Bile stasis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Among gastrointestinal pathologies, gastroenterologists distinguish bile stagnation, which is a syndrome that indicates a malfunction in the hepatobiliary system: bile, gallbladder (bile depot where it becomes more concentrated) or biliary transport network (intra- and extrahepatic bile ducts).
What is the risk of stagnation of bile?
This pathology is diagnosed more often, so you should know what is dangerous stagnant bile for the body. After eating, the fats contained in it begin to emulsify, but lipids can be digested and lipophilic vitamins can be fully absorbed, in addition to gastric juice and pancreatic enzymes, bile acids and their salts, the main constituents of bile, are needed. From the gall bladder they enter the duodenum, where the process of emulsification and colloidal hydrolysis of fats continues.
If the bile stagnates (i.e., does not enter the intestinal tract of the digestive tract), the activity of the intestinal enzyme of the lipase decreases, and the fats are not completely cleaved and enter a significant amount in the blood, making it difficult to convert glucose into glycogen (which is fraught with the development of diabetes mellitus). Bile stasis is dangerous by reducing the removal of excess cholesterol, which is found in the bile itself: it causes hypercholesterolemia (high cholesterol in the blood) and accelerates the development of atherosclerosis.
Stagnation of bile in the gallbladder often leads to its inflammation (secondary cholecystitis) or cholelithiasis (cholelithiasis). It is in the presence of stones in the gallbladder that acute and chronic cholecystitis develops with congestion of bile.
You can simultaneously diagnose gastritis and bile stasis when the mucous membrane of the esophagus and stomach are exposed to the bile acids that get there by "reverse" from the duodenum - with chronic duodenogastric reflux (arising from the weakness of the cardiac esophagus sphincter).
To the so-called sclerosing cholangitis - inflammation, fibrosis and strictures of the bile ducts - can lead to stagnation of bile in the ducts.
If the circulation of bile acids in the digestive tract is impaired, the absorption of fats (fat malabsorption) and fat-soluble vitamins: retinol (vitamin A), ergocalciferol (vitamin D), tocopherol (vitamin E), and phylloquinones (vitamins of group K) decreases. The most well-known consequences and complications of vitamin A deficiency are a deterioration of twilight vision, and vitamin D - osteomalacia (when a decrease in the mineralization of bones leads to their softening). At the same time, a simultaneous deficiency of vitamins A and D interferes with the absorption of calcium, which makes bone tissue even less dense, that is, osteoporosis develops. A lack of vitamin K threatens to reduce blood clotting and the emergence of hemorrhagic diathesis and bleeding.
A very real threat that chronic bile congestion conceals is an increase in the acidity of the intestine, because bile - due to the presence of calcium cations in it - reduces the acidity of the gastric contents of the stomach, which passes into the intestinal stage of digestion. With congestion of bile (cholestasis) there is an acid-alkaline imbalance of the gastrointestinal tract, and the result of acidification becomes ascites (hydrocephalus) and poor bowel function due to the multiplication of pathogenic microbes.
When there is a prolonged stagnation of bile in the liver, an increase in the level of cyanodeoxycholic bile acid produced in the liver can lead to the death of hepatocytes and focal necrosis of the parenchyma. This is a very serious complication, since the liver is responsible for very important functions.
If there is stagnation of bile in the intestine, the toxicity of conjugated metabolic products and exogenous toxins (including bacterial origin) is increased. Also, the consequences and complications concern the synthesis of hormones, which is significantly reduced, since lipids are needed for their production.
Epidemiology
According to research, up to 70% of cases are due to extrahepatic bile stasis. Among women, this syndrome occurs more often - especially during pregnancy. Due to immaturity of the liver enzyme system, newborns and children of the first two or three years of life are more prone to stagnation of bile.
Causes of the stagnation of bile
In clinical gastroenterology, the causes of congestion of bile are associated with the destruction of hepatocytes due to primary biliary or alcoholic cirrhosis of the liver (hepatocellular stasis); with liver damage by infections or parasites (viral hepatitis A, C, G, hepatic form of tuberculosis, amebiasis, opisthorchiasis, giardiasis, etc.); with the effect on the liver of various toxins or components of medications (including sulfonamides, penicillin antibiotics, analgesics, hormones).
