Vasomotor rhinitis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Vasomotor rhinitis is derived from the name of vegetative nerve fibers that innervate the smooth muscles of the arteries and veins. Vasomotor rhinitis is divided into vasoconstrictor (sympathetic) and vasodilating (parasympathetic) nerve fibers.
IN AND. Voyachek identified vasomotor rhinitis as false rhinitis. In his famous textbook "Basics of otorhinolaryngologists," he wrote that the name "false rhinitis" indicates that the symptom complex of the common cold may not be accompanied by pathological signs of inflammation of the nasal mucosa. For the most part, this is a symptom of general vegetative neurosis, and therefore is often only a link in a number of relevant disorders, such as asthma. Thus, in pure form - vasomotor rhinitis is functional. Subspecies of this group are allergic conditions, when vasomotor and secretory disorders of the nasal cavity occur under the influence of an allergen.
This definition, expressed more than half a century ago, remains relevant today, when the problem of chronic vasomotor (neuro-vegetative) and allergic rhinitis has been studied from many sides of medical and biological science (immunology, allergology, neuro-vegetative neurosis, etc.). According to some authors, it is the latter that play the most important role in the pathogenesis of true vasomotor rhinitis, which are not accompanied by any inflammatory reactions in the classical manifestation.
It is important, however, to emphasize that it is the nasal vegetative-vascular dysfunctions provoked by endo-or exoallergens that may be complicated by inflammatory processes; in these cases, it is the primary allergy that is the main etiological factor in the occurrence of vasomotor rhinitis. In this regard, it should be recognized that the modern division of vasomotor rhinitis into neurovegetative and allergic forms is largely arbitrary and is mainly didactic in nature. Apparently, these are two sides of the same pathological condition.
In its “pure form,” the neurovegetative form of vasomotor rhinitis can be observed with any irritative processes in the nasal cavity, for example, caused by the contact spike of the nasal septum, which irritates the perivasal nerve vegetative endings of the lower nasal ravines. However, this mechanism may further provoke the transition of the neurovegetative form to the allergic one. It is also possible that the nasal manifestations of the neurovegetative form of vasomotor rhinitis are a consequence of general vegetative neurosis; in this case, we can observe other manifestations of this neurosis, such as signs of neurocirculatory dystonia, hypotonic disease, angina pectoris, etc.
In the genesis of the neurovegetative form of vasomotor rhinitis, pathological conditions of the cervical spine, which are manifested by the alteration of the cervical sympathetic nodes, may play a large role. Thus, in the etiology and pathogenesis of vasomotor rhinitis, there is a whole complex of systemic pathological conditions in which the common cold is only the “tip of the iceberg” of a deeper and more common disease. An important role in the occurrence of vasomotor rhinitis can play provoking factors, which should include occupational hazards, smoking, alcoholism, drug addiction. On the other hand, primary vasomotor and allergic rhinitis can play the role of peculiar triggers (triggers), giving rise to more common and serious neurovascular diseases, such as migraine, perivascular neuralgia, diencephalic syndrome, etc.
Causes and pathogenesis of vasomotor rhinitis
Causes and pathogenesis of vasomotor rhinitis: an allergic form of vasomotor rhinitis is divided into seasonal (periodic) and persistent (year-round) rhinitis.
Seasonal runny nose is one of the pollinosis syndromes (pollen allergy, pollen fever), characterized mainly by inflammation of the respiratory tract mucosa and eyes. With a hereditary predisposition to pollinosis, pollen causes sensitization of the body, i.e., the production of antibodies to the pollen allergen, resulting in an exposure of the antigen to an antibody, which manifests signs of inflammation when the latter hits the mucous membrane. Pathognomous manifestations of seasonal rhinitis are seasonal bouts of acute rhinitis and conjunctivitis. In severe cases, they are joined by bronchial asthma. Pollen intoxication is also possible: fatigue, irritability, insomnia, and sometimes a rise in body temperature. In the presence of chronic foci of infection during hay fever, they can contribute to the development of acute sinusitis. Rare manifestations include diseases of the nervous system (arachnoiditis, encephalitis, damage to the visual and auditory nerves, the development of attacks of Meniere's disease).
