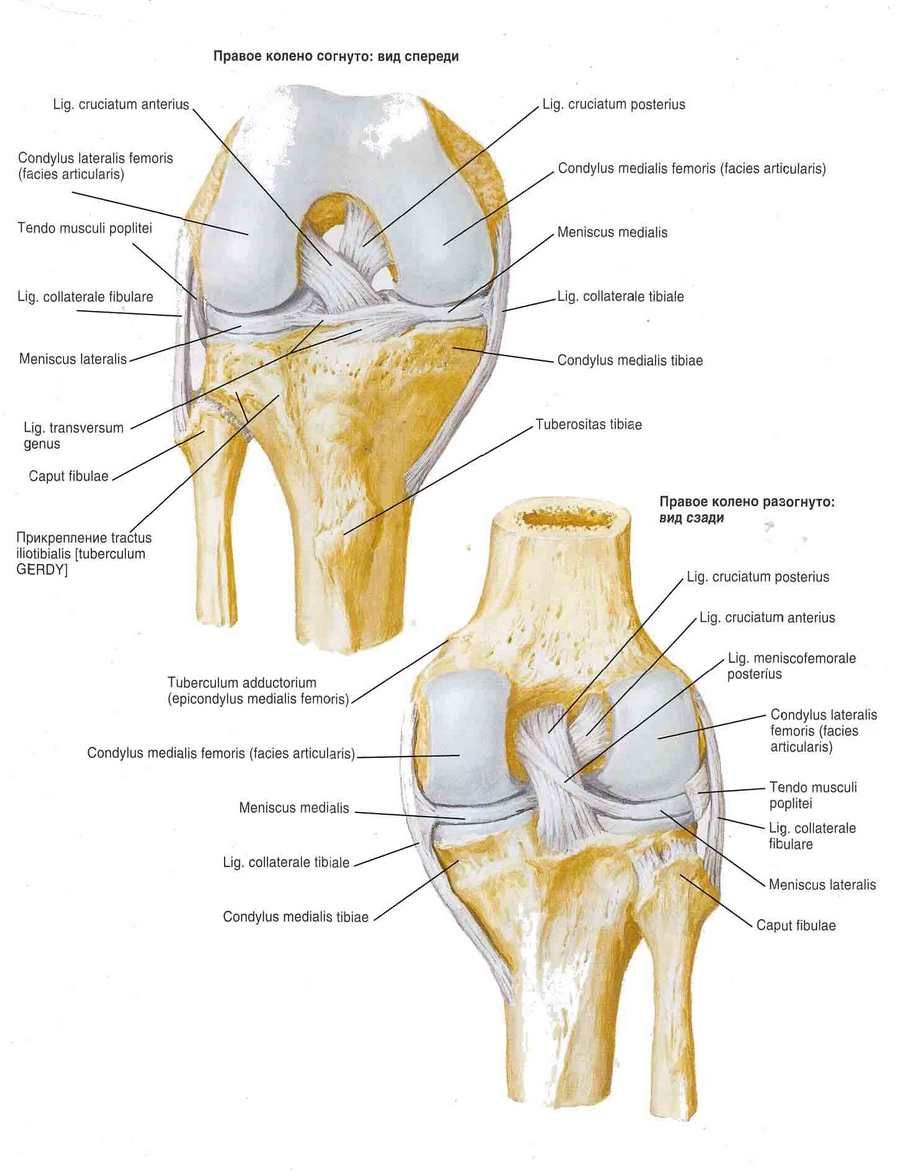
An arched popliteal ligament (lig. Popliteum arcuatum) begins on the posterior surface of the fibular head, flexes medially and is attached to the posterior surface of the tibia. In front, the joint capsule is strengthened by the tendon of the quadriceps muscle of the thigh, which was called the patellar ligament (lig. Patellae). The inner and outer bundles of the tendon of the quadriceps femoris, extending from the patella to the medial and lateral epicondylitis of the femur and to the tibial condyles, are called the medial and lateral supporting patellar ligaments (retinaculum patellae mediate et laterale).