As experts note, stagnation of bile in the liver occurs if there is a cyst of the liver, malignant neoplasms or metastases.
Among the reasons for stagnation of bile in the gallbladder and bile ducts are:
- dyskinesia of the gallbladder;
- stones in the gallbladder;
- inflection of the gallbladder;
- tumors of the gallbladder or bile ducts;
- inflammation in the neck of the gallbladder;
- cystic formations of the common bile duct or its compression by a cyst, localized in the pancreas;
- compression and narrowing of the initial section of the common hepatic duct (Mirizzi syndrome);
- violation of the functions of the valve system of the biliary tract (sphincters of Oddi, Lutkens, Mirizzi, Geister);
- failures of the endocrine and paracrine mechanisms of gastroduodenal digestion, associated with the imbalance of secretin, cholecystokinin, neurotensin and other intestinal hormones.
Risk factors
Closely linked hypodynamia and stagnation of bile: the less a person moves, the slower the metabolic processes in his body and the higher his risk of dyskinesia biliary ducts or the formation of gallstones.
A stagnation of bile after removal of the gallbladder is called a part of typical postoperative consequences, which arise due to the formation of scar tissue, narrowing the lumen of the bile duct.
An important food risk factor for biliary obstruction due to stones in the gallbladder can be excessive consumption of sugar, as well as fat-containing products that cause bile stagnation.
Also, the real risk factors for bile stagnation are alcohol abuse, overeating, obesity, inherited genetic predisposition to metabolic disorders.
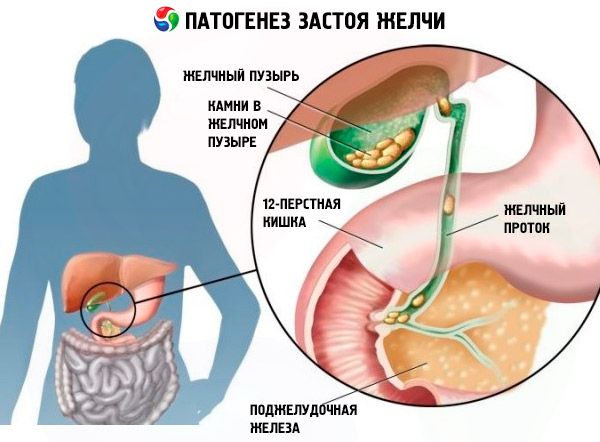
Pathogenesis
The pathogenesis of bile stasis in the intrahepatic ducts is associated with infections, endocrine disorders, genetic disorders of metabolism (thyrotoxicosis, amyloidosis of the liver or intestines) and iatrogenic effects. And the pathogenesis of bile stasis in the extrahepatic ducts (vesicle, general hepatic and common bile duct) is caused by changes in the composition of bile and an increase in its lithogenicity, bile duct anomalies and partial or complete obturation.
 [12]
[12]
Symptoms of the stagnation of bile
First of all, it should be understood that this condition can be asymptomatic. And the intensity and consistency in which the symptoms of stagnation of bile manifest themselves depend on the specific cause and individual characteristics of the hepatobiliary system of the body. But the first signs are itchy skin and changes in stool and urine. It is believed that dermal itching with bile congestion is a reaction to an increase in the level of bile acids in the blood plasma, where they get as a result of damage to the liver cells by chenodeoxycholic acid.
Feces with stagnation of bile have a characteristic discoloration due to a violation of elimination of the bile pigment of bilirubin (which normally oxidizes into sterocilin, staining the feces to brown, and urine to straw-yellow). Urine with bile stagnation, on the contrary, becomes dark, because it increases the level of urobilin (urine stericilin).
Constipation and diarrhea with bile congestion are typical symptoms of this condition. Since bile acids play an important role in intestinal motility, their reduction in the lumen of the intestine leads to constipation. A diarrhea during stasis is associated either with an increased content of unsorted fats in stool mass (steatoria), or with changes in the intestinal microflora.
Changes in color of the skin - icterus - are not observed in all patients, but at sufficiently high plasma levels of conjugated bilirubin, skin, sclera, mucous membranes become yellow. On the eyelids, spots of yellow color (xantelism) may appear, and focal skin lesions with inclusions of cholesterol (xanthomas) appear around the eyes, palmar folds, under the breast, on the neck and in the diaper area.