Symptoms Typically, an attack of rhinopathy occurs acutely, among full health, in late May and June, during the flowering of trees and herbs, characterized by the appearance of severe itching in the nose, uncontrolled repeated sneezing, abundant watery discharge from the nose, difficulty in nasal breathing. At the same time there are signs of conjunctivitis. The onset of seasonal rhinitis usually lasts 2-3 hours and can be repeated several times a day. The most common external factors can provoke vasomotor rhinitis here: exposure to the sun or a draft, local or general cooling, etc. It has been observed that the state of psychological stress reduces the severity or breaks off the attack of pollinosis.
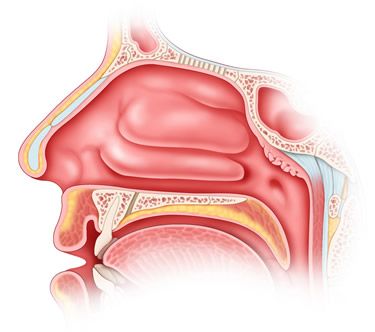
When anterior rhinoscopy does not reveal any pathological changes in the nasal mucosa during the interictal period, deformities of the nasal septum, contact spikes, and in some cases single mucous polyps may occur. During the crisis, the mucous membrane becomes sharply hyperemic or bluish, edematous, nasal conchs are enlarged and completely obtuse the nasal passages, in which abundant mucous discharges are observed. The vessels of the nasal concha react sharply with contraction to adrenaline lubrication. In some patients, attacks of seasonal runny nose may be accompanied by symptoms of irritation of the mucous membrane of the larynx and trachea (cough, hoarseness, and a viscous, clear sputum), as well as asthmatic syndrome.
Persistent allergic rhinitis is one of the syndromes of the allergic condition of the body, manifested by various forms of allergy. The signs and clinical course similar to hay fever. The main distinguishing feature of persistent allergic rhinitis is the lack of frequency, more or less constant flow, moderate severity of attacks. Allergens in this form of allergic rhinitis, unlike seasonal, can be a variety of substances with antigenic and haptenic properties that act permanently on humans and cause sensitization of the body to themselves with the formation of antibodies. These substances, in contact with tissue antibodies, cause the same “antigen - antibody” reaction as in the case of seasonal rhinitis, during which biologically active mediators (including histamine and histamine-like substances) are released, irritating receptors of the nasal mucosa, causing vasodilation and activating the activity of the mucous glands.
Symptoms of vasomotor rhinitis
Symptoms of vasomotor rhinitis are characterized by recurrent or constant nasal congestion, often intermittent, with occasional watery discharge from the nose, at the height of the attack - itching in the nose, sneezing, pressure sensation in the nose, headache. During the day, an attack (V.I. Voyachek called this attack an “explosion” of a vasomotor reaction) sneezing and rhinorrhea, as a rule, occurs suddenly and just as suddenly passes, can be repeated up to ten times a day and more often. At night, nasal congestion becomes constant due to the night cycle of the parasympathetic nervous system function enhancement.
Characterized by the congestion of that half of the nose, on the side of which lies the patient, and the gradual disappearance of it on the opposite side. This phenomenon testifies to the weakness of vasoconstrictors. According to VF Undritsa, KA Drennovoy (1956) and others, the long-term functional stage of the neurovegetative form of vasomotor rhinitis leads to the development of an organic stage (proliferation of interstitial tissue and the occurrence of hypertrophic rhinitis), which is largely due to the excessive use of decongestants. Vasoconstrictor fibers belong to the adrenergic nerves, since the transmission of excitation to the vessels causes the release of norepinelia in the synapses. These fibers for ENT organs come from the upper cervical sympathetic node. Parasympathetic vasodilator fibers are concentrated in the glossopharyngeal, facial, trigeminal nerve and pterygopalatomy.