In the cavity of the knee joint there are cruciate ligaments covered with synovial membrane. The anterior cruciate ligament (lig. Cruciatum anterius) begins on the medial surface of the lateral condyle of the thigh and is attached to the anterior intercondylar field of the tibia. The posterior cruciate ligament (lig. Cruciatum posterius) is stretched between the lateral surface of the medial condyle of the thigh and the posterior intercondylar field of the tibia.
The synovial membrane of the knee joint
The knee joint has several synovial bags. Their number and sizes vary individually. Synovial bags are located mainly between the tendons and under them near the place of attachment of the tendons to the bones. The nadnadkolennikovaya bag (bursa suprapatellaris) is located between the tendon of the quadriceps femoris and femur. A deep podadnikolnikovaya bag (bursa infrapatellaris profunda) is located between the patellar ligament and the tibia. Under the tendon bag of the sartorius muscle (bursa subtendmea m. Sartorii) is located near the place of attachment of its tendon to the tibia. The subcutaneous prednadolkovnikovaya bag (bursa subcutanea prepatellaris) is located in the fiber layer in front of the patella. The popliteal recessus (recessus subpopliteus) is located behind the knee joint, under the tendon of the popliteal muscle.
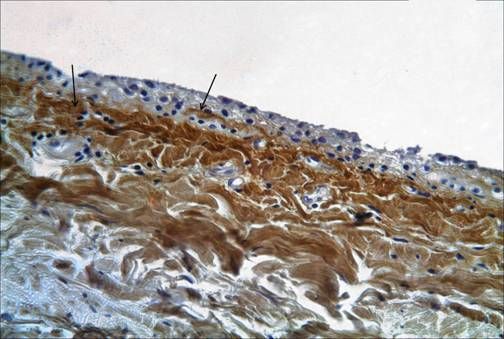
The synovial membrane lining the non-bony surface of the joint and differs from the mesothelial lining of other body cavities. It is not a true epithelial tissue. According to histological signs, there are three types of synovial tissue: synovial lining of alveolar surfaces, fibrous surfaces and adipose. The synovial membrane covering the cruciate ligaments is innervated well enough and is abundantly supplied with blood. In addition, there are macroscopic synovial structures in the knee joint that have a certain significance - folds or plics. The following most significant folds are distinguished: suprapatulatory, infra-papular, mediopathic and lateral folds. The most common is the suprapatellite plica (in 90% of cases). The synovial folds themselves have little surgical significance, however, for various pathological conditions they can increase in size, thicken, losing elasticity, which in turn leads to restriction of movements in the joint, especially flexion. Sometimes inside the synovial folds are hidden intraarticular bodies.
Infragmatic plica (lg. Mucosum) is an embryonic septum between the medial and lateral parts of the joint. With her hypertrophy, it is extremely difficult to visualize the different parts of the joint during arthroscopy. The most often surgical treatment is the mediapatulatory fold, which starts on the medial side of the joint, passes laterally and enters the medial part of the synovial capsule, covering the infra-papular fat pad. The frequency of its presence in the joint varies from 18 to 55%.
Meniscus of the knee joint
The meniscus of the knee joint is located in the joint cavity and serves to maintain and protect the cartilage. In addition to damping functions, the meniscus maintains the correspondence between the forms of articulating joint surfaces of bones, and also reduces friction in the joints. Most knee injuries occur in the joint meniscus. With such injuries, mobility is limited, pain occurs, and in severe cases cartilage is damaged and arthrosis develops. Damage to the meniscus can be combined with rupture of ligaments, bone injuries, which requires immediate medical attention.

Depending on which meniscus is damaged, external or internal, these types of injuries are distinguished:
- Detachment of the meniscus from the capsule
- A break in the meniscus (more often seen in the inner meniscus, may be longitudinal or transverse)
- Compression of the meniscus (usually occurs in the outer meniscus)
A meniscus rupture can be triggered by a knee injury, an awkward, abrupt movement, for example, during a jump. Most often, such injuries occur among athletes. The prognosis of the outcome of the disease depends on the severity of the lesion, its location, and also on the condition of the tissues. In chronic pathologies of the knee joint, the meniscus tissues can degenerate into fibrous growths, may thin out and exfoliate. Cartilage tissue in this case loses its functions, which leads to the development of arthrosis of the knee joint.