Characteristic pain in stasis bile - blunt paroxysmal, localized in the right upper quadrant of the abdomen (in the hypochondrium region); can give up and back (in the collarbone, shoulder or shoulder blade); possible acute attacks in the form of colic.
Heartburn with bile congestion is often accompanied by a constant sense of bitterness in the mouth, and dry mouth is also characteristic of bile stasis. Bile helps to break down the food proteins and nitrogenous bases in the food, and the smell from the mouth due to stagnation of bile arises because of deterioration of digestion and absorption of proteins. By the way, a bitter eructation of bile often manifests itself and stagnation of bile after removal of the gallbladder.
Fever - the temperature at bile congestion - evidence of infection, for example, phlegmonous or gangrenous cholecystitis with cholelithiasis. High temperature can give sepsis, which develops after carrying out endoscopic diagnostic manipulations.
In addition, bile congestion symptoms include nausea and vomiting; dizziness and a feeling of general weakness; enlargement of the liver (hepatomegaly); increased pressure in the system leading to the liver portal vein. With bile stasis in children, the lack of essential polyunsaturated fatty acids (linoleic, linolenic, arachidonic) can lead to growth retardation, damage to the peripheral nervous system, and dermatitis. Alopecia, that is, hair loss with bile stasis, is also the result of a deficiency of triglycerides.
Bile stasis during pregnancy
Clinical studies in recent years have shown that bile stasis during pregnancy is initiated by estrogens, which regulate most of the processes in the body of a future mother. So, pregnant women produce large hormones secretin, and, hence, more bile. But at the same time, the secretion of growth hormone growth hormone (STH) increases, and it blocks the hormone cholecystokinin, responsible for contraction of the gallbladder and common bile duct.
Bile stasis during pregnancy (idiopathic jaundice of pregnancy or obstetric cholestasis) is most often manifested by painful skin itching (especially the palms of the hands and soles of the feet) to the middle of the second or third trimester - as far as the maximum level of estrogen reaches. In addition, there was a significant increase in serum levels of aminotransferase, alkaline phosphatase, and unconjugated bile acids; other symptoms appear rarely. Within two to three weeks after delivery, spontaneous relief and disappearance of all symptoms occurs.
The epidemiology of bile stasis in pregnant women shows a 0.4-1% susceptibility to the condition of women in most areas of Central and Western Europe and North America, while in the Scandinavian and Baltic countries this indicator reaches 1-2%, and in some regions of Latin America - up to 5-15%.
At the same time, such consequences and complications of bile stasis in pregnant women are noted: premature birth (20-60%), meconium staining in amniotic fluid (more than 25%), fetal bradycardia (14%), fetal distress (22-40%), fetal loss (0.4-4%).
Bile stasis in 45-70% of women is and in all subsequent pregnancies.
By the way, with itching and lack of jaundice, stagnation of bile and allergy are often not differentiated, and the patients turn to dermatologists who can not help them in any way.
Bile stasis in a child
There are many reasons that cause stasis of bile in a child, in particular:
- absence of gallbladder (agenesis);
- doubling of the gallbladder (complete or rudimentary);
- deepening of the gallbladder to the parenchyma of the liver;
- diverticulum (protrusion of part of the wall) of the gallbladder;
- congenital bile duct dilatation inside the liver (Caroli syndrome);
- congenital strictures in the presence of a cyst of the common bile duct;
- a fairly common congenital (due to mutations of the gene of serine digestive enzymes), a violation of the synthesis of hepatic alpha-1-antitrypsin;
- genetically determined decrease or total absence of intrahepatic ducts (biliary atresia);
- heterogeneous bile formation disorder - progressive family intrahepatic congestion (Byler's disease); pathogenesis is associated with mutations in the genes of the hepatocellular transport system; is diagnosed in one newborn from 50-90 thousand.
Read also - Congenital malformations of the biliary tract
In addition, the stagnation of bile in a child of preschool and school age can have the same reasons as in adults (see above). But most often the etiology is associated with a violation of gallbladder motility and functional disorders of the biliary tract.
Where does it hurt?