In anterior rhinoscopy, enlarged inferior nasal conchae have a characteristic color, which V.I. Voyachek defined as “gray and white spots”. The inferior nasal concha feels soft with a bellied probe, the probe penetrates easily without damaging the mucous membrane in the thickness of the shell. A pathognomonic sign is a sharp reduction of the concha when lubricating them with adrenaline. The sense of smell is disturbed depending on the degree of difficulty of nasal breathing.
Allergic form of vasomotor rhinitis
Allergic diseases have been known since ancient times. Hippocrates (V-IV century. BC. E.) Described cases of intolerance to some nutrients; K.Galen (II in. Ne) reported a cold, arising from the smell of roses, in the XIX century. Hay fever was described and proved to be the cause of inhalation of plant pollen. The term "allergy" was proposed by the Austrian pediatrician C.Pirquet in 1906 to refer to an unusual, altered reaction of some children to their administration for the treatment of diphtheria serum. Substances that cause atypical (allergic) reactions were called allergens. Such substances include, for example, plant pollen, which causes seasonal diseases called pollinosis. Allergens are divided into exogenous (chemicals, food, various plants, protein compounds, microorganisms, etc.) and endogenous, which are metabolic products of an allergenic organism, resulting from a metabolic disorder, the occurrence of certain diseases that grow in the body microbial associations. The source of allergies can also be chronic foci of infection, serums and vaccines, numerous medications, household and epidermal allergens, etc. A particular group of allergens consists of physical factors - heat, cold, mechanical stress, which cause specific substances in the sensitive organism. With allergenic properties.
When an allergen is introduced into the body, an allergic reaction develops, which, depending on its nature, can be specific and nonspecific. The specific reaction goes through three stages - immunological, the stage of formation of mediators and the stage of pathophysiological, or clinical manifestations. Non-specific allergic reactions (pseudo-allergic, non-immunological) occur during the first contact with an allergen without prior sensitization. They are characterized by only the second and third stages of an allergic reaction. Allergic rhinitis can occur both in specific and non-specific type of reaction and mainly refers to allergic reactions of the first type, which also include anaphylactic shock, urticaria, atopic asthma, pollinosis, Quincke edema, etc.
Neurovegetative form of vasomotor rhinitis
As a rule, seasonality is not typical for this form of vasomotor rhinitis. Vasomotor rhinitis is equally common at all times of the year and depends mainly on either external triggering factors (dustiness of the rooms, aggressive fumes in the inhaled air, the presence of contact curvatures of the nasal septum), or the general neurovegetative dysfunction mentioned earlier. Usually, in the latter case, patients are patients not only of the rhinologist, but also of the neurologist.
What's bothering you?
Diagnosis of vasomotor rhinitis
Diagnosis of vasomotor rhinitis: pathological changes and the clinical course of persistent allergic rhinitis can be divided into four stages:
- stage of transient aperiodic seizures;
- stage type continue;
- polypopulation stage;
- stage of carnification.
The first stage is characterized by a more or less permanent moderately pronounced runny nose with periodic crises. Patients with this form of rhinitis show high sensitivity to the cold factor, reacting to the slightest cooling of the hands, feet, or the whole body, as well as drafts by the exacerbation of the pathological process. Patients complain of constant, intermittently increased nasal congestion, decrease or absence of smell, poor sleep, dry mouth, headaches, increased physical and mental fatigue, as well as periodically occurring attacks of expiratory dyspnea. At this stage, the initial phenomena of disturbance of cell membrane permeability occur.
At the anterior and posterior rhinoscopy at this stage of the disease, the same changes are observed as during an attack of seasonal rhinitis, and decongestants are active with respect to the vessels of the nasal cavity.