If the meniscus is damaged, the following symptoms may appear: difficulty in moving, especially when climbing or descending the stairs, accumulation of fluid in the joint, muscle tissue atrophy, clicking sound in the knee, local temperature increase in the affected area, pain in flexing-extension of the knee, swelling .
Depending on how bad the disease is, prescribe a treatment that can be both conservative and surgical. Conservative treatment includes the use of methods of physiotherapy, the patient is recommended to be at rest, ice can be applied to the affected area and elastic bandages applied. In case of large ruptures or separation from the capsule of a part of the meniscus, as well as in case of ligament damage, treatment can be performed surgically by means of arthroscopic methods. The period of full recovery of the motor ability of the joint can vary from several weeks to two to three months.
According to the shape of articular surfaces this joint is condylar. Around the frontal axis, flexion and extension (total volume 150 °) occur in it. When the shank is flexed (due to relaxation of the collateral ligaments), its rotation relative to the vertical axis is possible. The total volume of rotation reaches 15 °, passive rotation - up to 35 °. Cross-shaped ligaments inhibit pronation, while performing supination they relax. Supination is inhibited mainly by the tension of the collateral ligaments. Flexion is limited by the tension of the cruciate ligament and the tendon of the quadriceps muscle of the thigh.
Active and passive knee joint stabilizers
The mechanisms of knee joint stabilization at various settings of the thigh, shin, in statics and dynamics, in norm and in pathology have been the focus of researchers for many years, but not all is clear in this issue at the present time.
For convenience of consideration these mechanisms are divided into passive and active. The first include congruence of articular surfaces and cartilaginous structures, as well as its capsular-ligamentous apparatus of the knee joint, which reacts passively to the shin displacement. To the second - okolosustavnye muscles, which render this active resistance. In reality, they work simultaneously, mutually complementing and / or replacing each other. When injuries of capsular-ligament structures in one way or another, both mechanisms are constantly or temporarily disrupted, as a result of which the function of the joint suffers - its instability is noted.
Stabilization of the knee joint is one of those problems, the solution of which is possible only with the use of data obtained in various fields of knowledge (morphology, physiology and biomechanics).
In order to determine which links of the pathogenesis of a given process can be influenced, restoring a disturbed function, it is necessary to consider the mechanisms of knee joint stabilization. In addition, it is important to answer the question of which way to go. Do you expect to recover or compensate for the function? In which cases to choose conservative tactics, and in what operative treatment and what is the role of functional therapy in these cases?
The solution of these fundamental questions is possible only with a careful examination of the peculiarities of the biomechanics of the knee joint.
Movement in the knee joint
Around the frontal axis up to 135 ° (flexion) and up to 3 ° (extension). Turn of the shin around the longitudinal axis - up to 10 °.
Flexes the shin: biceps femoris, semimembranous muscle, semitendinous muscle, popliteal and gastrocnemius muscles.
Turn the shin to the inside (with the knee bent): semimembranous and semitendinous muscles, sartorius muscle and calf muscle (medial head).
Turning the calf outside: gastrocnemius muscle, biceps femoris (lateral head).
Basic diseases of the knee joint
 [10], [11], [12], [13], [14], [15], [16],
[10], [11], [12], [13], [14], [15], [16],
Deforming arthrosis of the knee joint
This is a chronic disease in which degenerative processes occur in the bone and cartilage tissues, leading to deformation of the joints. The main signs of deforming arthrosis: pain increases during movement, increases in damp and cold weather, usually weakens at rest. The older the person becomes, the higher the likelihood of developing the disease. This is due to the fact that the cartilage tissues inside the joints wear out over time and are increasingly difficult to recover from injuries and physical exertion. In the development of the disease, an important role is played also by hereditary factors.
Deforming arthrosis of the knee joint is accompanied by a crunch when moving, which eventually passes, as during the process of rubbing the surface of the bones is smoothed. In the knee joint inflammation develops, cysts appear in the bone tissue, the patient is difficult to move, when walking, he begins to limp. The course of the disease is aggravated by physical overload, prolonged stress on the feet, for example, in people whose professional activity involves a long stay in standing position - from sellers, teachers, athletes,
Deformation of the joint begins to develop, as a rule, in the second stage of the disease. On the third - joints are expanded and deformed so much that the joint becomes absolutely motionless.