Diagnostics of the stagnation of bile
In clinical practice, the diagnosis of stagnation of bile is carried out by examination, during which, in addition to collecting anamnesis and examining the patient, such tests are taken as:
- general blood analysis;
- biochemical blood test for bilirubin, cholesterol, bile acids, 5-nucleotidase, aminotransferases, as well as hepatic enzymes - alkaline phosphatase, leucine aminopeptidase (LAP) and gamma-glutamyl transpeptidase (GGTP);
- a blood test for antibodies to parasites;
- urine analysis for urobilin;
- analysis of stool for parasitic infestations.
Instrumental diagnosis of pathologies in bile congestion is carried out using:
- ultrasound (ultrasound) of the gallbladder, liver and small intestine;
- dynamic cholescintigraphy;
- esophagogastroduodenoscopy;
- radioisotope hepatobiliary scintigraphy;
- endoscopic cholangiography;
- endoscopic retrograde radiography of the bile duct and pancreas (ERCPG).
- CT or MRI of the digestive organs.
What do need to examine?
What tests are needed?
Differential diagnosis
The problem solved by differential diagnostics consists in a clear delineation of the problems of the hepatobiliary system that caused bile stasis from hereditary defects of bile excretion (Rotor, Dubin-Johnson syndromes), unconjugated hyperbilirubinemia (Gilbert's syndrome), parenchymal jaundice, hematuria, caroteneemia, erythropoietic porphyria, hepatic form of infectious mononucleosis, etc.
Who to contact?
Treatment of the stagnation of bile
The principles on which the complex treatment of stagnation of bile is based: if it is possible to eliminate the cause - the etiological treatment, including surgical treatment; when the cause can not be eliminated - symptomatic therapy with the maximum possible impact on individual pathogenetic components.
If stagnation of bile in the gallbladder or liver did not cause obstruction of the ducts, then drugs based on ursodeoxycholic acid, which is part of the bile, are used. These include the hepatoprotective drug with choleretic (increasing the synthesis of bile) and choleretic actions Ursofalk (Ursohol, Cholacid, Ursosan, Ursoliv, Ukrliv, Holudexan and other trade names) in the form of capsules and suspension for oral administration. This means also reduces the production of cholesterol and its absorption in the small intestine, which reduces the likelihood of the formation of cholesterol-containing stones. Capsules and suspension are prescribed for 10-15-20 mg per kilogram of body weight per day (a specific dose is determined by the doctor); long-term treatment.
Ursofalk can not be used for cirrhosis of the liver, acute cholecystitis or cholangitis, with calcified stones in the gall bladder and its dyskinesia, as well as in case of obvious functional deficiency of the liver, pancreas or kidneys. And among the side effects of ursodeoxycholic acid, the appearance of pain in the upper abdominal region, mild diarrhea, and the formation of bile calcitans.
Almost always prescribed cholagogue for bile stagnation, such as Allochol, Hofitol (Artichol, Tsinarix), Holiver, Odeston (Gimecromon, Holestil, Holstamin forte, etc.). The most effective hepatoprotector recognized drug Ademethionin (Heptor, Heptral).
Allochol (consisting of dry bile, extracts of nettle and garlic and activated carbon) promotes the production of bile, so when acute forms of hepatitis, liver dysfunction and obstructive jaundice do not apply it. Allochol tablets are taken after meals - 2 tablets three times a day. In some, the drug can cause skin allergies and diarrhea.
Tablets (and solutions for oral administration and for parenteral administration) Hofitol contain an extract of leaves of a seed artichoke, which promotes bile, diuresis and cholesterol metabolism. The drug in the form of tablets is taken three times a day for 1-2 tablets (before meals), a solution - 2.5 ml (for children - 0.6-1.25 ml). Hofitol can cause hives; it is contraindicated to use with stones in the gallbladder, obstruction of the biliary tract and liver failure.
A cholagogue Holiver, in addition to the extract of artichoke, contains extracts of bile and turmeric, stimulating the synthesis of bile acids and the output of hepatic bile. The drug is also effective for constipation associated with intestinal dysbiosis, and flatulence. Contraindications are similar to Hofitol; standard dosage - 2-3 tablets 3 times a day (before or after meals).