However, with a longer course of persistent allergic rhinitis, its second stage occurs, which manifests itself in the initial signs of degeneration of the nasal mucosa. It becomes pale, acquires a grayish tint, covered with granular formations, especially noticeable in the area of the front ends of the middle and lower turbinates and the posterior end of the lower turbinates. At this stage, the difficulty of nasal breathing becomes more or less constant, the effect of vasoconstrictor drugs is reduced to a minimum, the sense of smell is practically absent, and complaints of a general nature are intensified.
After some time, calculated from a period of several months to 1-4 years, mucous polyps appear on average in the middle of the nasal course (the stage of polyporosis or polypous rhinitis) in the form of translucent bag-like formations hanging down the leg into the lumen of the common nasal passage. Most often they look flattened, sandwiched between the lateral wall of the nose and its septum. Older polyps are usually covered with a thin vascular network and germinate connective tissue.
At the same time, the stage of carnification comes: the tissues of the middle and especially the lower turbinate become denser, stop responding to the vasoconstrictor preparations and acquire all the signs of hypertrophic rhinitis. The third and fourth stages are characterized by constant nasal congestion, mechanical and sensory anosmia, and an increase in the general symptoms of the disease.
Common symptoms of the disease (fatigue, insomnia, frequent colds, sensitivity to cooling, etc.) become permanent. At the polyproductive stage, attacks of bronchial asthma intensify and increase. The temporal ratio of bronchial asthma and the stage of polyproduction is different. Often, as the primary lesion occurs, it is the stage of polyproduction, t. C. Allergic rhinitis syndrome. If the basis of allergy is non-infectious genesis, then they talk about atopic bronchial asthma. It should also be noted that similar pathological processes in allergic rhinitis develop in the paranasal sinuses and most often in the maxillary, from which polyps prolabiruyut through her fistula into the middle nasal passage.
Treatment of allergic rhinitis involves the use of anti-allergic, desensitizing, antihistamine, vasoconstrictor, local anesthetic and general sedatives. This list of drugs is recommended by the international community of rhinologists in the form of the so-called 1996 consensus. However, despite these recommendations and the numerous original proposals of various authors, the treatment of patients suffering from allergic rhinitis remains difficult and not fully resolved. The most effective method is the identification and elimination of allergen causing vasomotor rhinitis, but with polyallergy and this method becomes ineffective, especially since this form of allergic rhinitis can follow the type of so-called creeping allergy, when previously indifferent substances under the influence of sensitizing effects of allergens themselves become cause appropriate, sometimes hyperergic reactions.
What do need to examine?
What tests are needed?
Who to contact?
Treatment of vasomotor rhinitis
Treatment of vasomotor rhinitis is mainly symptomatic, directed either to the use of sympathomimetic drugs that have a vasoconstrictor effect (sanorin, naphthyzin, ephedrine, etc.). New generation drugs include dosage forms whose active ingredients are substances that have sympathomimetic properties, for example, oxymetazoline (nazivin, nazol), tetrahydrozolin hydrochloride (tezin), xylometazoline hydrochloride (xylometazoline, xymelin), etc. All listed drops from rhinitis have a adrenomimeticheskim action, narrowing peripheral vessels, reduce swelling of the nasal mucosa, hyperemia and exudation. They are indicated for acute neurovegetative and allergic rhinopathy, hay fever, sinusitis and their tubular and otiatric complications. Apply them in the form of drops and aerosols. Methods of use and doses are indicated in the relevant annotations.
Symptomatic treatment of vasomotor rhinitis
Symptomatic treatment should also include various surgical interventions, such as mechanical and ultrasound submucosa destruction of the vascular plexuses of the inferior nasal concha for subsequent scarring, electroplating of the inferior nasal concha, the use of cauterizing silver nitrate salts, etc.