Arthritis of the knee joint
Arthritis of the knee joint is divided into osteoarthritis, rheumatoid arthritis and post-traumatic arthritis. The most common form of knee arthritis is osteoarthritis. This disease progresses gradually, depleting the articular cartilage. Osteoarthritis is common in elderly and middle-aged people. Osteoarthritis, or gonarthritis, of the knee joint affects the periarticular muscles, including the synovial membrane, ligaments as a result of the inflammatory process in the soft tissues.
Rheumatoid arthritis of the knee joint
It can occur both in an acute form and differ in the chronic course of the disease. In the acute stage of the disease, fluid accumulates in the cavity of the knee joint. The patient feels pain, redness and swelling in the knee joint. The motor activity of the joint is shortened, the patient tries to keep his foot in a half-bent state. If pus formed in the joint, the disease proceeds with a high fever and chills. The swelling of the joint is very pronounced. As a rule, with this form of disease, two knee joints are affected.
Post-traumatic arthritis of the knee joint
Occurs when a knee joint is injured and can develop over the years, gradually destroying the articular cartilage, causing painful pain and limiting the function of the joint.
Pain in the knee joint
Pain in the knee joint is accompanied by the following symptoms:
- Increases while walking on stairs
- Limits the motor activity of the joint, increases when trying to bend or unbend the leg
- Accompanied by a crunch when moving, the appearance of swelling
- Articular surfaces are deformed
- Atrophy of the thigh muscles
- There is an uneven climbing gait
Pain in the knee joint often occurs also with coxarthrosis or osteoarthrosis of the hip joint.
How to inspect the knee joint?
Examine the patient lying on his back with legs outstretched. Is there any swelling in the area of the knee joints? ( Its causes are : thickening of the bone, accumulation of fluid in the joint cavity, thickening of the synovium of the knee joint, in the latter case, palpation is felt "friction".) Note whether there is atrophy of the quadriceps. The presence of fluid in the cavity of the knee joint can be confirmed by this method: put the palm of one hand on the patella, or rather, the area just above it, and the thumb and index fingers of the other hand are below the patella. Changing the degree of pressure on the patella, the investigator causes the fluid to move in the cavity of the knee joint, which it senses with the fingers. If there is 30-40 ml of fluid in the joint cavity, then the phenomenon of ballotation of the patella can be caused, and its jerking about the surrounding bones ("kneeling") is felt. These "tapping" may be absent if the effusion is very small or if it is "tight", but its volume exceeds 120 ml.
The degree of flexion and extension in the knee joints varies in different people. Flexion is considered quite sufficient, if a person can touch the buttock with a heel. Compare the extension of the knee joints to the diseased and healthy limbs. The condition of the medial and lateral ligaments is examined with an almost completely unbent knee joint. With one hand, the examiner raises the leg of the patient lying on the couch, by the ankle, and the other slightly fixes the knee. The ligaments of the knee joint strain at the time of withdrawal, while attempting to take the lead, holding the ankle of the test leg with one hand, and the other hand under the ridge, push the knee joint in the medial direction (this is a test for the medial ligaments). Reverse manipulation with reduction in the knee joint is a test for lateral ligaments. If these ligaments are torn, then the knee joint "opens" more widely when examining the corresponding ligaments (be sure to compare the knee joints on both extremities).
Cross-shaped ligaments are examined by fixing the knee joint at an angle of 90 °. The foot of the leg being examined is located on the couch, and the investigator sits down on it to immobilize the large tibia. Grasp the knee back with your fingers so that your thumbs lie on the condyles of the femur. With the relaxed quadriceps femoris, the anteroposterior transition of the tibia is evaluated, on the thigh (about 0.5 cm in norm), the anterior cruciate ligament limits the hip slip forward, and the posterior one - back. Excessive slip in one direction (be sure to compare with the knee of the other leg) may indicate damage to the corresponding ligament.