Cholagogonnye tablets Odeston (based on 7-hydroxy-4-methylcoumarin) not only accelerate the circulation of bile, but also relieve spasms. It is recommended to take for 10-14 days one tablet (0.2 g) three times a day, half an hour before meals. Odeston is contraindicated in cases of ulcerative colitis and any gastrointestinal diseases with ulceration, bile duct obstruction, hemophilia; not applicable in the treatment of children. Side effects of the drug are manifested in the form of diarrhea, epigastric pain, increased formation of intestinal gases.
The drug Ademetionine (S-adenosyl-methionine) contributes to the normalization of liver function and metabolism. It is prescribed for 2-3 tablets a day; Contra-indications of the drug concern individual intolerance, use in the treatment of children and pregnant women (in I-II trimesters). A possible side effect is discomfort in the hypochondrium.
In addition, in the treatment of stagnation of bile used drug cholagogue collections of medicinal plants. For example, cholagogue No. 2 (flowers of the immortelle sand, yarrow herb, peppermint leaves, coriander seeds) or collection number 3 (flowers of calendula, tansy and chamomile and mint leaves). From the dry raw materials prepare a decoction - a tablespoon to a glass of water (boil for no more than 10 minutes and insist half an hour in a sealed container, strain and add boiled water to the original volume). Cholagogue should be used after consultation with a doctor; drink decoctions before meals twice a day - 100 ml each.
Choleretic properties also have a dog rose: you can prepare infusion from dry berries or take the remedy Holosas (according to a dessert spoon per day, children - half a teaspoon). Also, you should take vitamins A, C, D, E, K.
Homeopathy
Of homeopathic remedies for the treatment of bile stasis, Galsten (tablets for resorption under the tongue and droplets) and Gepar kompozitum (solution in ampoules for parenteral use) can be used.
Both preparations contain many components, but each contains a milk thistle (Silybum marianum) or a milk thistle (in the form of an extract of plant seeds). Among the active ingredients of milk thistle, the flavonolignan complex (silibinin, silibins, isosilbins, silicystrin, isosilicristin, silidianin and dihydroquercetin) has a particular benefit. Milk thistle also contains vitamin K and ω-6 fatty linoleic acid.
The preparation of Galsten stimulates the production of bile and activates its movement from the liver to the gallbladder and further, relieves spasms and inflammation. Doctors recommend taking this drug one tablet (under the tongue) twice a day; drops - 7-10 drops three times a day (in between meals). In the manual, adverse allergic reactions are noted, and in contraindications only increased sensitivity is indicated. However, Galstena contains Chelidonium majus, that is, celandine, and this plant is known to be poisonous (due to the presence of isoquinoline alkaloids) and can cause seizures, intestinal cramps, drooling and contractions of the uterine muscles.
Homeopathic preparation Gepar compositum consists of 24 active substances (one of them - rastoropsha). It is used by intramuscular or subcutaneous injection - one ampoule every 3-7 days for 3-6 weeks. Among the side effects marked hives and itching.
Operative treatment
To date - depending on the etiology and localization of stagnation of bile - surgical treatment includes such types of surgical intervention as:
- laparoscopic removal of stones in cholelithiasis and concrements of bile ducts (endoscopic lithoextraction);
- removal of a cyst or tumor that prevents the outflow of bile;
- the installation of stents in the bile ducts;
- balloon dilatation (dilatation) of the lumen of the bile ducts with their obstruction;
- drainage of the common bile duct (choledochostomy);
- expansion of the gallbladder or its ducts with stenting and the formation of biligidestive anastomoses;
- operations on sphincters of the gallbladder;
- removal of the gallbladder (cholecystectomy).
With biliary atresia (see Bile stasis in a child), the ducts in the liver are created surgically: the children of the first two months undergo a reconstructive operation (portoenterostomy), but liver transplantation may be required.
Alternative treatment
Among the variety of recipes for alternative treatment of this pathology, it is possible to identify the most appropriate tips:
- To consume within 1-1,5 months a mix of juices prepared at home - carrot, apple and beetroot (in equal proportions); should drink 150 ml of this juice (an hour after eating).
- Drink natural apple cider vinegar, adding a tablespoon to a cup of apple juice or water with lemon juice; there you can put a teaspoon of honey.
- Take a mummy dissolved in water (tablet 0.2 g per 500 ml) for two weeks; to drink all the amount per day (in several receptions, half an hour before meals). Between courses of application it is advised to do 5-7-day breaks. A full cycle of such mummies can last 3-5 months. True, the alternative recipe does not mention that at such volumes of use of this biostimulator can be diarrhea, increased heart rate and increased blood pressure.