Elements of pathogenetic treatment of vasomotor rhinitis contain various physiotherapeutic methods, both local and at a distance, aimed at normalizing the interaction of sympathetic and parasympathetic calving of the ANS, improving microcirculation, enzymatic activity, enhancing the oxidation of biosubstrates, normalizing the function of cell membranes, etc. For example local methods include the use of low-energy laser radiation, constant magnetic fields, etc. According to the method of A.F. Mamedov (19 91), the combined effect of these factors is used, in which the permanent magnetic field is directed outside to the slope of the nose, and the inside is irradiated with the help of a laser fiber reflexogenic zones of the front ends of the middle and lower turbinates. At a distance, laser irradiation of the projection zone of the pterygine node, various physiotherapeutic effects on the neck area, etc. Are used.
In the treatment of the neurovegetative form of vasomotor rhinitis, the directional study of the general neurovegetative status for the identification of possible general neurological disorders and neurotic conditions is important. Assess living and working conditions, the presence of bad habits, chronic foci of infection and diseases of internal organs.
All treatments for allergic rhinitis are divided into local and general, symptomatic and pathogenetic. If an allergen is found and the corresponding anti-antigen serum has been developed for it, then they speak about etiotropic or immunological treatment. Currently, there are a huge number of different medicines used for allergies, and in particular for allergic rhinitis, details of which are listed in the Register of medicines.
Topical treatment of vasomotor rhinitis
Topical treatment is mainly symptomatic and only partly pathogenetic, aimed at blocking allergic reactions of a local nature, i.e., nasal syndrome of general allergy. Preparations for local use are used in the form of nasal sprays, less often in the form of drops or powders blown into the nasal cavity. As drugs for local use drugs prepared on the basis of azelastine hydrochloride (Allergodil), levocabastin, etc.
Allergodil released in the form of a nasal spray and eye drops. Levocabastip is used in the form of endoasal and eye drops. Both drugs have anti-allergic and antihistamine properties, selectively blocking H1-receptors. After intranasal administration, it quickly eliminates the symptoms of allergic rhinitis (itching in the nasal cavity, sneezing, rhinorrhea) and improves nasal breathing by reducing the swelling of the nasal mucosa. When applied to the conjunctiva reduces the manifestations of allergic conjunctivitis (itching, tearing, redness and swelling of the eyelids, schmosis). In addition to antihistamines, in case of allergic rhinitis, local application of alpha-blockers (naphthyzin, sanorin, galazolin), as well as new drugs of similar action (Dr. Theiss nasal spray, tezin, xymein, etc.) is possible.
Each drug used in allergic and any other diseases is characterized by such concepts as contraindications, use during pregnancy and feeding, side effects, overdose, precautionary measures, special instructions, compatibility with other drugs, etc., which are described in detail in their respective manuals., reference books and annotations. Before using any drug, this information should be carefully studied.
Allergodil spray: for adults and children over 6 years old by one injection in each half of the nose 2 times a day. Eye drops for adults and children over 4 years old one drop in the morning and evening until the symptoms of the disease disappear.
Levocabastin: intranasally for adults and children over 6 years old - 2 inhalations in each nasal passage 2 times a day (maximum 4 times a day). Treatment continues until symptoms disappear.
Dr. Theiss nose spray nasal spray: the basis of the spray is kenlometazoline, which has a vasoconstrictor and anti-congestive effect. The drug is injected into both halves of the nose during inhalation using a special sprayer, one injection in each half of the nose 3-4 times a day for 2 nsd.
Nazivin (Oksimstazolin) produced in the form of drops and spray. Nasal drops: for adults and children over 6 years old, 1-2 drops in each half of the nose 2-3 times a day 0.05% solution; children from 1 year to 6 years - 0.025%, up to 1 year - 0.01% solution. Spray nasal and nasal spray dosed 0.5%: for adults and children over 6 years of age - one injection 2-3 times a day for 3-5 days.