Rotary test McMurray is designed to detect pedunculated (ie, with the preservation of the legs) tears of the meniscus. The knee joint is bent, the tibia rotates laterally, and then the knee joint is bent as the tibial bone continues to rotate. Reception is repeated several times at different degrees of flexion in the knee joint, and then again with rotation of the tibia on the thigh. The purpose of this manipulation is to press the free end of the pedunculated meniscus inside the joint. When the knee is straightened, the pressed end of the meniscus is released, and this is accompanied by a sensation of a kind of a click (sometimes audible), and the patient then notices the pain. This method does not, however, reveal breaks in the "bucket handle" type. Remember: when moving in the normal knee joint, it is usually audible to click the patella.
Arthroscopy of the knee joint
Arthroscopy of the knee joint made it possible to examine the internal structures of the knee joint, which makes it possible to establish an accurate diagnosis and diseases that cause pain in the knee without opening the joint. With the help of this method, it became possible to perform a number of surgical interventions in a closed joint, which undoubtedly shortens the period of convalescence for persons subjected to arthroscopic surgery.
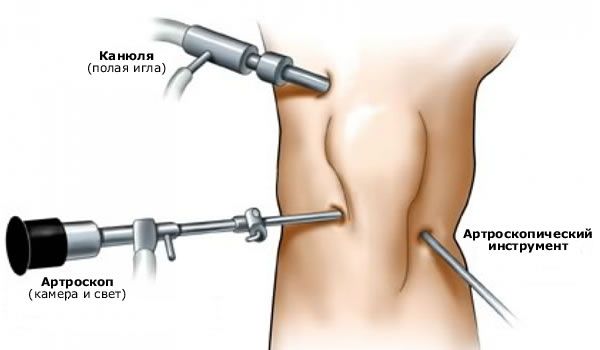
Arthroscopy of the knee joint is a universal method of examination, the results of which are always compared with the data of other studies.
In our opinion, arthroscopy has the greatest value for various intraarticular pathologies: meniscus lesions, articular cartilage, pathological condition of synovial folds, etc.
Of particular relevance arthroscopy acquires in acute trauma, when there is a highly distorted symptomatology and the impossibility of conducting objective testing because of the pain syndrome.
From our point of view, arthroscopic diagnosis is the most valuable method of examination for acute rupture of ligamentous elements of the knee joint.
The earliest detection of cruciate ligament ruptures (in the first two weeks) makes it possible to perform operative stitching of ligamentous elements. In this case, you can hope for a good result of treatment. If more than three weeks have elapsed since the injury, it is not advisable to sew crosswise ligaments, since shortening of collagen fibers occurs and irreversible avascular changes occur.
With diagnostic arthroscopy, produced in the days following the injury, you need to thoroughly wash the joint of the blood, which further prevents the progression of gonarthrosis. In addition, it provides better verification of concomitant intraarticular pathology.
Previously, we attached great importance to partial ruptures of cruciate ligaments, especially PKC. We developed various diagnostic criteria for the detection of this pathology, including arthroscopic signs of partial ruptures. However, later, taking into account the possibilities of process compensation, we came to the conclusion that if the cruciate ligaments are damaged (especially with a partial fracture), it is inappropriate to rely solely on arthroscopic data, since damage to one or another anatomical substrate is not equal to the instability of the knee joint.
That is why at the present time diagnostic arthroscopy is carried out by us immediately before the operative stabilization of the knee joint. Its task is to identify a combined intraarticular pathology, followed by an operative correction.
 [25], [26], [27], [28], [29], [30]
[25], [26], [27], [28], [29], [30]
MRI of the knee
MRI of the knee joint makes it possible to examine both bones and soft tissues, as well as to objectively evaluate all processes occurring in the joint and adjacent tissues. This allows you to identify various pathologies at the earliest stages, for example, with a meniscus rupture or trauma to the ligaments. The MRI method is harmless, has few contraindications (contraindications include pregnancy, excessive body weight, presence of a pacemaker in the body). Magnetic resonance imaging is of great importance in the preoperative study of joints, as well as during rehabilitation. MRI of the knee joint is recommended for meniscus rupture, ligament damage, for various injuries, infectious pathologies, tumors, with puffiness and pain in the joints and periarticular tissues.
PKC is normal with a knee MRI of the knee is a dark band of low intensity signal. From the femoral insertion in the postromedial portion of the outer condyle of the femur, the PKC moves anteriorly downward and medially. The tibial attachment is anterolateral to the tubercles of the intercondylar elevation.