Also, alternative treatment suggests using oats and preparing a decoction of it: a tablespoon of whole grains are poured into two glasses of water and cooked for about half an hour; drink 15-20 minutes before meals 3-4 times during the day (drink all the amount per day). However, it should be borne in mind that oats act as a laxative and reduces blood pressure.
Churm with bile stagnation will help to cope with diarrhea (for this it is recommended to prepare a decoction). In a persimmon, there is a lot of beta-carotene and vitamin C, as well as manganese - a cofactor for the synthesis of the antioxidant enzyme superoxide dismutase, which increases the stability of the mucous membranes. Other powerful antioxidants found in persimmons include lycopene and cryptoxanthin. But the pomegranate not only promotes hemopoiesis, but also has cholagogue properties; but this fruit helps constipation.
So, it is safer to use cholagogue grasses in bile stasis: a medicine douche, an immortelle sandy, a birdwort (a knotweed), a three-leaved watch, a naked herring, corn stigmas, a sweet clover, a paint duck, a mountain arnica. Decoctions are prepared and taken, as well as pharmacy cholagogue (see earlier).
 [28], [29], [30], [31], [32], [33]
[28], [29], [30], [31], [32], [33]
Diet in case of congestion of bile
The therapeutic diet for bile congestion is a diet number 5 and the introduction of certain restrictions and even prohibitions in the diet.
That is, fatty foods (animals and cooking fats, rich broths, fatty meat and fish, whole fat milk, cream, butter, sour cream, etc.) should be excluded; canned food and meat gastronomy with preservatives; semi-finished products and snacks; Refined sugar, fructose and sweets; bread and buns of white flour. See also - Diet for diseases of the gallbladder
Need to eat: fresh vegetables and fruits; Boiled, baked or stewed lean meat and poultry, seafood (source of protein); legumes (vegetable protein); healthy fats (walnuts, almonds, flaxseeds, pumpkin seeds).
Whole grains are required, such as brown rice, barley, oats, buckwheat; healthy oils with polyunsaturated fatty ω-3 and ω-6 acids: olive oil, sesame oil, linseed oil.
Exercises for bile congestion
Doctors warn: without movement, all processes in the body, including the secretion of bile, are violated. Therefore, gymnastics with bile stasis is needed, but it should not exacerbate pathology and intensify the symptoms.
It is recommended to walk (at least an hour a day), as well as such exercises with stagnation of bile, in which you do not need to do low inclines forward, sharp turns, strong flapping movements and jumps.
Remember the simple morning gymnastics: most of its elements are suitable for stagnation of bile. For example:
- Legs on the width of the shoulders, hands on the waist - alternately turn the body into the right and left sides.
- Legs on the width of the shoulders, hands behind the head - tilts to the right and left.
- In the same initial position - bend the right leg in the knee and reach for it with the elbow of the left hand, then bend the left leg and do the same with the elbow of the right hand.
- Lie on your back (legs straight, arms stretched along the body); on the inspiration, the right leg bends in the knee with the approach to the stomach, the exhalation assumes the initial position, the same is done by the other leg.
- Lying on the back, legs bend at the knees, put the palm of one hand on the stomach, take deep breaths with the diaphragm raised and protrude the abdominal wall; on an exhalation to involve a stomach or belly.
- Similar respiratory movements should be performed lying on the right and left sides.
By the way, the last exercise is a kind of internal self-massage of almost all organs located exactly where bile is stagnant. But a special therapeutic massage for bile congestion should be prescribed only by a doctor who has the results of examining the patient's gallbladder and liver.
More information of the treatment
Prevention
Prophylaxis of bile stasis is possible only with respect to some causes of its occurrence (alcohol, infection, helminths, tumors, unhealthy diet, lack of exercise). With congenital and genetically determined syndromes, as well as with endocrine and hormonal factors, pathologies of the hepatobiliary system do not exist.
Forecast
It is difficult to talk about the prognosis of stagnation of bile in this or that case, taking into account the individual characteristics of each patient, as well as all the complications, consequences and a whole complex of accompanying problems of general metabolism.