Tizin (tetrahydrozoline hydrochloride) - sympathomimetic amine. Drops, aerosol, gel for intranasal use (0.05-0.1%). Adults and children over 6 years old - 2-4 drops in each nostril no more than every 3 hours. It also has a sedative property, it is applicable in pediatrics.
Xymelin (kenlometazolin) stimulates alpha-adrenoreceptors, has a fast and long-lasting vasoconstrictor and anti-congestive effect. Adults and children over 6 years old - 2-3 drops of a 1% solution, or one injection from a nebulizer into each half of the nose 4 times a day. Breast and children up to 6 years old - 1-2 drops of a 0.5% solution in each nostril 1-2 (no more than 3) times a day. Nasal gel only for adults and children over 7 years old - 3-4 times a day; lay a small amount in each half of the nose as deeply as possible on the cobblestones for how many minutes so that the cotton wool stick can be easily removed.
To the local treatment of allergic rhinitis should be selectively add drugs listed in the section on the treatment of neurovegetative form of vasomotor rhinitis.
Pathogenetic treatment of vasomotor rhinitis
General treatment should be recognized as pathogenetic, and in cases where immunological methods are used - and etiotropic. As A.S. Kiselev (2000) notes, specific immunotherapy is very effective, but its difficulties lie in the laboratory isolation of the active allergen (antigen), especially in polyallergy. In addition, the use of specific antiallergic sera can cause hyperergic reactions such as anaphylaxis and exacerbation of atopic asthma, so immunotherapy is not widespread either in our country or abroad. The use of general (oral) treatment is based on the assumption that atopic rhinitis (seasonal, year-round) is a local manifestation of a common allergic disease, therefore the use of drugs with appropriate pharmacological properties that act on the body as a whole is an obligatory method of treatment not only rhinogenic manifestations allergies, but also its manifestations in other organs and systems. The most common method of using antiallergic drugs of general effect is oral. All of them have almost a very similar pharmacological effect.
Of the antihistamines that have found widespread use in the past century and have not lost their relevance in our time, you should specify such as diphenhydramine, diazolin, suprastin, tavegil, the main pharmacodynamic effect of which is the replacement of endogenous histamine (source of allergic reactions) in histamine receptors of blood vessels and blocking the pathogenic properties of histamine in these receptors. Currently, there are many new-generation drugs that have a more effective effect and are devoid of the side effects typical of previous-generation drugs. New generation drugs selectively block H1-histamine receptors, prevent hisagumin from acting on vascular smooth muscle, reduce capillary permeability, inhibit exudation and excretory function of the glands, reduce itching, capillary stasis, erythema, prevent development and alleviate the course of allergic diseases.
Oral drugs for the treatment of vasomotor rhinitis
Astemizol. Indications: allergic seasonal and year-round rhinitis, allergic conjunctivitis, allergic skin reactions, angioedema, bronchial asthma, etc. How to use and dosage: per os on an empty stomach 1 time per day; adults and children over 12 years old - 10 mg, children aged 6-12 years - 5 mg in the form of tablets or suspensions, up to 6 years - 2 mg per 10 kg of body weight only as a suspension. The maximum duration of treatment is 10 days.
Loratadine. The indications are the same as for astemizole; In addition, it is indicated in allergic reactions to insect bites and in pseudo-allergic reactions to histaminole-librators. Dosage and administration: per os before meals. Adults and children (over 12 years old or with a mass of more than 30 kg) - 10 mg (1 tablet or 1 teaspoon of syrup) 1 time per day.