PKC is well visualized on sagittal sections with extensia with external rotation of the tibia 15-20 °. External rotation reduces artifacts and straightens PKS in the sagittal plane.
PKC is brighter than ZKS, which is important, as this can lead to an incorrect diagnosis of PKC rupture.
The macroscopic anatomy of the cruciate ligaments is also different: if the ZKS is represented by parallel fibers, the PKC is twisted. The data indicating the rupture of PKC are as follows: lack of visualization of PKC, lack of continuity of the ligament fibers or abnormal orientation of the remaining fibers.
The complete rupture of PKC is diagnosed more by indirect data: anterior translation of the tibia, excessive posterior slope of the SCS, wavy contour of the PKC with partial or complete rupture.
Diagnosis of ruptures of LAS is much easier. When the leg is unbent, the ZKS has a slight posterior slope in the sagittal plane.
Often near the SCS, a fibrous cord that connects the horn of the external meniscus with the femoral condyle is traced. This is a menisco-femoral ligament (Wrisberg or Humphrey).
Complete fractures of the SCS are well defined in the MRI of the knee joint, or in separation from the bone attachment, or in a defect in the middle of the substance. In the case of partial rupture of SCS, there is an increase in the intensity of its signal, a focal thickening.
If the BCS is damaged, the low-signal intensity of the pole located close to the femoral or tibia is determined.
The thickness of BCS increases with hemorrhage, edema. Usually, BCS gaps are limited by the deep location of the ligament, focal meniscocapsular separations with the joint fluid are visualized, peripheral to the meniscus and limited to a thin band extending deep to the ligament.
A similar picture is represented by damage to the ISS, with the only difference being that the tendon of the popliteal muscle and the structural elements of the arcuat complex are often involved in the process.
Roentgen of the knee joint
On the radiographs of the knee joint, the articular surfaces of the bones forming it are clearly visible. The patella is layered on the distal epiphysis of the femur, the X-ray joint gap is wide, curved in its middle part.
X-ray examination is the most accessible when examining patients with knee ligament injury. X-ray data further influence the treatment plan. Undoubtedly, they are correlated with the results of the clinical examination.
Radiography is performed in two standard projections. In addition, make functional radiographs. When evaluating images, the position of the patella, the tibio-femoral angle, and the thickness of the articular cartilage are taken into account. Assess the relationship and shape of bones: the convexity of the lateral tibial plateau, the concavity of the medial, dorsal arrangement of the fibula in relation to the tibial.

The day of correct evaluation of the relationship between the tibia and the patella, it is advisable to produce lateral radiographs at 45 ° flexion. For an objective evaluation of the tibial rotation, it is necessary to superimpose the lateral and medial condyles of the tibia on each other. Usually the medial femoral condyle is projected more distally than the lateral one. The height of the patella is also assessed.
If necessary, to determine the axis of the limb, additional radiographs are made on long cassettes in a standing position in a direct projection, since there may be significant abnormalities in gonarthrosis.
To obtain additional information on the state of the patello-femoral articulation, axial shots of the patella are made, which allows an analysis of the articular cartilage state on its lateral and medial facet.
To determine the degree of shift of the tibia relative to the femur in the anteroposterior and medial-lateral direction, we previously performed functional radiographs with a load, now this information is provided by ultrasound.
It is extremely important to pay attention to calcification of soft tissues, detachment of bone fragments, ossification of the femoral attachment of BCS. T. Fairbank (1948) described a number of radiologic symptoms observed late in the meniscus removal: the formation of crests and osteophytes along the tibia edge, flattening of the femoral condyles, narrowing of the articular space, which eventually progress.
We noted a number of radiologic signs characteristic of chronic anterior instability of the knee: a decrease in the intercondylar fossa, a narrowing of the joint gap, the presence of peripheral osteophytes on the tibia, the upper and lower pole of the patella, a deepening of the anterior meniscus groove on the lateral condyle of the thigh, hypertrophy and acuity of the intercondylar elevation.
When determining the severity of deforming arthrosis guided by X-ray signs, described by NS. Kosinskaya (1961). There is a direct correlation between the severity of gonarthrosis and the degree of knee instability, as well as the timing of seeking treatment, the number of previously performed surgical interventions for those whose knee joint was injured.