Other drugs of a similar action: histalong, dimeboi, clarisens, clariaise, claritin, desloratadine, cystine, ebastine, astafen, ketotif, ketotifen, pseudoephedrine, and more. Others
Steroid drugs. General steroid therapy for allergic rhinitis is used extremely rarely, only in cases complicated by attacks of atopic bronchial asthma, and is the prerogative of the pulmonologist, and for anaphylactic shock - the resuscitator. However, topical application of koritkoteroidov in combination with antihistamine therapy significantly increases the effectiveness of the treatment of allergic rhinitis, especially in its severe clinical forms. In the last century, various ointments and emulsions containing steroid components became widespread. Currently used more modern composite drugs that do not have side effects inherent in steroids used in pure form. Such drugs include baconase (beclomethasone dipropionate), syntaris (flunisolide), flicsonase (fluticasone permeate), etc.
Baconase - dosed aerosol glucocorticoid drug for intranasal use. 1 dose contains 50 µg of active substance beclomethasone dipropionate. The drug has a pronounced anti-inflammatory and anti-allergic properties, eliminates swelling, hyperemia. It is used for the prevention and treatment of seasonal and year-round allergic rhinitis. Apply only intranasally two inhalations in each nostril <2 times a day. The maximum daily dose is 8 inhalations per day.
Sintaris - dosed aerosol (active substance fluzinolide) of a glucocorticoid preparation for intranasal use, is available in glass bottles of 20 ml (200 doses), equipped with a dispensing spray device. It has a decongestant, antiexudative, antiallergic effect. It is indicated for seasonal and year-round rhinitis, including hay fever. Adults appoint 2 injections in each nostril 2 times a day. During the period of exacerbation or with severe disease - 2 injections in both halves of the nose 3 times a day. Children one spray (25 mcg) 1 time per day. The maximum dose: adults - 6, children 3 sprays per day.
Similar nasal sprays (fliksonaze and fliksotid) on an active basis fluticasone give the same therapeutic effect as mentioned; have a minimal systemic effect.
At present, composite preparations containing substances of antihistamine and alpha-adrenomimetic action, such as clarinase and rhinopront, are becoming common.
Clarinese-12 (composition - tablets containing 5 mg of loratadine and 120 mg of pseudoephedrine). Possess antiallergic and vasoconstrictor properties; they block H1 receptors, have decongesting properties (pseudoephedrine sulfate), reduce the edema of the mucous membrane of the upper respiratory tract of the VDP, improve their permeability and facilitate respiration. Apply per os, regardless of the meal, without chewing, drink a glass of water. Adults and children aged 12 years and older - 1 tablet 1-2 times a day.
Rinopront. The active substances are carbinoxamine maleate and phenylephrine hydrochloride, which have antihistamine and antiallergic effects. Carbinoxamine reduces the value of capillaries of the nasal mucosa, phenylephrine has a sympathomimetic effect, causes vasoconstriction and reduces swelling of the mucous membrane. Within 10-12 h eliminates the phenomenon of acute rhinitis, burning and itching in the eyes, feeling of heaviness in the head. This dosage form is used for acute cold of various origins (vasomotor, allergic, infectious and inflammatory, with hay fever).
Adults and children over 12 years old are prescribed 1 capsule 2 times a day with an interval of 12 hours. If it is difficult to swallow, 1 tablespoon of syrup is prescribed 2 times a day. Children from 1 year to 6 years - but 1 teaspoon of syrup 2 times a day, from 6 to 12 years - 2 teaspoons 2 times a day.
Local steroid therapy gives effect in combination with antihistamines and alpha-blockers. As a rule, corticosteroids used for topical administration are included in the composition of composite dosage forms made according to special prescriptions or used in monoform.
Of the last generation of drugs should be noted rinocort, the active basis of which is a semisynthetic corticosteroid budesonide.
Rinocort - glucocorticoid drug for inhalation; Available in aerosol. It has a local anti-inflammatory effect, almost without causing a systemic effect. It is indicated for seasonal and year-round allergic rhinitis, as well as for the prevention of pollinosis and recurrence of polyps after polypotomy. The initial dose is 2 injections (100 μg) in each nostril in the morning and evening. When a therapeutic effect is achieved, the dose may be reduced.
More information of the treatment


 [
[